TO THE EDITOR:
Reproductive health is an important aspect of health care for young adults with sickle cell disease (SCD).1 Along with SCD-specific reproductive health concerns (eg, genetic transmission2 and fertility impairment),3,4 studies suggest that their routine reproductive health care needs (eg, contraception)5,6 may not be met, increasing the risk of unplanned pregnancies and sexually transmitted infections (STIs), including human papilloma virus (HPV). These issues are particularly salient during transition to adult care because it is already high risk for those with SCD.7
Limited contraception use among transitioning young adults with SCD may be related to issues with access, insurance, self-management, and transition readiness.8 Another factor may be limited engagement with primary care because primary care providers (PCPs) are often tasked with providing this service, but PCP use among individuals with SCD declines with age.9 In 1 survey, 46% of adolescents and young adults with SCD reported their hematologist as their PCP.10
Understanding how sexual and reproductive health care is provided during transition to adult care and examining the incidences of high-risk reproductive health outcomes could inform the urgency of the problem and strategies to optimize practice. Thus, the aims of this study were to describe sexual activity, contraception use, STI testing and diagnosis, and HPV vaccination completion among young adults with SCD imminently transitioning to adult care. We also examined whether contraception counseling was provided (and by which provider type) and whether receipt of counseling was associated with having ≥1 STI.
Data were collected as part of a larger study of participants aged 18 to 21 years with SCD who had their final pediatric hematology visit at Nationwide Children’s Hospital (NCH) between 2015 and 2019. Participants’ entire NCH electronic health record was reviewed for (1) sociodemographic and medical characteristics (eg, sex and SCD genotype); (2) documentation by any provider on whether they were ever sexually active, had ever received contraception counseling, had ever used contraception (and what type), had ever had a documented pregnancy (females only), had ever received STI screening, and/or had ≥1 STI (and which one[s]); and (3) HPV vaccinations provided by Vaccines For Children providers.11 Finally, documentation of having an NCH PCP (because data from these visits could be accessed) and NCH PCP visit in the last year of pediatric hematology care were noted. This study was approved by the institutional review board at NCH and performed in accordance with the Declaration of Helsinki.
Three research staff collected data in parallel using a keyword approach (ie, contraception and STI) until they reached agreement; after which, only 1 staff member reviewed each participant’s chart. χ2 tests were conducted using SPSS (Version 28.0)12 to examine associations between receipt of contraception counseling and STI diagnosis.
We identified 53 eligible participants (53% female; mean age, 21 [standard deviation, 1.25]; 100% Black/African American, African, or multiple races; 53% hemoglobin [Hb] SS, 32% Hb SC, 9% Hb Sβ+, and 6% Hb Sβ0; 66% public, 30% private, and 4% other insurance). Of whom, 30 had an NCH PCP, and 7 of them had a PCP visit in the last year of pediatric hematology care.
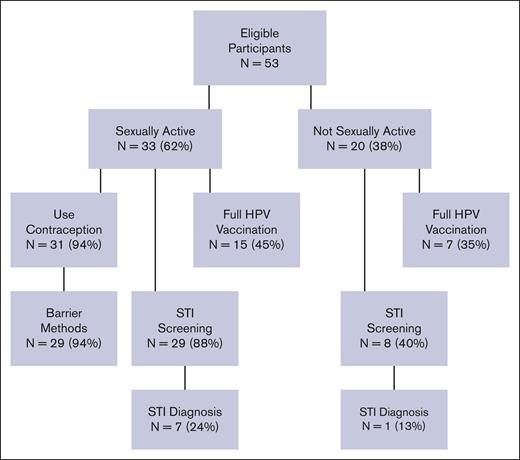
Of the 53 participants, 33 (62%) were documented to be sexually active (Figure 1), and 29 (55% of the whole sample) had documentation that they received contraception counseling. For participants with an NCH PCP and hematologist (n = 30), 10 (33%) had contraception counseling documented by their hematologist, 2 (13%) had it by the PCP and their hematologist, and 4 (25%) had it by some other provider. Three females (10%) had documented pregnancies.
Sexual activity, contraception use, and reproductive health services.
Of the 37 participants who had STI testing, 8 (22%) had 12 STIs diagnosed (chlamydia, gonorrhea, gardnerella, trichomoniasis, and/or herpes). Receipt of contraception counseling was not significantly associated with being diagnosed with ≥1 STI (P > .05). Only 22 participants (42%) received the full HPV series.
We found substantive gaps in routine reproductive health care received by transitioning young adults with SCD. Key study findings included multiple STIs and pregnancies, infrequent contraception counseling, and low HPV vaccination completion in a population of young adults with SCD who were largely sexually active. Although these findings may not substantively differ from nonchronically ill young adult populations,13 this population is also at risk of SCD-specific complications from these reproductive health outcomes and appears to be infrequently engaged in primary care in which preventative reproductive services are largely provided. Cumulatively, these findings suggest that (1) for some, pediatric hematology visits may be the only opportunity to receive or be linked with this care; and (2) hematologists need new strategies, such as implementing a colocated multidisciplinary clinic that shows preliminary benefit in providing care to children with SCD,14 to address reproductive health.
We found that most young adults who reported being sexually active at some point also had documentation that they used barrier contraception, but a relatively large number were still diagnosed with ≥1 STI. This is consistent with data suggesting that barrier methods are intermittently and/or imperfectly used by young adults15 and providers may need to specifically counsel about always using barrier contraception. These findings may also reflect the high rates of STIs among young non-Hispanic Black persons in the United States in general,16 and therefore, additional studies are needed to provide context to the problem of STIs in young adults with SCD.
Unplanned pregnancies could not be broadly assessed (because pregnancy intentions and pregnancy in male partners are not routinely documented), but 3 young women became pregnant while still in pediatric hematology care. Although our observed pregnancy rate is similar to women in their early 20s in general,13 these females also have SCD-specific pregnancy risks that the Centers for Disease Control and Prevention considers to outweigh their contraceptive risks.17 These findings combined with previous data showing high rates of unplanned, high-risk pregnancies,18,19 and limited understanding of the effectiveness of contraceptives20 highlight the importance of pediatric hematologists providing counseling on (1) the safest contraception options, (2) SCD-specific risks of pregnancy and contraception, and (3) the need for high-risk prenatal care if/when pregnancy occurs to their adolescent and young adult females with SCD.
Finally, we observed that less than half of our participants completed their HPV series. HPV is the most common STI,21 with well-known links to cancer.22 Previous studies have also demonstrated lower uptake of HPV vaccination among African Americans.23 Given the Healthy People 2030 goal to achieve 80% HPV vaccination completion,24 our findings reaffirm the need for targeted interventions, including increasing provider, patient, and family education, and access by potentially providing HPV immunizations during hematology visits to reduce cancer risk among this population that is already at higher risk of malignancy.25
Our study’s limitations include its retrospective nature and small sample size; the findings only reflect what was disclosed by young adults, documented by providers, and included in the NCH electronic health record. Nevertheless, the negative outcomes of low contraception counseling and use in this population, their well-established health care barriers, and their risks as they transition to adult care suggest that additional research to elucidate the problems and optimize this care is urgently needed. Multicenter prospective studies should be designed to confirm our findings and to inform the development of interventions to optimize outcomes, guidelines on which aspects of reproductive health care should be provided by whom, and pathways for referral to specialists.
Acknowledgment: This study was supported by the National Institutes of Health (K08CA237338, L.N. [principal investigator]).
Contribution: D.S., C.J.S., S.B., S.E.C, and L.N. designed the study; L.N. and S.E.C. were the principal investigators; C.J.S., S.B., and D.S., coordinated the project; D.S., S.B., C.J.S., S.M.L., and Z.A.C. abstracted data; C.J.S. analyzed the data; D.S., L.N., C.J.S., and S.E.C. contributed to writing the first draft of the manuscript; and all authors contributed to revision of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Susan Creary, Nationwide Children's Hospital, 700 Childrens Dr, Columbus, OH 43205; e-mail: susan.creary@nationwidechildrens.org.
References
Author notes
∗S.E.C. and L.N. contributed equally to this study.
Data are available upon request from the corresponding author, Susan E. Creary (susan.creary@nationwidechildrens.org).