TO THE EDITOR:
CD19 chimeric antigen receptor (CAR) T-cell therapy generates impressive responses in pediatric patients with relapsed/refractory B-cell acute lymphoblastic leukemia (r/r B-ALL).1-4 Although the focus of initial studies was bone marrow disease, signals of activity toward extramedullary disease (EMD) are emerging.5-8 In addition to the well-described central nervous system (CNS) and testicular involvement, EMD can also develop at other focal sites.918Fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) is the primary imaging modality used to assess EMD, but diagnostic criteria for non-CNS EMD are not standardized.10,11 Non-CNS EMD is not routinely monitored, and the true burden in patients with r/r B-ALL is unknown. Recent reports have demonstrated that although CAR T-cell therapy can generate complete responses (CRs) or partial responses at extramedullary sites, these responses may be delayed and discrepant from the marrow response.7,8,12 These works identified questions concerning CAR T cells for the treatment of extramedullary pediatric B-ALL, including the role of screening PET/CT, durability of response, and optimal integration of CAR T cells with other therapeutic modalities.
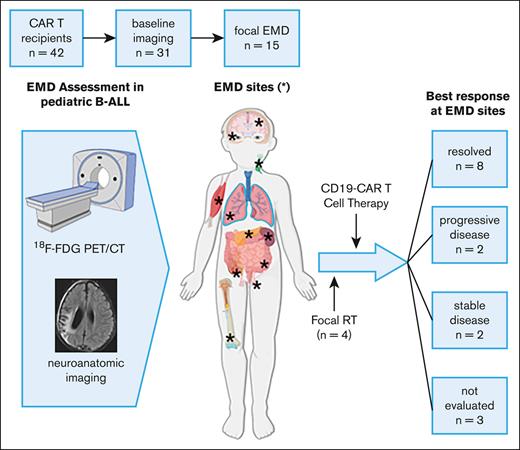
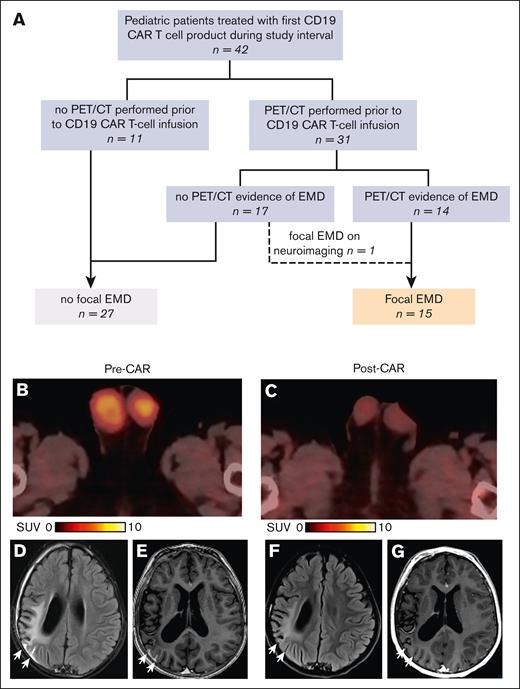
We performed an institutional review board–approved retrospective analysis of pediatric patients who received CD19 CAR T-cell therapy for r/r B-ALL at a single institution from November 2018 to December 2021 to detail the incidence of focal EMD, evaluate treatment response, and describe the incorporation of pre–CAR T-cell radiation therapy (RT) for select patients. Imaging physicians retrospectively re-evaluated all diagnostic imaging studies. Focal EMD was defined as FDG-avid visceral or soft tissue infiltration, mass lesions, or focal bony lesions; characteristic lesions on anatomical neuroimaging; and lymph nodes/aggregates >2 cm by anatomic imaging or >1 cm with FDG avidity without alternative clinical explanation. Of the 42 patients treated with CD19 CAR T-cell therapy, 31 underwent baseline PET/CT, obtained because of clinical suspicion or personal history of EMD (n = 9) or as part of screening (n = 22). PET/CT identified EMD in 14 of 31 patients (45%). One patient with a negative PET/CT result had focal CNS disease identified upon neuroimaging, forming a cohort of 15 patients with focal EMD (Figure 1A).
Identification of the cohort with EMD and representative imaging-based responses. (A) Identification of focal EMD among pediatric patients with r/r B-ALL treated with CD19 CAR T-cell therapy. (B-C) 18F-FDG PET/CT fusion images from UPN4 with testicular disease, with bilateral FDG-avid testicular enlargement before CAR T-cell infusion (B), which completely resolved after infusion (C). (D-G) Magnetic resonance imaging findings in UPN15 with focal CNS disease. Postcontrast axial T2 fluid-attenuated inversion recovery image (D) and 3D T1 image (E) through the level of the lateral ventricles obtained before CAR T-cell therapy demonstrated leptomeningeal enhancement along 2 of the right parietal sulci, suggesting leukemic infiltrate (D-E) (white arrows), which completely resolved after therapy on after contrast T2 fluid-attenuated inversion recovery image (F) and 3D T1 image (G) (arrows).
Identification of the cohort with EMD and representative imaging-based responses. (A) Identification of focal EMD among pediatric patients with r/r B-ALL treated with CD19 CAR T-cell therapy. (B-C) 18F-FDG PET/CT fusion images from UPN4 with testicular disease, with bilateral FDG-avid testicular enlargement before CAR T-cell infusion (B), which completely resolved after infusion (C). (D-G) Magnetic resonance imaging findings in UPN15 with focal CNS disease. Postcontrast axial T2 fluid-attenuated inversion recovery image (D) and 3D T1 image (E) through the level of the lateral ventricles obtained before CAR T-cell therapy demonstrated leptomeningeal enhancement along 2 of the right parietal sulci, suggesting leukemic infiltrate (D-E) (white arrows), which completely resolved after therapy on after contrast T2 fluid-attenuated inversion recovery image (F) and 3D T1 image (G) (arrows).
The characteristics of the 15 patients with EMD before CD19 CAR T-cell infusion are included in supplemental Table 1. The median age was 8 years (range, 2-22 years). This cohort represents a heavily pretreated population, including prior allogeneic hematopoietic cell transplant (HCT; n = 8) and prior antigen-directed therapy (n = 10). The patient with unique patient number 3 (UPN3) had prior CD19 CAR T-cell therapy without documented EMD and an interval allogeneic HCT. The most common focal EMD sites were bone (n = 7), soft tissue (n = 2), and the CNS (n = 2). Other sites included the orbit, soft tissue, viscera (lungs/pleura, spleen, bowel, and kidney), testes, and lymph nodes (Table 1). The relevance of focal bony disease is illustrated by UPN8, in which a directed aspirate of an FDG-avid right humerus lesion revealed 54% leukemic blasts, whereas a simultaneous bone marrow aspirate at the iliac crest revealed minimal disease detectable only by next-generation sequencing (NGS). Five patients (33%) had multiple sites of focal EMD. Two patients also had active disease in the cerebrospinal fluid at their last evaluation preceding CAR T-cell infusion (CNS2 = 1 and CNS3 = 1).13 Most patients (n = 14) had concurrent bone marrow involvement, including 8 with ≥5% marrow blasts, 5 with detectable minimal residual disease by flow cytometry or NGS, and 1 with aplastic marrow with peripheral blasts (Table 1). Several patients had leukemia with high-risk genetic features,14 including 4 with KMT2A rearrangements (2 diagnosed as infants).
Characteristics of patients with EMD
| UPN . | Preinfusion disease evaluation . | Postinfusion response . | Notable genetics . | Clinical outcome† (mo to event/last contact) . | |||
|---|---|---|---|---|---|---|---|
| Focal EMD . | Bone marrow∗ . | CSF . | Focal EMD . | Bone marrow∗ . | |||
| 1‡ | Soft tissue | 0.06% | CNS1 | Progressive | CR and MRD neg | IKZF1 truncation and hyperdiploid | EMD progression (1) |
| 2‡ | Orbit and focal bone | NGS pos | CNS1 | Mixed (1 mo), resolved by 3 mo | CR and MRD neg | KMT2A::RELA | EMD relapse at a new site (5) |
| 3 | Pleura | 32% | CNS1 | NE | CR and NGS pos | NF1 and RASGRP4 alterations | Consolidative HCT (1) |
| 4 | Testicular and lymph nodes | 33% | CNS1 | Resolved | CR and MRD neg | KMT2A::MLLT3 | Ongoing BCA and remission (15) |
| 5 | Focal bone | 34% | CNS1 | Resolved | CR and MRD neg | None detected | Consolidative HCT (3) |
| 6 | Pancreas, kidney, and bowel | 45% | CNS1 | NE | Progression | Hypodiploid | Marrow nonresponse (1) |
| 7 | Focal bone | NGS pos | CNS1 | Stable | CR and MRD neg | None detected | Consolidative HCT (2) |
| 8‡ | Focal bone | NGS pos | CNS1 | Resolved | CR and MRD neg | KMT2A::MLLT10 | Repeat CD19 CAR infusion for the loss of BCA (4) |
| 9 | Focal bone | Aplastic, PB 2% | CNS1 | Resolved | CR and MRD neg | None detected | Ongoing BCA and remission (4) |
| 10 | Testicular | None detected | CNS1 | Progressive | CR and MRD neg§ | Hyperdiploid and complex karyotype | EMD progression (1) |
| 11 | Spleen, bowel, pancreas, and soft tissue | 98% | CNS2 | Stable | Progression | KMT2A::AFF1 | Marrow progression (1) |
| 12 | Lung | 95% | CNS3 | NE | Progression | TSC1 truncation, IL7R, and SH2B3 (Ph-like) | Marrow progression (1) |
| 13 | Focal bone | 6.8% | CNS1 | Improved (1 mo), resolved by 2 mo | CR and MRD neg | None detected | Consolidative HCT (3) |
| 14‡ | Focal bone and focal CNS | 0.08% | CNS1 | Bone: NE; CNS: resolved | CR and MRD neg | CREBBP truncation and hyperdiploid | Ongoing BCA and remission (2) |
| 15 | Focal CNS | 5% | CNS1 | Improved (1 mo) and resolved by 2 mo | CR and MRD pos | ETV6::ETV5 and hyperdiploid | Consolidative HCT (2) |
| UPN . | Preinfusion disease evaluation . | Postinfusion response . | Notable genetics . | Clinical outcome† (mo to event/last contact) . | |||
|---|---|---|---|---|---|---|---|
| Focal EMD . | Bone marrow∗ . | CSF . | Focal EMD . | Bone marrow∗ . | |||
| 1‡ | Soft tissue | 0.06% | CNS1 | Progressive | CR and MRD neg | IKZF1 truncation and hyperdiploid | EMD progression (1) |
| 2‡ | Orbit and focal bone | NGS pos | CNS1 | Mixed (1 mo), resolved by 3 mo | CR and MRD neg | KMT2A::RELA | EMD relapse at a new site (5) |
| 3 | Pleura | 32% | CNS1 | NE | CR and NGS pos | NF1 and RASGRP4 alterations | Consolidative HCT (1) |
| 4 | Testicular and lymph nodes | 33% | CNS1 | Resolved | CR and MRD neg | KMT2A::MLLT3 | Ongoing BCA and remission (15) |
| 5 | Focal bone | 34% | CNS1 | Resolved | CR and MRD neg | None detected | Consolidative HCT (3) |
| 6 | Pancreas, kidney, and bowel | 45% | CNS1 | NE | Progression | Hypodiploid | Marrow nonresponse (1) |
| 7 | Focal bone | NGS pos | CNS1 | Stable | CR and MRD neg | None detected | Consolidative HCT (2) |
| 8‡ | Focal bone | NGS pos | CNS1 | Resolved | CR and MRD neg | KMT2A::MLLT10 | Repeat CD19 CAR infusion for the loss of BCA (4) |
| 9 | Focal bone | Aplastic, PB 2% | CNS1 | Resolved | CR and MRD neg | None detected | Ongoing BCA and remission (4) |
| 10 | Testicular | None detected | CNS1 | Progressive | CR and MRD neg§ | Hyperdiploid and complex karyotype | EMD progression (1) |
| 11 | Spleen, bowel, pancreas, and soft tissue | 98% | CNS2 | Stable | Progression | KMT2A::AFF1 | Marrow progression (1) |
| 12 | Lung | 95% | CNS3 | NE | Progression | TSC1 truncation, IL7R, and SH2B3 (Ph-like) | Marrow progression (1) |
| 13 | Focal bone | 6.8% | CNS1 | Improved (1 mo), resolved by 2 mo | CR and MRD neg | None detected | Consolidative HCT (3) |
| 14‡ | Focal bone and focal CNS | 0.08% | CNS1 | Bone: NE; CNS: resolved | CR and MRD neg | CREBBP truncation and hyperdiploid | Ongoing BCA and remission (2) |
| 15 | Focal CNS | 5% | CNS1 | Improved (1 mo) and resolved by 2 mo | CR and MRD pos | ETV6::ETV5 and hyperdiploid | Consolidative HCT (2) |
BCA, B cell aplasia; CR, complete response (<5% marrow blasts); CSF, cerebrospinal fluid; HCT, hematopoietic cell transplant; MRD, minimal residual disease by flow cytometry (0.01-5% blasts); NE, not evaluated; neg, negative result; NGS, disease detected only by next-generation sequencing (<0.01%); PB, peripheral blood; pos, positive result.
Disease burden detected by flow cytometry, unless otherwise indicated (morphology for UPN11).
First occurrence of relapse, additional systemic disease–directed therapy including consolidative HCT, or nonrelapse mortality.
Received focal RT before CAR T-cell infusion.
No detectable marrow disease before infusion.
Patients received tisagenlecleucel (n = 6) or an investigational CD19 CAR T-cell product (n = 9) after fludarabine/cyclophosphamide lymphodepletion.4,15,16 The rates of cytokine release syndrome and neurotoxicity observed were as expected (supplemental Table 1).17 Most patients underwent a disease response assessment 4 weeks after CAR T-cell infusion. Reassessment of EMD sites was clinically guided based on known prior sites of EMD, with the response defined as progressive, mixed, stable, improved, or resolved (supplemental Table 2). The best responses at focal EMD sites included resolved (n = 8), stable (n = 2), progressive (n = 2), and not evaluated (n = 3). UPN14 was partially evaluated because focal non-CNS EMD was established only retrospectively (Table 1). Figure 1B displays images from UPN4 with bilateral testicular involvement before infusion. He developed testicular and scrotal swelling on day +4 after infusion with concurrent grade 1 cytokine release syndrome and subsequent CR at all disease sites (Figure 1C). Representative brain magnetic resonance imaging from UPN15 demonstrate focal CNS lesions (Figure 1D-E), with resolution after treatment (Figure 1F-G). Four patients received RT for EMD sites as part of bridging therapy, with a target treatment dose of 24 Gy administered over 12 to 16 fractions (Table 1). No additional RT-related toxicities were observed. For example, UPN14 presented with acute vision loss due to EMD involving the optic nerve. After emergent RT and subsequent CD19 CAR T-cell infusion, the patient achieved a CR and remains in remission.
Of the 14 patients with focal EMD and simultaneous detectable marrow disease, 11 (79%) were in marrow CR after CAR T-cell treatment (Table 1). Response at focal EMD sites lagged marrow response in 3 patients, with mixed (n = 1) or improved (n = 2) response at 1 month after infusion, and CR by 2 to 3 months without additional therapy. Thus, responses between compartments were not always congruent. Of the 10 patients with initial response to CD19 CAR T-cell therapy at all evaluated disease sites, 5 underwent consolidative HCT, 1 received CAR T-cell reinfusion for early loss of B-cell aplasia, 3 have ongoing remission/B-cell aplasia, and 1 had CD19+ relapse at a new EMD site. With a median follow-up of 6 months (range, 1-31), 9 patients (60%) are alive, with 4 disease-related and 2 treatment-related deaths.
Our study demonstrates that EMD is present in almost half of pediatric patients with r/r B-ALL referred for CD19 CAR T-cell therapy when evaluated by PET/CT, with many sites identified by imaging without clinical symptoms. Considerations of PET/CT screening must balance the potential benefit of identifying clinically significant focal disease for comprehensive response monitoring with the risks of false-positive findings and associated costs.18 Performing rigorous analyses of focal EMD across cohorts to further understand the clinical impact would require standardized assessment and definitions for nonclassical EMD sites, which are lacking in current practice.13
Our experience highlights CD19 CAR T-cell activity at EMD sites while also demonstrating examples of nonresponse at EMD sites despite clearance of marrow disease. Although growing evidence supports the activity of CD19 CAR T cells against EMD, mixed responses suggest that CAR T-cell activity at EMD sites is limited compared with that in the bone marrow.6,7,12,19 Limited activity is likely multifactorial, including impaired CAR T-cell homing to and penetration of EMD sites and the impact of the local microenvironment, mirroring experiences in lymphoma and solid tumors.20,21 CAR T-cell infusion after RT directed at EMD sites is a promising paradigm. However, in this context, it is challenging to isolate the independent impact of RT vs CAR T-cell therapy. Extrapolating from the lymphoma experience, RT may prime patients for response to immunotherapies.22-24 This approach was feasible in our cohort, and we did not observe any additional acute toxicities related to preceding RT exposure.
In summary, pediatric patients with r/r B-ALL have a high burden of focal EMD, which demonstrates a lower response rate to CD19 CAR T-cell therapy than marrow disease. Prospective systematic evaluations of EMD using advanced imaging techniques will be critical in further elucidating the role of CAR T-cell therapy for pediatric patients with r/r B-ALL and EMD. As sequential immunotherapies, HCT, and novel targeted treatments may provide increased selective pressure driving an EMD phenotype in patients with r/r B-ALL, a heightened level of suspicion will be required to identify EMD and evaluate response.
Acknowledgments: The authors thank the staff of their clinical care teams for providing excellent patient care. The authors thank the patients whose outcomes are reported in this work and their families. The visual abstract was designed with BioRender.com, for which the authors have a license.
This work was supported by National Institutes of Health/National Cancer Institute grants P30CA021765 and 5P30CA021765-42, the American Society of Hematology (A.C.T.), the American Society of Transplantation and Cellular Therapy (A.C.T. and R.E.), and the American Lebanese Syrian Associated Charities.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contribution: R.E., B.M.T., S.G., and A.C.T. designed the study; R.E. and A.C.T. collected data; B.L.S. and A.K.B. performed expert review of diagnostic images and provided representative images; R.E., B.M.T., S.G., S.N., C.C., H.I., J.T.L., and A.C.T. contributed to data analysis; R.E. and A.C.T. drafted the manuscript; and all authors reviewed and edited the manuscript.
Conflict-of-interest disclosure: S.G. is a consultant of TESSA Therapeutics; is a member of the data and safety monitoring board of Immatics; serves on the scientific advisory board of Be Biopharma; and has received honoraria from Tidal, Catamaran Bio, and Sanofi within the past 2 years. S.G. and R.E. have patents/patent applications in the fields of T-cell and gene therapy for cancer. The remaining authors declare no competing financial interests.
Correspondence: Rebecca Epperly, Bone Marrow Transplantation, St. Jude Children’s Research Hospital, 262 Danny Thomas Pl, Memphis, TN 38105; e-mail: rebecca.epperly@stjude.org; and Aimee C. Talleur, Bone Marrow Transplantation, St. Jude Children’s Research Hospital, 262 Danny Thomas Pl, Memphis, TN 38105; e-mail: aimee.talleur@stjude.org.
References
Author notes
Data are available on request from the corresponding authors, Rebecca Epperly (rebecca.epperly@stjude.org) and Aimee C. Talleur (aimee.talleur@stjude.org).
The full-text version of this article contains a data supplement.