TO THE EDITOR:
Although initially effective, patients frequently relapse from B-cell maturation antigen (BCMA)–targeting chimeric antigen receptor (CAR) T-cell therapy and survival after relapse is limited.1-4 Part of relapses after CAR T-cell therapy can be attributed to the heterogeneity of multiple myeloma (MM).5 BCMA is often nonuniformly expressed within tumors,6 allowing for CAR-mediated immunoediting and outgrowth of BCMAlow or BCMA(–/–) MM cells.7-9 The efficacy of BCMA-targeting CAR T cells may further be compromised by BCMA shedding and trogocytosis.10,11 As an attempt to design a potentially curative approach, strategies targeting additional MM antigens are currently being developed.12 Other surface antigens targetable by CARs include SLAMF713 and CD38,14 but their expression on non–B-cell lineage cells potentially compromises their safety profile. G protein–coupled receptor class C group 5 member D (GPRC5D) is an alternative surface antigen with a safe expression profile, and GPRC5D-targeting CAR T cells have recently entered the clinical stage.15,16 Although GRPC5D-targeting CAR T cells induced clinical responses, most patients eventually relapsed. Similar to BCMA-targeting CAR T-cell therapy, relapse was associated with the loss of GPRC5D expression.
Alternatively to CAR engineering, T cells can be engineered to express a transgenic T-cell receptor (eTCR-T cells). In contrast to CARs, TCRs recognize protein-derived peptides presented in the context of HLA. Importantly, this includes intracellular protein–derived antigens, which broadens the pool of safely targetable antigens.17 This also provides the opportunity to target antigens that are uniformly expressed and essential for the survival of MM, such as BOB1 (alternative names POU2AF1 and OCA-B).18,19 However, MM cells can evade TCR-mediated targeting through defects in the antigen presentation machinery.20 Because CAR-mediated recognition is typically MHC-independent, MM cells with acquired defects in antigen presentation can still be targeted by CAR T cells.
Here, we propose multi-antigen targeting of MM using CAR- and TCR-engineered T cells. We hypothesized that simultaneous targeting via 2 independent modes of antigen recognition would reduce the occurrence of immune escape, potentially inducing long-lasting remissions after cellular therapy for MM.
The generation of TCR- and CAR-engineered T cells, fluorescence-activated cell sorting–based quantification of primary MM killing, CRISPR/Cas9 engineering, and murine xenograft experiments were performed analogously to previously published protocols17,19,21 (refer to supplemental Methods).
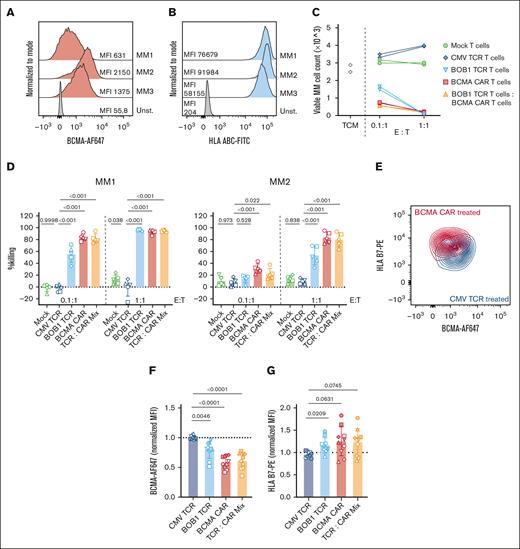
First, we tested how primary MM cells respond to T cells transduced to express an HLA-B∗07:02 restricted TCR targeting a BOB1 derived peptide or to CAR T cells targeting BCMA.19 Three bone marrow samples from patients with MM were analyzed for expression of BCMA and HLA on MM cells. Expression of BCMA varied considerably between samples (Figure 1A), whereas expression of HLA-ABC was uniform and high on all 3 samples (Figure 1B). HLA-B∗07:02-positive MM samples MM1 and MM2 were then subjected to overnight recognition in vitro by BCMA-CAR T cells, BOB1-TCR T cells, or a combination thereof (Figure 1C-D). Both BCMA-CAR T cells and BOB1-TCR T cells induced efficient lysis of primary MM. Lysis by BCMA-CAR T cells appeared to be more efficient than lysis by BOB1-TCR T cells, which is consistent with earlier findings reporting stronger initial effector functions for CAR T cells.21 Killing induced by the combination of eTCR- and CAR T cells reached comparable levels to that induced by BCMA-CAR T cells alone. Interestingly, BCMA expression in residual MM cells decreased after exposure to BCMA-targeting CAR T cells (Figure 1E), but also after exposure to BOB1-TCR T cells (Figure 1F). Conversely, HLA-B∗07:02 expression on MM cells was tendentially increased after exposure to eTCR- and CAR T cells (Figure 1G). HLA-B∗07:02-negative MM material 3 was only recognized by BCMA-CAR T cells (supplemental Figure 1A), and recognition by CAR T cells again was associated with a decrease in BCMA expression (supplemental Figure 1B).
Primary multiple myeloma cells can be targeted efficiently by both eTCR- and CAR T cells. (A-B) Bone marrow mononuclear cells derived from 3 patients with MM were thawed and assessed by flow cytometry. MM cells were identified as CD3–CD19–CD45neg/lowCD38hiCD56hi/low. (A) Expression of BCMA vs unstained. (B) Expression of HLA-ABC vs unstained. (C-D) Fifty thousand bone marrow mononuclear cells from HLA-B7–positive MM materials 1 and 2 were incubated with indicated T cells derived from 2 donors at designated effector-to-target ratio (E:T) ratios (5000 T cells or 50 000 T cells; for combination of BOB1-TCR T cells and BCMA-CAR T cells 2500 or 25 000 of each T-cell population were added together). (C) Representative data showing counts of viable MM cells of MM material MM1 after overnight coculture with indicated T cells derived from 1 donor in technical duplicates. Viable MM cells were identified as sytox-blue–, CD3–CD19–CD45lowCD38hiCD56hi/low acquired in isovolumetric flow cytometry measurements. (D) Summary of killing data on MM materials MM1 (left) and MM2 (right) subjected to recognition by T-cell products generated from 5 different donors (indicated by symbols). Statistics depict repeated measures 2-way ANOVA (paired for donors, Dunnett post hoc test). (E) Representative data showing expression of BMCA and HLA-B∗07:02 on primary MM after exposure to BCMA-CAR T cells or CMV-TCR T cells in an E:T ratio of 0.1:1. (F-G) normalized gMFIs of BCMA (AF647) (F) and HLA B7 (PE) (G) on surviving MM cells after coculture with indicated T cells in an E:T ratio of 0.1:1. The symbol shapes are analogous to those in panel E. Pooled data of both MM materials as indicated by filled or open symbols (open: MM1, closed: MM2). Statistics in panels F-G depict repeated measures 1-way ANOVA (paired for donors, Dunnett post hoc test). MM, multiple myeloma; ANOVA, analysis of variance; gMFI, geometric mean fluorescence intensity.
Primary multiple myeloma cells can be targeted efficiently by both eTCR- and CAR T cells. (A-B) Bone marrow mononuclear cells derived from 3 patients with MM were thawed and assessed by flow cytometry. MM cells were identified as CD3–CD19–CD45neg/lowCD38hiCD56hi/low. (A) Expression of BCMA vs unstained. (B) Expression of HLA-ABC vs unstained. (C-D) Fifty thousand bone marrow mononuclear cells from HLA-B7–positive MM materials 1 and 2 were incubated with indicated T cells derived from 2 donors at designated effector-to-target ratio (E:T) ratios (5000 T cells or 50 000 T cells; for combination of BOB1-TCR T cells and BCMA-CAR T cells 2500 or 25 000 of each T-cell population were added together). (C) Representative data showing counts of viable MM cells of MM material MM1 after overnight coculture with indicated T cells derived from 1 donor in technical duplicates. Viable MM cells were identified as sytox-blue–, CD3–CD19–CD45lowCD38hiCD56hi/low acquired in isovolumetric flow cytometry measurements. (D) Summary of killing data on MM materials MM1 (left) and MM2 (right) subjected to recognition by T-cell products generated from 5 different donors (indicated by symbols). Statistics depict repeated measures 2-way ANOVA (paired for donors, Dunnett post hoc test). (E) Representative data showing expression of BMCA and HLA-B∗07:02 on primary MM after exposure to BCMA-CAR T cells or CMV-TCR T cells in an E:T ratio of 0.1:1. (F-G) normalized gMFIs of BCMA (AF647) (F) and HLA B7 (PE) (G) on surviving MM cells after coculture with indicated T cells in an E:T ratio of 0.1:1. The symbol shapes are analogous to those in panel E. Pooled data of both MM materials as indicated by filled or open symbols (open: MM1, closed: MM2). Statistics in panels F-G depict repeated measures 1-way ANOVA (paired for donors, Dunnett post hoc test). MM, multiple myeloma; ANOVA, analysis of variance; gMFI, geometric mean fluorescence intensity.
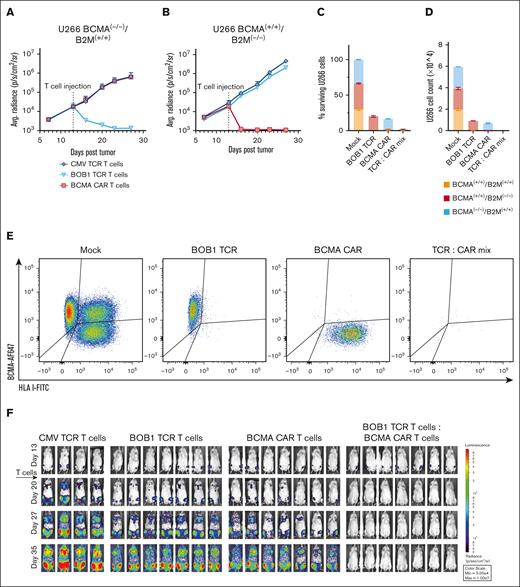
The study of the long-term behavior of primary MM in response to cellular therapy in vitro is challenging due to the limited viability of primary MM ex vivo. To study evasion of MM cells from CAR and eTCR-T cells in extended in vitro cocultures and in vivo, we established an immune-escape model based on the MM cell line U266. Using CRISPR/Cas9 engineering, we generated U266 cells that were either refractory to BCMA-CAR T-cell therapy or refractory to eTCR T-cell therapy by knocking out BCMA or β2-microglobulin (B2M), respectively (supplemental Figure 2). Sorted U266-BCMA(–/–) or U266-B2M(–/–) were engrafted to NSG mice and treated 2 weeks later with BCMA-CAR T cells, BOB1-TCR T cells, or control T cells. Importantly, BOB1-TCR T cells induced complete remissions in mice bearing U266-BCMA(–/–), whereas BCMA-CAR T cells failed to induce any antitumor response compared with control T cells (Figure 2A). Conversely, BCMA-CAR T cells completely cleared tumor from U266-B2M-(–/–) bearing mice that were refractory to eTCR T-cell therapy (Figure 2B). To emulate antigen escape of a heterogeneous tumor population after cellular therapy, we mixed U266-wildtype (U266-WT) cells at a 1:1:1 ratio with U266-BCMA(–/–) and U266-B2M(–/–). This heterogeneous MM population was then subjected in vitro to recognition by BOB1-TCR T cells, BCMA-CAR T cells, or a combination of the 2. After overnight coculture at an effector-to-target ratio of 1:1, only “immune escaped” U266 cells survived after single-antigen targeting, whereas all U266 cells were killed after double-antigen targeting (Figure 2C). We observed some degree of bystander killing after single-antigen targeting, as indicated by reduced numbers of BCMA- or HLA-negative cells compared with control T-cell–treated MM cells. However, after long-term coculture, immune-escaped tumor cells were able to expand despite the continuous presence of T cells, indicating insufficient levels of bystander killing to control tumor growth (Figure 2D-E). Lastly, we engrafted the mix of U266-WT, U266-BCMA(–/–), and U266-B2M(–/–) into NSG mice. Single-antigen targeting using only BOB1-TCR T cells or only BCMA-CAR T cells induced a temporary delay in tumor growth, but tumor growth progressed a few days after treatment (Figure 2F-G). In contrast, double-antigen targeting durably decreased the tumor load to below the detection level. At the termination of the experiment, no MM cells were detected in the bone marrow of dual-treated mice, whereas MM cells were still present in mice that received single-antigen targeting (Figure 2H). Phenotypic analysis revealed that all the remaining U266 in the bone marrow of mice treated with BOB1-TCR-T cells lacked HLA class I expression, whereas all the remaining U266 in mice treated with BCMA-CAR T cells were negative for BCMA, recapitulating immune escape after cellular therapy (Figure 2I).
Effective targeting of a heterogeneous tumor population in vitro and in vivo requires multi antigen targeting. (A-B) NSG mice were inoculated IV with 2 × 106 U266-BCMA(–/–) or U266-B2M(–/–) expressing Luc2 (Addgene #72486). Tumor cells were allowed to engraft for 2 weeks before IV treatment with indicated T-cell populations (6 × 106 purified eTCR-T cells or CAR T cells per mouse). Tumor signal was regularly monitored using IVIS imaging after subcutaneous injection of luciferin. For IVIS images, refer to supplemental Figure 2D-E. (C) Overnight killing of heterogeneous U266 cells by the indicated T-cell populations in vitro. (D) Survival and phenotype of heterogeneous U266 cells after 7 days of coculture with indicated T-cell populations. (E) Fluorescence-activated cell sorting plots of heterogeneous U266 showing prevalence of U266-WT, U266-BCMA(–/–), and U266-B2M(–/–) 7 days after coculture with indicated T cells. (C-E) Representative data showing technical duplicates from 1 of 3 independent experiments using T cells derived from independent donors. (F-G) NSG mice were inoculated IV with a 1:1:1 mix of U266 WT, U266-BCMA(–/–), and U266-B2M(–/–) (2 × 106 cells in total) expressing Luc2. After 2 weeks, mice were IV treated with indicated T-cell populations (6 × 106 purified eTCR-T cells or CAR T cells per mouse; in the combination group 3 × 106 BCMA-CAR T cells were coinjected with 3 × 106 BOB1-TCR T cells); n = 4 for CMV-TCR T-cell treatment group; n = 7 for other treatment T-cell groups. (H) Mice were euthanized and bone marrow was extracted for fluorescence-activated cell sorting analysis for presence of U266 cells. The percentage of U266 in the bone marrow indicates 100% × (n[Luc2-tdTom+])/(n[mCD45+ OR huCD45+]). Statistics depict 1-way ANOVA comparing double-treated mice to BOB1 TCR or BCMA CAR single-treated mice (Fisher's LSD test). (I) Phenotyping of U266 cells detected in the bone marrow of euthanized mice. IVIS, in vivo imaging system; ANOVA, analysis of variance; LSD, least significant difference.
Effective targeting of a heterogeneous tumor population in vitro and in vivo requires multi antigen targeting. (A-B) NSG mice were inoculated IV with 2 × 106 U266-BCMA(–/–) or U266-B2M(–/–) expressing Luc2 (Addgene #72486). Tumor cells were allowed to engraft for 2 weeks before IV treatment with indicated T-cell populations (6 × 106 purified eTCR-T cells or CAR T cells per mouse). Tumor signal was regularly monitored using IVIS imaging after subcutaneous injection of luciferin. For IVIS images, refer to supplemental Figure 2D-E. (C) Overnight killing of heterogeneous U266 cells by the indicated T-cell populations in vitro. (D) Survival and phenotype of heterogeneous U266 cells after 7 days of coculture with indicated T-cell populations. (E) Fluorescence-activated cell sorting plots of heterogeneous U266 showing prevalence of U266-WT, U266-BCMA(–/–), and U266-B2M(–/–) 7 days after coculture with indicated T cells. (C-E) Representative data showing technical duplicates from 1 of 3 independent experiments using T cells derived from independent donors. (F-G) NSG mice were inoculated IV with a 1:1:1 mix of U266 WT, U266-BCMA(–/–), and U266-B2M(–/–) (2 × 106 cells in total) expressing Luc2. After 2 weeks, mice were IV treated with indicated T-cell populations (6 × 106 purified eTCR-T cells or CAR T cells per mouse; in the combination group 3 × 106 BCMA-CAR T cells were coinjected with 3 × 106 BOB1-TCR T cells); n = 4 for CMV-TCR T-cell treatment group; n = 7 for other treatment T-cell groups. (H) Mice were euthanized and bone marrow was extracted for fluorescence-activated cell sorting analysis for presence of U266 cells. The percentage of U266 in the bone marrow indicates 100% × (n[Luc2-tdTom+])/(n[mCD45+ OR huCD45+]). Statistics depict 1-way ANOVA comparing double-treated mice to BOB1 TCR or BCMA CAR single-treated mice (Fisher's LSD test). (I) Phenotyping of U266 cells detected in the bone marrow of euthanized mice. IVIS, in vivo imaging system; ANOVA, analysis of variance; LSD, least significant difference.
In summary, we developed a 2-sided model for the outgrowth of immune-escaped tumor cells after CAR T-cell or eTCR T-cell treatment. Single-antigen targeting led to immune escape and outgrowth of tumor cells in vitro and in vivo, whereas dual-antigen targeting completely cleared heterogeneous tumor-cell populations. Interestingly, in overnight assays using primary MM cells, we observed a decrease in BCMA surface expression after exposure to BCMA-CAR T cells, whereas expression of HLA increased. These observations support the notion that antigen-specific target cell recognition mechanisms by CAR and eTCR T cells might be complementary and that this could be exploited for multi-antigen targeting strategies.
Preventing immune escape is of particular concern in MM, a heterogeneous disease prone to relapse after cellular therapy. We advocate dual-route targeting using HLA-dependent and HLA-independent recognition modes as a strategy to prevent immune escape after cellular therapy. Although from a manufacturing point of view, it might be attractive to design a single expression vector encoding both the tumor-targeting CAR and TCR, functional data on such a product are to date only limitedly available and might negatively impact either CAR or eTCR function.22,23 Alternatively, as separate products, CAR T cells can be combined with different TCRs directed to different antigens and restriction elements depending on patient characteristics.17,24 This is especially attractive for off-the-shelf strategies using engineered third party T cells, a strategy recently confirmed to be effective and feasible for BCMA-targeting CAR T cells.25
Acknowledgments: The authors acknowledge the fluorescence-activated cell sorting core facility and animal facility of the Leiden University Medical Center.
This project received funding from the H2020 Marie Skłodowska-Curie Actions (721358). The BOB1 4G11 B7 T-cell receptor is licensed to Miltenyi Biotec.
Contribution: T.L.A.W. conceptualized the study, designed and performed in vitro and in vivo experiments, analyzed and visualized the data, and wrote the manuscript; M.H.M. conceptualized the study, performed in vivo experiments, visualized data, and critically revised the manuscript; D.F.G.R. performed in vivo experiments; K.B., A.K.W., and R.S.H. performed in vitro experiments; J.H.F.F. critically revised the manuscript and jointly supervised the study; and M.H.M.H. conceptualized the study, critically revised the manuscript, supervised the study, and provided funding.
Conflict-of-interest disclosure: M.H.M.H. received research funding from Miltenyi Biotec. The remaining authors declare no competing financial interests.
Correspondence: Tassilo L. A. Wachsmann, Department of Hematology, Leiden University Medical Center, Albinusdreef 2, 2333ZA Leiden, The Netherlands; e-mail: t.l.a.wachsmann@lumc.nl; and Mirjam H. M. Heemskerk, Department of Hematology, Leiden University Medical Center, Albinusdreef 2, 2333ZA Leiden, The Netherlands; e-mail: m.h.m.heemskerk@lumc.nl.
References
Author notes
Data supporting the findings of this study are available upon reasonable request from the corresponding authors, Tassilo L. A. Wachsmann (t.l.a.wachsmann@lumc.nl) and Mirjam H. M. Heemskerk (m.h.m.heemskerk@lumc.nl).
The full-text version of this article contains a data supplement.

![Effective targeting of a heterogeneous tumor population in vitro and in vivo requires multi antigen targeting. (A-B) NSG mice were inoculated IV with 2 × 106 U266-BCMA(–/–) or U266-B2M(–/–) expressing Luc2 (Addgene #72486). Tumor cells were allowed to engraft for 2 weeks before IV treatment with indicated T-cell populations (6 × 106 purified eTCR-T cells or CAR T cells per mouse). Tumor signal was regularly monitored using IVIS imaging after subcutaneous injection of luciferin. For IVIS images, refer to supplemental Figure 2D-E. (C) Overnight killing of heterogeneous U266 cells by the indicated T-cell populations in vitro. (D) Survival and phenotype of heterogeneous U266 cells after 7 days of coculture with indicated T-cell populations. (E) Fluorescence-activated cell sorting plots of heterogeneous U266 showing prevalence of U266-WT, U266-BCMA(–/–), and U266-B2M(–/–) 7 days after coculture with indicated T cells. (C-E) Representative data showing technical duplicates from 1 of 3 independent experiments using T cells derived from independent donors. (F-G) NSG mice were inoculated IV with a 1:1:1 mix of U266 WT, U266-BCMA(–/–), and U266-B2M(–/–) (2 × 106 cells in total) expressing Luc2. After 2 weeks, mice were IV treated with indicated T-cell populations (6 × 106 purified eTCR-T cells or CAR T cells per mouse; in the combination group 3 × 106 BCMA-CAR T cells were coinjected with 3 × 106 BOB1-TCR T cells); n = 4 for CMV-TCR T-cell treatment group; n = 7 for other treatment T-cell groups. (H) Mice were euthanized and bone marrow was extracted for fluorescence-activated cell sorting analysis for presence of U266 cells. The percentage of U266 in the bone marrow indicates 100% × (n[Luc2-tdTom+])/(n[mCD45+ OR huCD45+]). Statistics depict 1-way ANOVA comparing double-treated mice to BOB1 TCR or BCMA CAR single-treated mice (Fisher's LSD test). (I) Phenotyping of U266 cells detected in the bone marrow of euthanized mice. IVIS, in vivo imaging system; ANOVA, analysis of variance; LSD, least significant difference.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/7/20/10.1182_bloodadvances.2023010410/2/m_blooda_adv-2023-010410-gr2gi.jpeg?Expires=1765062661&Signature=V3qlc5mRV9rTx1hSn~tduspeeHEPc8QHUOuseMcuBCLRTSbrySj3IRaFWzbeatuFoAsRouOSjJCn8~R9Dz1vi9v5hzDu~WXfN00hD5HGErD3OhpMcwWyZF8kjgYoUCh4SZBqog0dRCS50bHBqcHA6gVLfwyQUZZbgnN~jlcXhzPdCDO6hkymabJMDEwGpZC1zwIbionsDw8OGfcIkfs31l4Fz3nKqIqnNdtgXhYzMt3tKgm9a3YN32TI1CRXmK4vC31cWWaEAJ-1I4eQiUZXFFu10VpSHAMMdy1r8I1TLf-tK21RFL1H-UYXilH7ioQYlDhJI9HJAIwjq0dK4LvXzg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)