Key Points
Early diagnosis of SCD in Luanda, Angola using POC tests is feasible and allows for improved connection to care.
Sickle SCAN and HemoTypeSC perform as well as the gold standard isoelectric focusing to diagnose SCD in young infants.
Abstract
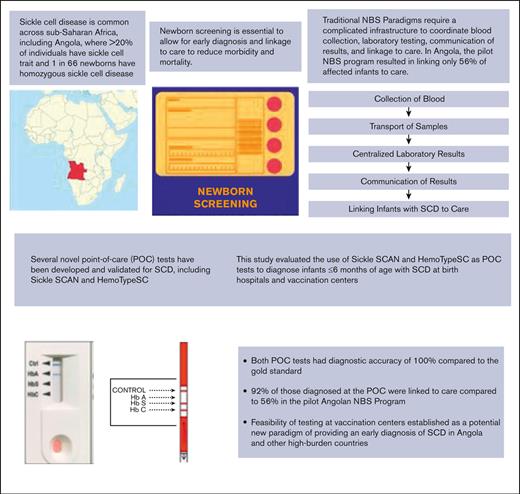
Sickle cell disease (SCD) is a life-threatening blood disorder affecting >500 000 infants annually, mostly in sub-Saharan Africa. Most infants do not have access to an early diagnosis and die early from treatable complications of SCD. Universal newborn screening (NBS) is not yet available in any African country for a variety of reasons, including lack of laboratory capacity, difficulty in tracking affected infants, and the relatively short stay of mothers and newborns at maternity hospitals. Several point-of-care (POC) tests for SCD have been recently developed and validated, but the 2 most well-established tests (Sickle SCAN and HemoTypeSC) have not been rigorously compared with one another. In this study, we aimed to evaluate and compare these 2 POC tests to screen infants aged ≤6 months in Luanda, Angola. Challenging the traditional NBS paradigm, we performed testing not only at maternity centers, but also at vaccination centers across Luanda. We enrolled 2000 babies and performed 1000 tests with each POC test. Both tests demonstrated diagnostic accuracy, with 98.3% of Sickle SCAN results and 95.3% of HemoTypeSC results aligning with the gold standard isoelectric focusing hemoglobin pattern. When the result was provided at the POC, 92% of infants were linked to SCD care compared with 56% in the pilot Angolan NBS program, which used centralized laboratory testing. This study demonstrates the real-world feasibility and accuracy of POC tests to screen infants for SCD in Angola. This study also suggests that including vaccination centers may improve the capture rate for early infant SCD screening programs.
Introduction
Sickle cell disease (SCD) is among the most common, lethal, and poorly recognized diseases across the globe. In sub-Saharan Africa, where the incidence of SCD is much higher because of the protective effect of sickle cell trait (the carrier state, HbAS) against malaria, over 500 000 children are born each year with SCD, including an estimated 10 000 per year in Angola.1-5 Most of these children die aged ∼5 years, primarily because of the lack of timely and accurate diagnosis.6-8 In well-resourced countries such as the United States and most of Europe, early identification of SCD through newborn screening (NBS) is routine, and subsequent delivery of preventive measures and comprehensive care is highly effective in reducing morbidity and early mortality.9,10 Despite the success of many pilot NBS programs primarily focused in urban centers,3,11-14 there are no countries in Africa that have effectively implemented universal NBS to date. Barriers to more widespread implementation of NBS are many, including inadequate financial, laboratory, and technical resources. The pilot NBS program in Angola used the traditional NBS paradigm of blood collection as dried blood spots (DBS) at maternity centers and centralized laboratory testing by isoelectric focusing (IEF). Published data from the first 2 years of this pilot program (2011-2013) confirmed the high burden of SCD, with 21% of infants having sickle cell trait and 1 in 66 newborns (1.6%) diagnosed with homozygous HbSS disease.3 Hemoglobin C was rare with only 21 HbFAC results (0.06%) and 7 infants with HbSC disease (0.003%). Despite persistent efforts to contact the families of affected infants, many infants with a diagnosis of SCD were unable to be reached, as only 56% of infants with SCD were linked to care in this pilot NBS program.3 Although traditional NBS programs use this paradigm of centralized laboratory testing, these higher-resource settings use existing infrastructure to relay results and establish care for infants found to have abnormal results. In contrast, in most African settings, there is lack of a traditional mailing system, lack of established primary-care providers, and inconsistent telephone numbers or telephones that cannot be reached to lack of electricity to provide a charge or insufficient credits on the account. Although early diagnosis is critically important to reduce the burden of SCD, the traditional NBS paradigm that has been effective in the United States and Europe may not be suitable for most of sub-Saharan Africa.
There are many highly effective and well-established laboratory methods to diagnose SCD, including IEF, high-performance liquid chromatography (HPLC), cellulose acetate and citrate agar electrophoresis, capillary zone electrophoresis, and DNA analysis.15 Although these methods are accurate, each requires a high degree of laboratory sophistication and technical expertise, along with the high associated costs of laboratory equipment and reagents. Because testing is often batched, results are usually not available for days to weeks and, as noted in the pilot Angolan NBS program, it becomes challenging to deliver information after positive test results. Over the past decade, there has been an increasing number of efforts recognizing the importance of developing inexpensive, accurate, point-of-care (POC) tests for SCD.16 Two of these POC tests, Sickle SCAN and HemoTypeSC, have demonstrated promise and accuracy in high- and low-resource settings and are now being distributed across Africa.17-25 These 2 POC tests have not yet been compared directly to one another in a real-world setting and there remains a debate as to whether either of these tests can serve as a standalone diagnostic method for screening infants and newborns in the high prevalence regions of sub-Saharan Africa. In this study, we aimed to evaluate and compare the accuracy of Sickle SCAN and HemoTypeSC with the gold standard IEF as primary diagnostic methods to screen newborns and young infants in Luanda, Angola. In addition, to challenge the traditional NBS paradigm of testing at maternity hospitals, the study was also designed to assess the feasibility of using these POC tests in the context of routine vaccination programs.
Methods
Study design and objectives
This was a prospective cohort study performed in Luanda, Angola with the following 3 primary objectives: (1) to compare the accuracy and limitations of 2 rapid POC tests (Sickle SCAN and HemoTypeSC) to diagnose SCD in young infants with high levels of fetal hemoglobin (HbF) living in a limited-resource setting compared with the gold standard IEF; (2) to evaluate the feasibility of obtaining an early diagnosis of SCD using POC tests at both vaccination centers and maternity facilities, challenging the traditional NBS paradigm; and (3) to determine if POC testing facilitates improved linkage to SCD care compared with traditional newborn screening using a centralized laboratory. The study was developed and performed with the collaboration of the Angolan Ministry of Health with the goal of using these data to inform national strategies to improve the early diagnosis of SCD across Angola.
Importantly, to allow for extrapolation of results, the study was designed to occur in a real-world setting with all POC testing performed and interpreted by local health care staff (nurses and laboratory technicians) with the same basic instructions for the use of the test.
Recruitment and enrollment of study participants
The Angolan Ministry of Health and local Luanda team selected 10 facilities to participate in the study. The facilities included maternity hospitals where babies were born as well as vaccination facilities where infants received their initial vaccines in the first year of life. Each facility performed 100 tests using each POC device (200 babies in total) with the intention of testing 2000 infants in total across the entire study. The study aimed to enroll newborns and young infants (aged ≤6 months) who were born at or presented for routine vaccination at one of the study sites on the day(s) the study team was present for testing. Inclusion criteria was designed to be simple, including only (1) age ≤6 months (through the last day when they were aged 6 months before turning 7 months), either born at the study site or presenting for routine vaccination; and (2) willingness of the parents to provide informed consent. Informed consent was considered necessary for this study as the the tests have not been used at the POC as primary diagnostics before. Written, informed consent was obtained before proceeding with any study procedures. If the parent was unable to provide written consent, thumbprint was used, as is standard for research studies in Angola. There were no specific exclusion criteria. Although all children would receive testing by the gold standard IEF used in the existing NBS program, the study was deemed to be research given the evaluation of the novel POC tests. Consequently, informed consent was obtained from parents/caregivers at the time of testing. To facilitate enrollment and informed consent, a member of the study team was present at the maternity or vaccination center during consent but did not otherwise interfere with or participate in study procedures or POC testing. The study was approved by the Ethics Committee within the Angola Ministry of Health and approved locally in the United States by the Cincinnati Children’s Hospital Medical Center Institutional Review Board.
Study procedures
After obtaining informed consent, blood was obtained from each infant using a lancet by heel-stick. As per the typical procedures of the traditional NBS program for testing by IEF, 2 drops of blood were obtained and saved as a DBS. After the collection of the DBS, additional blood was obtained for the specified POC test as detailed below. The total blood volume required to perform both the POC test and IEF was <1 mL. Families of the infants who were tested, were asked whether there was a known history of sickle cell in the family, with response options of yes, no, or I do not know.
POC and gold standard sickle cell testing
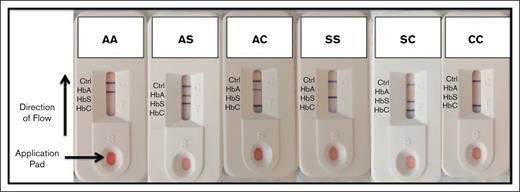
Sickle SCAN is a rapid immunoassay designed to detect the presence of HbA, HbS, and HbC within 5 minutes using only a drop of blood. The test has been validated, and it can distinguish a normal hemoglobin pattern (HbAA), sickle trait (HbAS), and the 2 most common forms of SCD (HbSS, HbSC). The test kit includes all required materials except for a lancet to draw the blood, gauze, and alcohol to clean the site (Figure 1). The procedure is simple and rapid (Figure 1B) with straightforward interpretation of results (Figure 1C), in which the presence of a band next to the label indicates presence of that specific hemoglobin. Sickle SCAN has been previously evaluated by our team and others in US-based laboratories and in real-world settings in various parts of the world, including Angola, Tanzania, Nigeria, and Haiti. The test also performed well in the presence of high amounts of HbF, suggesting that the test would be amenable to newborn screening.11-15
Sickle SCAN POC test. The Sickle SCAN results are noted by the presence of a band aligned with each hemoglobin type, including HbA, HbC, and HbS, with a control band to ensure the test is working properly. The Sickle SCAN test can qualitatively identify the presence or absence of HbA, HbS, and HbC and can accurately distinguish the most common forms of SCD (HbSS and HbSC) from the carrier states (HbAC and HbAS).
Sickle SCAN POC test. The Sickle SCAN results are noted by the presence of a band aligned with each hemoglobin type, including HbA, HbC, and HbS, with a control band to ensure the test is working properly. The Sickle SCAN test can qualitatively identify the presence or absence of HbA, HbS, and HbC and can accurately distinguish the most common forms of SCD (HbSS and HbSC) from the carrier states (HbAC and HbAS).
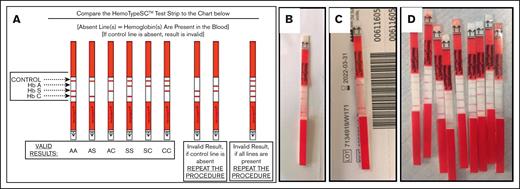
HemoTypeSC is a rapid test kit used to identify the presence of HbA, HbS, and HbC using small volumes of whole blood within 10 minutes. The procedure is depicted in Figure 2A. Lack of a band indicates the presence of the hemoglobin. This may cause misinterpretation of the assay when widely distributed, though as noted in Figure 2B, each genotype is defined by a specific pattern of bands. The test has been evaluated with encouraging results. Initial studies in US-based laboratories demonstrated correct determination of hemoglobin pattern in 100% of samples. HemoTypeSC has subsequently been used in controlled studies in the limited-resource settings of Ghana, Martinique, and Uganda with similar encouraging results.16-18
HemoTypeSC POC test. HemoTypeSC is a competitive immunoassay, such that the presence of a band indicates the absence of that particular hemoglobin. (A) Panel A demonstrates the interpretation of results. The HemoTypeSC test can qualitatively identify the presence or absence of HbA, HbS, and HbC. The subsequent panels are real-world examples from the study of results demonstrating the diagnosis of HbSS (B) and sickle cell trait (C). (D) Panel D shows the indeterminate result that indicates the presence of all 4 bands, which occurred in 4.2% of tests in this study.
HemoTypeSC POC test. HemoTypeSC is a competitive immunoassay, such that the presence of a band indicates the absence of that particular hemoglobin. (A) Panel A demonstrates the interpretation of results. The HemoTypeSC test can qualitatively identify the presence or absence of HbA, HbS, and HbC. The subsequent panels are real-world examples from the study of results demonstrating the diagnosis of HbSS (B) and sickle cell trait (C). (D) Panel D shows the indeterminate result that indicates the presence of all 4 bands, which occurred in 4.2% of tests in this study.
The DBS sample was transported to the central Angolan NBS laboratory and tested by the gold standard IEF for comparison. Testing was performed by the initial Angolan NBS laboratory staff, who had experience interpreting hundreds of thousands of results. At times, IEF results can be difficult to interpret with very faint HbA or HbS bands, particularly for infants who may be premature. The study tried through repeat testing and by using multiple experienced staff to resolve as many results as possible for comparison with POC results. If the initial IEF results were not clear, IEF was repeated using the leftover DBS to obtain a definitive diagnostic result for comparison. If repeat IEF testing was performed and the result could not be agreed upon by 2 experienced laboratory technicians, results were considered to be nondiagnostic, and the associated POC tests were not included in the final analysis due to lack of gold standard comparison.
Training and procedures for local staff performing and interpreting POC tests
Local maternity and vaccination center staff received a basic overview of each test using the company supplied package insert. After this brief introduction to testing, no additional instruction or help with reading samples was provided by the research team to best simulate a real-world testing environment. There was a consideration as the study was being designed, for having each infant tested by both methods to allow for direct comparison. However, the local teams felt that it would be too burdensome and complicated to perform both tests back-to-back and would not be reflective of how these tests would be used in the real-world setting. Thus, in the final study design, staff performed 1 POC test on 1 day and the other POC test on the following day. Although most staff were consistent for these days and were able to use both tests, the study did not specifically ensure that all staff had the ability to perform or compare both tests. At the time of the test, the gold standard IEF result was not known to any person performing the tests. For each method, the result was recorded as normal (HbAA), sickle cell trait (HbAS), SCD (HbSS), other (eg, HbAC, HbC only, HbSC), or unable to interpret. Although the result of HbSC, as a form of SCD, would be treated the same as a result of HbSS, we did not expect to find many results with HbC, given the results from the pilot NBS program. In an effort to evaluate usability, we solicited the objective and subjective feedback from providers and technicians performing the 2 POC tests and recorded the laboratory experience and job title for each person who performed a test. To allow for post hoc evaluation of possibly misinterpreted results, photographs of the test were taken after interpretation. These photographs were not used to change the primary result recorded by the end user and were only used after the fact to better understand if or why results were misinterpreted at the POC.
Counseling and education after POC testing
At the beginning of the study, the Angolan team was not comfortable relaying results to parents at the time of testing, because of uncertainty of the accuracy of the POC results and the fear of providing misleading diagnostic information to parents; however, partway into the study, as confidence grew in these test results, procedures were adjusted to inform parents of the testing results at the time and location of testing to obtain the most benefit from this POC testing. The research team included members of the initial Angolan NBS program who have nearly 10 years of experience in counseling families about SCD testing results. These experienced members of the team provided education to each family that was tested, describing the significance of each result, including HbAA, HbAS, or HbSS. Counseling was performed in a quiet and private area with a closed door to ensure confidentiality. Because POC testing was not deemed to be 100% accurate, contact information was obtained for all families in case IEF testing produced a conflicting result and to follow-up with infants diagnosed with SCD throughout the study.
Evaluation of usability and user preference among POC tests
After completing testing at each site, the end users were asked to identify their job function/role and to evaluate the usability of the POC tests with the following 3 questions: (1) did you have difficulty performing the test?; (2) did you have difficulty interpreting the test?; and (3) do you think you could incorporate this test into your daily workload?
Follow-up of infants diagnosed with SCD
For infants diagnosed with SCD, information for clinical follow-up in 1 of the 4 SCD clinics in Luanda was provided. The study team made follow-up telephone calls to determine whether SCD follow-up care was established.
Data collection and statistical analysis
Study data were initially recorded on paper case report forms at the testing sites and subsequently entered into a simple electronic database in a secured, internet–based Research Electronic Data Capture (REDCap) database. In order to transparently and systematically investigate the accuracy of these novel diagnostics, we followed the published Standards for Reporting of Diagnostic Accuracy Studies guidelines in interpreting and reporting our results.26 Kappa statistics were used to determine agreement between each test and the gold standard (IEF). Accuracy measures, including sensitivity, specificity, positive predictive values, and negative predictive values, were also calculated. Statistical significance was defined as a P value <.05. The study sample size of 2000 (1000 with each test) was a convenience sample based on birth volumes at each study site and overall study resources. Importantly, the data analysis intended to examine the ability of the real-world use of these POC tests to produce an accurate diagnosis. We, thus, included failures for any reason as “inaccurate results,” even if they were not user errors and not a problem or inaccuracy of the diagnostic test itself. This was done to allow for reporting on how well the POC tests perform in providing a diagnosis at the POC in these maternity hospital and vaccination center settings.
Results
Participants
Blood samples were collected from 2000 infants (50.7% females and 49.3% males) aged from 0 to 6 months, including 1000 tested with Sickle SCAN and 1000 with HemoTypeSC. There were 1260 tests (63%) performed at maternity centers and 740 tests (37%) performed at vaccination centers. The tests were performed and interpreted by local staff at each testing location, including nurses (48.5%), students (30.5%), laboratory technicians (20.8%), and physicians (0.2%). The mean (standard deviation) age of infants at the time of testing was 30.9 (52.3) days with a range from 0 to 213 days (3 study participants had a missing date of birth recorded).
Gold standard IEF results
The overall distribution of hemoglobin patterns as determined by the gold standard IEF was exactly in line with previously published NBS results from Luanda, Angola, demonstrating the high burden of SCD (Table 1), with 22.1% of infants having a pattern consistent with sickle cell trait (FAS) and 1 in 59 infants (1.7%) identified with a pattern consistent with sickle cell anemia (FS). There were no results identifying the presence of HbC (HbAC, HbC only, or HbSC), consistent with the low prevalence of HbC in Luanda from the pilot NBS program. There were 104 participants whose samples (5.5%) had indeterminate initial IEF results (faint bands or results that were read differently by the 2 experienced laboratory technicians) and had to be repeated. Of these, a total of 11 (0.6%) samples, despite repeat testing, were unable to provide a diagnostic IEF result. Thus, the total number of samples used for comparison with the POC tests was 989.
Results of screening tests using gold standard IEF results
| . | N . | % . |
|---|---|---|
| HbAA | 1513 | 73.7 |
| HbAS | 442 | 22.1 |
| HbSS | 34 | 1.7 |
| IEF indeterminate | 11 | 0.6 |
| . | N . | % . |
|---|---|---|
| HbAA | 1513 | 73.7 |
| HbAS | 442 | 22.1 |
| HbSS | 34 | 1.7 |
| IEF indeterminate | 11 | 0.6 |
There were 70 out of 1000 mothers (3.5%) who reported a known family history of SCD in the family. Of those 70 mothers, 11 (15.7%) had a result consistent with SCD (FS) and 28 (40%) had a result consistent with sickle cell trait (FAS).
Sickle SCAN results
A total of 1000 infants were tested using Sickle SCAN. The Sickle SCAN test took an average of 7 minutes to obtain a result and was repeated 2 times (0.2%) (1 sample spilled before application on the testing cassette and the other 1 did not produce bands that were visible). In this real-world setting, after excluding the 11 results that did not have a diagnostic IEF result for comparison, the Sickle SCAN result obtained at the POC aligned correctly with the gold standard IEF result in 972 of 989 tests (98.3%). Of the 17 results that were not accurately diagnosed at the time of testing, 6 (0.6%) were due to the test not being read within the recommended 5-minute time frame and 11 (1.1%) were read inaccurately. Results that were read incorrectly were primarily because of very faint bands that were difficult to distinguish. Importantly, of the 11 tests that were read inaccurately, there were no missed diagnoses of SCD and no false positive SCD diagnoses. Overall, there were only 1.7% of samples with errors that were due to the performance or interpretation of the test by the user. The actual test results, when the test was performed and interpreted correctly, aligned with the gold standard 100% of the time. When looking specifically at the ability to diagnose SCD, Sickle SCAN had a sensitivity, specificity, positive predictive value, and negative predictive value of 100%.
HemoTypeSC results
A total of 1000 infants were tested using HemoTypeSC. Testing with HemoTypeSC took an average of 15 minutes to obtain a result and needed to be repeated 42 times (4.2%) because of invalid results (the result strip showed all 4 bands, Figure 2D). In this real-world setting, after excluding the 11 results that did not have a diagnostic IEF result for comparison, the HemoTypeSC result obtained at the POC aligned correctly with the gold standard IEF result in 943 of 989 tests (95.3%). There were 46 total HemoTypeSC tests that did not provide an accurate result for a variety of reasons. Most (42/46 [4.2% of total samples]) did not provide an interpretable result at all, because the test strip was not removed from the solution within the recommended 10-minute time frame, resulting in a blurred and uninterpretable result. These happened to 42 samples on a single day of testing during which the nurses performing the test forgot to return to read the result and the infants had already left, not allowing for repeat testing. Although this is not the fault of the test itself, it illustrates potential opportunities for errors in the testing process. There were only 4 HemoTypeSC tests (0.4%) that were interpreted inaccurately when the research team compared the results at the POC care with the photographs. These photographs were used to better understand whether the test was misinterpreted or the test produced an incorrect or difficult to interpret result. Of the 4 that were read incorrectly, the recorded result was HbAA when it should have been HbAS (based on the research team reviewing the photo of the test). Importantly, there were no HbSS results that were missed, and no babies were incorrectly labeled as HbSS. Overall, there were 3.6% of samples with errors that were because of the performance or interpretation of the test by the user. The actual test results, when the test was performed and interpreted correctly, aligned with the gold standard 100% of the time. When looking specifically at the ability to diagnose SCD, HemoTypeSC had a sensitivity, specificity, positive predictive value, and negative predictive value of 100%.
User experience
Overall, both tests were reviewed as easy to perform and interpret. For Sickle SCAN, 29% reported some difficulty in performing the test, whereas 18% reported some difficulty in performing the HemoTypeSC test. Most users reported no difficulties in interpreting the tests (70% for HemoTypeSC and 75% for Sickle SCAN). Nearly all users (98%) reported that they could incorporate Sickle SCAN into their daily workload, compared with 84% for HemoTypeSC.
Linkage to sickle cell care
A total of 34 infants (1.7%) were identified in the study with a result of HbSS, consistent with SCD. As noted in “Methods,” the initial phase of the study waited for confirmatory IEF results before informing the family. There were 10 infants identified with SCD in this phase and only 4 (40%) were able to be contacted with results to link them to care, whereas 6 infants (60%) were unable to be contacted and, thus, lost to follow-up, similar to results from the initial Angola NBS program. In the phase of the study during which the results were provided at the POC, 22 of 24 infants (92%) established care with the SCD clinic. When infants were brought back to care, repeat testing by 1 of the 2 POC tests was performed to confirm the diagnosis, which was accurate for all cases.
Discussion
The global burden of SCD is already tremendous, and with the implementation of basic health interventions in settings such as sub-Saharan Africa and India, the number of affected infants and surviving children with SCD is projected to increase even further in the coming decades.1 The implementation of universal NBS1 could save the lives of >5 million newborns with SCD by 2050. The traditional NBS paradigm, developed in high-resource settings of the United States and Europe, includes obtaining a blood sample at birth hospitals in the first days of life and sending these DBS to centralized laboratories for testing for dozens of conditions, including SCD. There is an associated infrastructure to relay abnormal results to primary-care providers and families such that linkage to care is established for most affected infants. In the limited-resource settings of sub-Saharan Africa, there are many obstacles to the completion of even 1 of these complicated series of steps from testing babies to establishing specialized SCD care. More than a decade ago, our team developed and implemented a pilot NBS program for SCD in Luanda, Angola, based upon this traditional NBS paradigm. Although this pilot program (and many others) was successful in diagnosing many babies with SCA, allowing for establishment of care and likely prevention of early mortality, there were several challenges that prevented testing all babies and establishing care with those found to have SCD. The maternity hospital setting, in which mothers and babies are often released from 6 to 12 hours after birth, is chaotic making it difficult to add the additional step of NBS. The centralized laboratory testing by IEF is labor intensive and time consuming, and it is often challenging to relay positive results to mothers because there is no established postal system or network of primary-care providers. This study was designed to challenge the traditional NBS paradigm and provide data to support an innovative early diagnosis strategy to diagnose and link as many infants as possible to specialized SCD care.
This study has several important and novel findings. First, the study compared the 2 most widely available POC tests for SCD with each other and with the gold standard, both in terms of diagnostic accuracy and user friendliness. We confirmed that both tests were highly accurate even in newborns with high levels of HbF. In fact, the failure rate of these POC tests was better than that of the gold standard NBS method, IEF, which did not provide an accurate result in 0.6% of samples, with many others requiring repeat IEF runs to produce an agreed upon result. Most inadequate or incorrect POC results were related to errors in the process of testing and not the actual tests themselves, which continued to demonstrate tremendous accuracy. Based on our experience and this study, we support the use of these POC tests as standalone diagnostic tests for the early diagnosis of SCD in limited-resource settings. Repeat confirmatory testing can be performed using a more advanced methodology such as IEF or HPLC if available, but this is not required and may not be available in most settings. Sub-Saharan Africa has an extremely high prevalence of HbS, with some regions also having HbC. Both POC tests can accurately diagnose the most common and severe forms of SCD, including HbSS and HbSC diseases. The POC tests do have limitations in that they cannot diagnose HbS/β-thalassemia or identify other hemoglobin variants such as HbD, HbE, or HbO; however, these variants are rare. The most effective way to allow for widespread diagnosis of the most common forms of SCD is by deploying these POC tests. Future efforts can focus on more advanced backup or confirmatory technologies that may be able to identify other rare forms of SCD. Before establishing sickle cell care, each infant should be tested again using any accurate test (including the POC tests described here) to confirm that the initial result was, in fact, from the baby presenting for SCD care. It is simply not feasible to expect the availability of HPLC or IEF across most of sub-Saharan Africa and requiring one of these methodologies for confirmatory testing would be a tremendous barrier to true universal NBS. In addition to confirming the accuracy of these POC tests, this study also demonstrates the feasibility of expanding the early diagnosis of SCD beyond the birth hospital to vaccination centers. The complications of SCD usually do not manifest until after age from 4 to 6 months, when the levels of HbF decline such that sickle hemoglobin predominates. This provides a window from 4 to 6 months during which it is critical to establish the diagnosis of SCD to allow linkage to care. This contrasts with many metabolic disorders that require a diagnosis within days to weeks. These metabolic disorders, such as phenylketonuria, were the first tests included in NBS programs and are the reason why the paradigm of testing in the first 24 to 48 hours after birth was established.27,28 In settings such as sub-Saharan Africa, SCD is likely to be the only condition tested for, allowing us to challenge or augment the traditional NBS paradigm. This study demonstrates that expansion of testing beyond the birth hospitals to include vaccination centers is likely to increase the numbers of infants that are tested and diagnosed. Testing at vaccination centers will identify infants who are born at home or those who may miss being tested owing to the maternity hospital staff being busy. Infants present for vaccinations several times through the first year of life, allowing many opportunities for testing. We suggest the integration of SCD testing into primary care services such as vaccination programs. We recommend that Ministries of Health in high burden countries link early SCD testing to national immunization programs, by including SCD testing on national vaccination cards to document if a child was tested and what the result of the test was. This multilayered strategy, using POC testing to allow for immediate counseling and linkage to care, is more likely to allow for widespread, even universal, NBS in these settings. There is also the possibility that if SCD testing is considered to be important for many families, the linkage of vaccination with SCD testing may potentially also increase the frequency with which infants receive vaccinations.
Importantly, the POC tests, although feasible and accurate, must be available and cost-effective. Although the cost to purchase these POC tests is approximately from $3-5 per test, there is some cost inflation as tests are imported and resold locally. In Angola, each test is sold exclusively by 1 distributor with the current per test cost of $4.60 USD for Sickle SCAN and $7.06 for HemoTypeSC. In comparison, the reagent only cost to perform IEF is $1.58, in addition to the upfront cost of equipment, which is approximately between $20 000 and $30 000 USD. To allow for expanded access to and use of the POC tests, it will be necessary to drive down the end-user price to be closer to the production costs without the excessive cost inflation because of fees related to importation and exploitation of the high demand for diagnostics in high prevalence regions. Cost effectiveness analyses, which incorporate the downstream effects of POC testing and linkage to care, will also be important to demonstrate the value of universal screening.
This study does have some limitations. The study was performed in an urban setting and although the intent was to create a real-world experience, there may have been some influence from the fact that this was a research study and our study team was on site on the day of testing. Although the study team did not interfere or engage with the end users while testing or interpretation was being performed, the study itself or the presence of study staff may have resulted in more attention by the end users that could have affected the overall testing procedures at each birth hospital and vaccination site. Further real-world implementation studies that are done without supervision or in the context of a study, in both urban and rural settings, will be necessary to further validate the feasibility and success of this early diagnosis strategy, because there may be different levels of expertise and fewer available staff in rural settings. There is also a varying volume of children at maternity and vaccination centers in urban and rural settings. Although POC tests are simple and easy to interpret, they are difficult to batch and must be performed 1 at a time, perhaps creating challenges in very high-volume settings. Testing was performed at each site usually on subsequent days using one of the POC tests each day, and the staff was often the same on both days; however, the study did not ensure that all staff had the opportunity to use and compare both tests. Furthermore, as noted in “Methods,” the tests were not performed at the same time on the same babies based on feedback by local staff to ensure a more real-world and simplified testing process. This made it difficult to determine if both tests would produce difficult to interpret results on the same babies or not, but overall, both tests comparably performed very well. Finally, although the linkage to care was excellent with the POC testing strategy, the study did not follow these infants over a longer period, which will be necessary to clearly demonstrate the impact on morbidity and mortality of SCD.
In conclusion, this study provides further validation of the diagnostic accuracy and clinical utility of POC tests for SCD. As these tests are now becoming increasingly available, these data support the widespread implementation of either Sickle SCAN or HemoTypeSC as primary diagnostic methods for the early diagnosis of SCD. Early diagnosis programs should consider the inclusion of vaccination centers and birth hospital as testing sites to capture more infants. Further implementation studies are needed, including careful analysis of end-user cost, to determine the appropriate strategy for widespread implementation of these POC tests in low-resource settings of sub-Saharan Africa.
Acknowledgments
The authors thank the 2000 mothers and their babies who participated in this study. They acknowledge Francisco Domingos and Cesar Freitas and the leadership of both Hospital Pediátrico David Bernardino and Instituto Hematológico Pediátrico for their continued support of our collaborative sickle cell work in Angola. The authors also thank the leadership and staff of each birth hospital and vaccination center for their enthusiastic participation in this important study.
Authorship
Contribution: C.B., A.A., B.S. and P.T.M. designed the study; C.B., M.M., R.P, A.A, and B.S. performed the research; H.S.O. analyzed the data and wrote the first draft of the manuscript; and all authors contributed to editing and revising the final manuscript before approval.
Conflict-of-interest disclosures: The authors declare no competing financial interests.
Correspondence: Patrick T. McGann, Lifespan Comprehensive Sickle Cell Center, 593 Eddy St, Suite 105, Providence, RI 02903; e-mail: patrick_mcgann@brown.edu.
References
Author notes
Any publication-related data are available on request from the corresponding author, Patrick T. McGann (patrick_mcgann@brown.edu).