Key Points
CRS after haploidentical stem cell transplantation is associated with enhanced early T-cell reconstitution.
CRS after haploidentical stem cell transplantation is associated with a lower incidence of posttransplant relapse.
Abstract
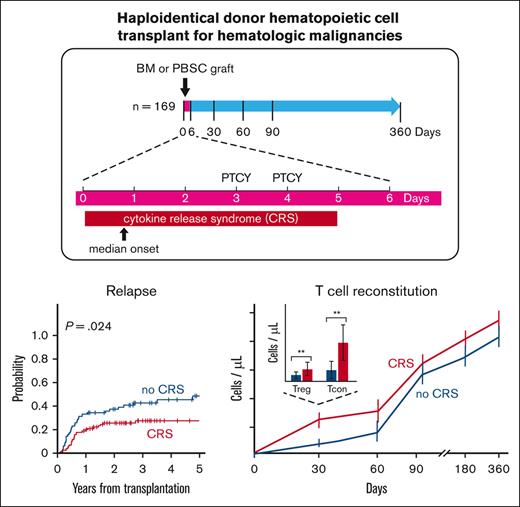
Cytokine release syndrome (CRS) following haploidentical hematopoietic cell transplantation (HCT) resembles CRS after chimeric antigen receptor-T therapy. We conducted this single-center retrospective study to evaluate the association of posthaploidentical HCT CRS with clinical outcomes and immune reconstitution. One hundred sixty-nine patients who underwent haploidentical HCT between 2011 and 2020 were identified. Of these, 98 patients (58%) developed CRS after HCT. CRS was diagnosed based on the presence of fever within the first 5 days after HCT without evidence of infection or infusion reaction and was graded according to established criteria. The development of posthaploidentical HCT CRS was associated with a lower incidence of disease relapse (P = .024) but with an increased risk of chronic graft-versus-host disease GVHD (P = .01). The association of CRS with a lower incidence of relapse was not confounded by graft source or disease diagnosis. Neither CD34 nor total nucleated cell dose was associated with CRS independently of graft type. In patients developing CRS, CD4+ Treg (P < .0005), CD4+ Tcon (P < .005), and CD8+ T cells (P < .005) increased 1 month after HCT compared with those who did not develop CRS, but not at later time points. The increase in CD4+ regulatory T cells 1 month after HCT was most notable among patients with CRS who received a bone marrow graft (P < .005). The development of posthaploidentical HCT CRS is associated with a reduced incidence of disease relapse and a transient effect on post-HCT immune reconstitution of T cells and their subsets. Therefore, the validation of these observations in a multicenter cohort is required.
Introduction
Cytokine release syndrome (CRS) was originally defined as an adverse event in the context of chimeric antigen receptor T-cell (CAR-T) therapy, viral infections, and immunotherapy.1,2 As the number of haploidentical hematopoietic cell transplants (HCTs) has increased over the last several years with the introduction of posttransplantation cyclophosphamide, CRS has also been recognized as a common phenomenon in this setting.3-9 However, unlike in the CAR-T setting, the clinical implications of the development of CRS following haploidentical HCT remain unclear. For example, although CRS has been associated with a reduced incidence of relapse in some studies, it has not been associated with others.4,9 In particular, whether CRS development impacts immune reconstitution or influences haploidentical HCT outcomes, such as relapse or nonrelapse mortality, is not definitively known.
The pathophysiology of CRS is thought to involve the activation of immune effector cells upon encountering a target that results in the release of IFNγ and TNFα, promoting the release of IL-6 from bystander cells, including monocytes, macrophages, endothelial cells, dendritic cells, and T cells. This further drives the expansion and activation of immune effector populations and subsequent propagation of additional cytokine release.10,11 In the context of CAR-T therapy, the syndrome has been associated with the characteristics of infused cells, including their quantity, expansion, and specific engineered constructs.12 The tumor burden has also been associated with the frequency and severity of CRS in patients treated with CAR-T therapy.12 Furthermore, tumor type has some relevance to post–CAR-T CRS, with retrospective studies in B-cell malignancies suggesting that severe CRS is most frequent in ALL and lymphoma.12,13
Although posthaploidentical HCT CRS shares characteristics with CAR-T CRS, important differences include the relatively low disease burden at the time of HCT as well as the occurrence in a human leukocyte antigen mismatched alloimmune setting. The association between disease type and burden at the time of haploidentical HCT contributing to CRS has been made in some retrospective studies,5,6 but not in others.7 Whether disease diagnosis or residual burden at the time of HCT increases the risk of the development of CRS is unknown.
To address the current gaps in knowledge regarding posthaploidentical HCT CRS, we conducted this single-center retrospective study in a cohort of patients who received haploidentical HCT and for whom longitudinal immune reconstitution data were available. In particular, we focused on determining whether CRS was associated with the disease type or residual burden at the time of HCT and whether it was related to clinical outcomes or immune reconstitution.
Methods
Patients
Patients who underwent haploidentical HCT at the Dana-Farber Cancer Institute between 1 December 2011 and 1 December 2020, were retrospectively identified using an institutional database. All characteristics of the disease that were the indications for HCT were collected from the chart review and the classification of acute myeloid leukemia clinical ontogeny was performed as described by Lindsley et al.14 Patients who received HCT for nonmalignant diseases were excluded. All patients received graft-versus-host disease (GVHD) prophylaxis with cyclophosphamide (posttransplantation cyclophosphamide) on days +3 and +4 following stem cell infusion, with additional mycophenylate mofetil and tacrolimus or sirolimus, starting on day +5. A detailed review of patient charts was undertaken to diagnose and grade CRS, with collected data including temperature, blood pressure and need for fluid supplementation or vasopressor requirement, oxygenation status and need for supplemental O2, need for mechanical ventilation, hepatic function, and renal function. The diagnosis of CRS was based on the development of a new fever in the absence of any evidence of infection based on clinical documentation, blood culture and urine culture data, and any concurrent imaging findings. CRS grading was performed per the previously described criteria.3,4,10 Tocilizumab was considered for any patient with grade 2 or higher CRS in accordance with our standard institutional policy.
Flow cytometry
All patients provided consent for a standard IRB-approved protocol for posttransplantation sample collection. Peripheral blood samples following HCT were collected at timed intervals at the discretion of the treating clinician. Peripheral blood mononuclear cells were isolated using Ficoll centrifugation and cryopreserved in 10% DMSO until analysis. A panel of antibodies customized to identify natural killer cells and T-cell subsets was applied to the collected samples, as previously described.15 Flow cytometry cell staining was performed as previously described.15 Data were acquired on a BD LSR Fortessa flow cytometer and analyzed using FlowJo (Tree Star) software. Calculation of the absolute quantities of all immune effector cell subsets was based on their proportion, as determined by flow cytometry applied to the absolute peripheral white blood cell counts and lymphocyte counts, with the latter obtained from the clinical pathology blood count analyzer.
Statistical analysis
Baseline and pretransplantation characteristics were reported descriptively and compared using Fisher exact test, χ2 test, or Wilcoxon rank-sum test, as appropriate. Univariable and multivariable logistic regression analyses were performed to investigate clinical factors associated with CRS. Because all cases of CRS occurred within 5 days of HCT with a median time to onset of 1 day and no death or relapse occurred within 5 days, without loss of generality, CRS was treated as a time fixed variable in all analyses. Overall survival (OS) and progression-free survival (PFS) were estimated using the Kaplan-Meier method and log-rank test was used for group comparisons. Time-to-events were measured from stem cell infusion to death (OS) or death/disease progression (PFS), whichever occurred first. The cumulative incidences of nonrelapse mortality, relapse, and acute/chronic GVHD were estimated in the competing risks framework, considering relapse, nonrelapse mortality, and relapse or death without developing GVHD as a competing event, respectively. The difference between the cumulative incidences in the presence of a competing risk was tested using the Gray method.16 Cox regression analysis for OS and PFS and Fine and Gray17 competing risks regression analysis for relapse were performed to investigate the prognostic implications of CRS for these outcomes in the presence of other factors. The factors considered in the regression analysis included age at transplantation, male recipient with a female donor, graft source, disease risk index, primary disease, conditioning intensity, HCT-comorbidity index, patient and donor cytomegalovirus serostatus, year of transplantation, measurable residual disease status at transplantation, disease diagnosis, and amount of CD34 and total nucleated cell (TNC) infused per kilogram of graft (Table 1). Before regression analysis, the linearity assumption for all continuous variables was examined using the methods of restricted cubic spline function on relative hazard and classification and regression tree for survival data.18,19 Before performing the Cox regression analysis, the proportional hazards assumption was examined. Immunologic parameters were analyzed primarily descriptively and compared using the Wilcoxon rank-sum test for group comparisons and Wilcoxon Signed-Rank test for paired comparisons. All tests were 2-sided at a significance level of 0.05. Multiple comparisons were not considered. All analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC) and R v3.4 (the CRAN Project).
Baseline clinical characteristics and univariate analysis of the posthaploidentical HCT CRS cohort
| Baseline characteristics . | Total . | No CRS . | CRS . | P value . | |
|---|---|---|---|---|---|
| Age at HCT, median (range) | 58 (20-76) | 55 (23-74) | 60 (20-76) | .19 | |
| CD34 cell dose at HCT∗, median (range) | 5.6 (1-29) | 3.7 (1-19.9) | 7.4 (1.2-29) | <.0001 | |
| TNC cells/kg at HCT†, median (range) | 6.1 (1.3-28.4) | 3.7 (1.3-18.4) | 8.8 (2.1-28.4) | <.0001 | |
| Graft source, n (%)‡ | BM | 88 (52.1) | 57 (80.8) | 31 (31.6) | <.0001 |
| PBSC | 81 (47.9) | 14 (19.2) | 67 (68.4) | ||
| Conditioning intensity, n (%) | Myeloablative | 42 (24.9) | 18 (25.4) | 24 (24.5) | 1 |
| Reduced Intensity | 127 (75.1) | 53 (74.6) | 74 (75.5) | ||
| Disease risk index, n (%) | Low | 8 (4.7) | 5 (7) | 3 (3.1) | .24 |
| Intermediate | 104 (61.5) | 47 (66.2) | 57 (58.2) | ||
| High | 51 (30.2) | 16 (22.5) | 35 (35.7) | ||
| Very high | 5 (3) | 2 (2.8) | 3 (3.1) | ||
| Patient sex, n (%) | Female | 67 (39.6) | 27 (38) | 42 (42.9) | .63 |
| Male | 102 (60.4) | 44 (62) | 56 (57.1) | ||
| Male recipient and female donor, n (%) | 31 (18.3) | 15 (21.1) | 16 (16.3) | .43 | |
| Cytomegalovirus serostatus in donor or recipient, n (%) | Negative | 59 (34.9) | 27 (38) | 32 (32.7) | .31 |
| Positive | 110 (65.1) | 44 (62) | 66 (67.3) | ||
| Disease, n (%) | ALL | 21 (12.4) | 5 (7) | 16 (16.3) | .47 |
| AML | 70 (41.4) | 30 (42.3) | 40 (40.8) | ||
| CLL | 1 (0.6) | 1 (1.4) | 0 (0) | ||
| HL | 7 (4.1) | 3 (4.2) | 4 (4.1) | ||
| MDS | 5 (3) | 1 (1.4) | 4 (4.1) | ||
| MDS/MPN | 38 (22.5) | 16 (22.5) | 22 (22.4) | ||
| MPN/CML | 3 (1.8) | 2 (2.8) | 1 (1) | ||
| NHL | 21 (12.4) | 11 (15.5) | 10 (10.2) | ||
| T-PLL | 3 (1.8) | 2 (2.8) | 1 (1) | ||
| HCT-comorbidity index score, n (%) | 0-2 | 103 (61) | 44 (62) | 59 (60.2) | .87 |
| ≥3 | 66 (39) | 27 (38) | 39 (39.8) | ||
| Pretransplant measurable residual disease, n (%) | ND | 24 (14.2) | 15 (21.1) | 9 (9.2) | .07 |
| No | 58 (34.3) | 20 (28.2) | 38 (38.8) | ||
| Yes | 87 (51.5) | 36 (50.7) | 51 (52) | ||
| Baseline characteristics . | Total . | No CRS . | CRS . | P value . | |
|---|---|---|---|---|---|
| Age at HCT, median (range) | 58 (20-76) | 55 (23-74) | 60 (20-76) | .19 | |
| CD34 cell dose at HCT∗, median (range) | 5.6 (1-29) | 3.7 (1-19.9) | 7.4 (1.2-29) | <.0001 | |
| TNC cells/kg at HCT†, median (range) | 6.1 (1.3-28.4) | 3.7 (1.3-18.4) | 8.8 (2.1-28.4) | <.0001 | |
| Graft source, n (%)‡ | BM | 88 (52.1) | 57 (80.8) | 31 (31.6) | <.0001 |
| PBSC | 81 (47.9) | 14 (19.2) | 67 (68.4) | ||
| Conditioning intensity, n (%) | Myeloablative | 42 (24.9) | 18 (25.4) | 24 (24.5) | 1 |
| Reduced Intensity | 127 (75.1) | 53 (74.6) | 74 (75.5) | ||
| Disease risk index, n (%) | Low | 8 (4.7) | 5 (7) | 3 (3.1) | .24 |
| Intermediate | 104 (61.5) | 47 (66.2) | 57 (58.2) | ||
| High | 51 (30.2) | 16 (22.5) | 35 (35.7) | ||
| Very high | 5 (3) | 2 (2.8) | 3 (3.1) | ||
| Patient sex, n (%) | Female | 67 (39.6) | 27 (38) | 42 (42.9) | .63 |
| Male | 102 (60.4) | 44 (62) | 56 (57.1) | ||
| Male recipient and female donor, n (%) | 31 (18.3) | 15 (21.1) | 16 (16.3) | .43 | |
| Cytomegalovirus serostatus in donor or recipient, n (%) | Negative | 59 (34.9) | 27 (38) | 32 (32.7) | .31 |
| Positive | 110 (65.1) | 44 (62) | 66 (67.3) | ||
| Disease, n (%) | ALL | 21 (12.4) | 5 (7) | 16 (16.3) | .47 |
| AML | 70 (41.4) | 30 (42.3) | 40 (40.8) | ||
| CLL | 1 (0.6) | 1 (1.4) | 0 (0) | ||
| HL | 7 (4.1) | 3 (4.2) | 4 (4.1) | ||
| MDS | 5 (3) | 1 (1.4) | 4 (4.1) | ||
| MDS/MPN | 38 (22.5) | 16 (22.5) | 22 (22.4) | ||
| MPN/CML | 3 (1.8) | 2 (2.8) | 1 (1) | ||
| NHL | 21 (12.4) | 11 (15.5) | 10 (10.2) | ||
| T-PLL | 3 (1.8) | 2 (2.8) | 1 (1) | ||
| HCT-comorbidity index score, n (%) | 0-2 | 103 (61) | 44 (62) | 59 (60.2) | .87 |
| ≥3 | 66 (39) | 27 (38) | 39 (39.8) | ||
| Pretransplant measurable residual disease, n (%) | ND | 24 (14.2) | 15 (21.1) | 9 (9.2) | .07 |
| No | 58 (34.3) | 20 (28.2) | 38 (38.8) | ||
| Yes | 87 (51.5) | 36 (50.7) | 51 (52) | ||
P values below the threshold of 0.05 have been shown in bold.
ALL, acute lymphocytic leukemia; AML, acute myeloid leukemia; CLL, chronic lymphocytic leukemia; CML, chronic myeloid leukemia; HL, Hodgkin lymphoma; MDS, myelodysplastic syndrome; MDS/MPN, myelodysplastic syndrome-myeloproliferative neoplasm overlap; MPN, myeloproliferative neoplasm; ND, not done; NHL, non-Hodgkin lymphoma; T-PLL, T-prolymphocytic leukemia.
Presented as ×106 cells/kg.
Presented as ×108 cells/kg.
All percentages refer to the ratio of number (n) to the total number of patients within an individual group (CRS or no CRS).
Results
Patient characteristics
The baseline clinical characteristics of all patients who received haploidentical HCT for malignant disease and a comparison of the patients who developed CRS with those who did not are summarized in Table 1. Fifty-eight percent of patients (98/169) met the clinical criteria for a diagnosis of CRS, as defined by the American Society for Transplantation and Cellular Therapy consensus grading.10 Onset of CRS within the first 5 days after HCT was not associated with the cooccurrence of severe neutropenia, defined as an absolute neutrophil count <0.5 × 109 cells/ μL. Among all patients who developed CRS, the majority were grade 1 (65/98, 66%) or grade 2 (31/98, 32%). Two patients had CRS grades of 3 to 4. The median time to onset of CRS was 1 day (range, 0-5) after stem cell infusion, whereas the median time to the maximum severity of CRS was 3 days (range, 0-5) after stem cell infusion. Twenty-five patients with CRS were treated with tocilizumab, with 80% of patients receiving the drug for grade ≥2 CRS. The median time to resolution of CRS was on day +5 after stem cell infusion (supplemental Table 1).
Comparing patients who did and did not develop CRS, no significant differences were detected with respect to age, sex, diagnosis at transplantation, conditioning intensity, and the cytomegalovirus serostatus of both patient and donor (Table 1).
CRS is associated with a peripheral blood stem cell (PBSC) graft source
In univariable analysis, the development of CRS was associated with PBSC graft source (P < .0001), CD34+ and TNC cell dose per kilogram (P < .0001, for both) (Table 1). There was an association between CRS grade and graft source (Χ2 [1, N = 98] = 11.7; P = .0006)), with patients receiving a PBSC graft being more likely to develop grade ≥2 CRS. Although CD34+ and TNC cell dose per kilogram appeared to be associated with the development of CRS, these were highly correlated with the graft source. CD34+ and TNC cell dose per kilogram were higher in PBSC grafts (median: 9.4 × 106 CD34+ cells/kg, 10.1 × 108 TNC cells/kg) than in bone marrow (BM) graft (median, 3.2 × 106 CD34+ cells/kg, 3.5 × 108 TNC cells/kg; P < .0001 for both differences), and a higher proportion of patients with CRS received PBSC grafts (68.4% vs 19.2%; P < .0001). When CD34+ and TNC cell doses were compared within each graft source, these cell doses between patients with and without CRS did not differ. In multivariable analysis, only a PBSC graft source was independently associated with the development of posthaploidentical HCT CRS (odds ratio 8.4; 95% confidence interval [CI], 3.5-22.6). The factors considered in the regression analysis included age at transplantation, male recipient with a female donor, cell source (BM or peripheral blood), disease risk index, HCT-comorbidity index, cytomegalovirus serostatus, primary disease, conditioning intensity, measurable residual disease status at transplantation, and year of transplantation. Notably, a parsimonious model adjusting for age, male patient with female donor, and disease risk index led to a very similar result.
Development of CRS following haploidentical HCT is associated with reduced posttransplantation relapse
The development of CRS was associated with a decreased incidence of posthaploidentical HCT relapse (3-year estimate, 27% [95% CI, 18-37] vs 41% [95% CI, 29-50]; P = .024) (Figure 1), with the association not confounded by graft source (Figure 2A). This result is consistent with the results of the multivariable Fine and Gray regression analysis (sHR 0.53; 95% CI, 0.3-0.94; P = .03) (supplemental Table 2). The relapse incidence was not different between grade 1 and grade ≥2 CRS (2-year relapse: 26% vs 28%, respectively) (supplemental Figure 1). We explored whether the association between CRS and relapse was confounded by the disease and found no association between CRS incidence and disease diagnosis (supplemental Figure 2A). Among patients with myeloid disease, the development of CRS was not associated with gene mutation type (supplemental Figure 2B). In patients with acute myeloid leukemia in whom distinct leukemia ontogeny can be identified from the gene mutation profile, we found no association between disease ontogeny and development of CRS (supplemental Figure 2C).
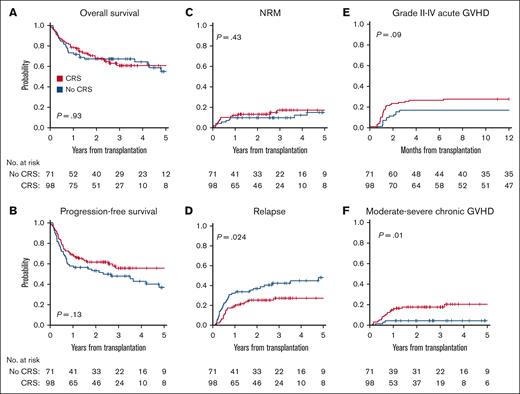
Posthaploidentical HCT outcomes following the development of CRS. (A) OS, (B) PFS, (C) nonrelapse mortality, (D) relapse, (E) grade 2 to 4 acute GVHD, and (F) moderate-to-severe chronic GVHD.
Posthaploidentical HCT outcomes following the development of CRS. (A) OS, (B) PFS, (C) nonrelapse mortality, (D) relapse, (E) grade 2 to 4 acute GVHD, and (F) moderate-to-severe chronic GVHD.
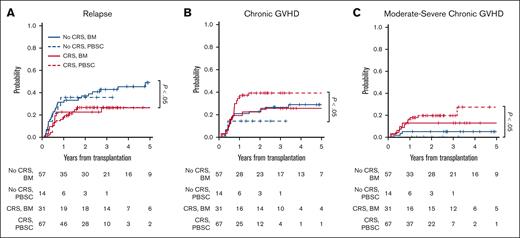
Posthaploidentical HCT outcomes following the development of CRS stratified by graft source. (A) Cumulative incidence of relapse among patients who did and did not develop CRS, stratified by graft source. Shown is the comparison between CRS and no CRS groups among patients receiving either a BM or PBSC graft. (B) Cumulative incidence of chronic GVHD in patients who did and did not develop CRS and received either a BM or PBSC graft. Shown is the comparison between the CRS and no CRS groups among patients receiving a PBSC graft. (C) Cumulative incidence of moderate-to-severe chronic GVHD in patients who did and did not develop CRS and received either a BM or PBSC graft. Shown is the comparison between the CRS and no CRS groups among patients receiving a PBSC graft. Fourteen of the 81 patients who received a PBSC graft did not develop CRS, and none of these 14 patients developed moderate-to-severe chronic GVHD (dashed blue line on the x-axis).
Posthaploidentical HCT outcomes following the development of CRS stratified by graft source. (A) Cumulative incidence of relapse among patients who did and did not develop CRS, stratified by graft source. Shown is the comparison between CRS and no CRS groups among patients receiving either a BM or PBSC graft. (B) Cumulative incidence of chronic GVHD in patients who did and did not develop CRS and received either a BM or PBSC graft. Shown is the comparison between the CRS and no CRS groups among patients receiving a PBSC graft. (C) Cumulative incidence of moderate-to-severe chronic GVHD in patients who did and did not develop CRS and received either a BM or PBSC graft. Shown is the comparison between the CRS and no CRS groups among patients receiving a PBSC graft. Fourteen of the 81 patients who received a PBSC graft did not develop CRS, and none of these 14 patients developed moderate-to-severe chronic GVHD (dashed blue line on the x-axis).
Among all patients, no differences in OS (P = .93), PFS (P = .13), or cumulative incidence of nonrelapse mortality (P = .59) were observed between patients who did or did not develop CRS. However, the development of CRS was associated with an increased risk of moderate-to-severe chronic GVHD (2-year estimate 18% [95% CI, 11-26] vs 4% [95% CI, 1-11]; P = .01), with the association being most notable among patients who received PBSC grafts (Figures 2B-C). Treatment of CRS with tocilizumab was not associated with any effect on key HCT outcomes (supplemental Figure 3).
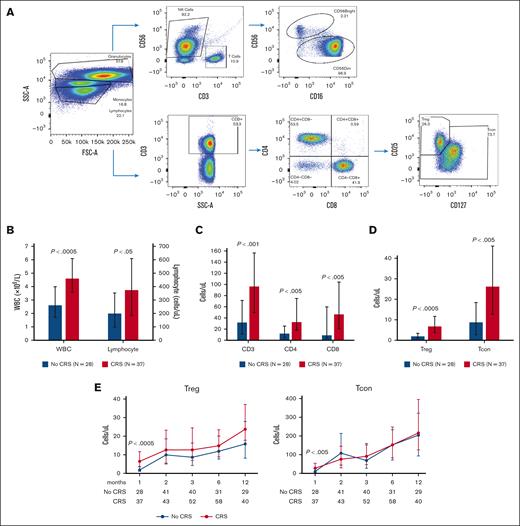
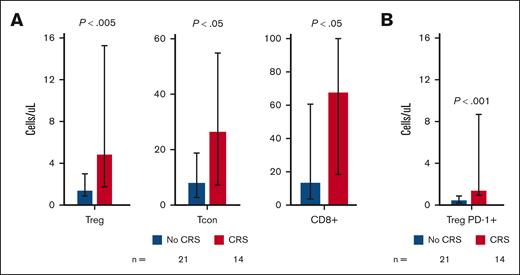
CRS development is associated with a transient increase in T-cell reconstitution
The development of CRS was associated with the attainment of >90% donor chimerism at 1-month after haploidentical HCT in total buffy coat leukocytes (P = .018), granulocyte (P = .02) and T-cell (P = .028) lineages compared with those who did not develop CRS (supplemental Figure 4). To determine whether any of the associations between CRS and clinical outcomes could be related to an effect on immune reconstitution, we compared the flow cytometry defined lymphocyte subsets in patients who developed CRS with those who did not (Figure 3A). Among all patients with HCT, CRS was associated with a higher total white blood cell (P < .0005) and higher total lymphocyte count (P < .05) at 1-month after transplantation (Figure 3B). The absolute numbers of CD3+ T cells (P < .001) and their CD4+ (P < .005) and CD8+ (P < .005) subpopulations were also higher at 1-month after HCT in patients who developed CRS (Figure 3C), although the increase did not persist (Figure 3E; supplemental Figure 5). Among the T-cell subpopulations, the increase in regulatory T cells (Tregs) at 1-month after haploidentical HCT was most significant (P < .0005) (Figure 3D), with both central memory and effector memory Treg subsets increasing in the context of CRS (supplemental Figure 6A). An increase in conventional T cells (Tcon) (P < .005) was also noted at 1-month after HCT in the context of CRS that did not persist (Figures 3D-E). There was no association between the total number of natural killer (NK) cells, the CD56dim NK subset, or the CD56bright NK cell subset, and the development of CRS (supplemental Table 3).
Immune reconstitution posthaploidentical HCT in patients with CRS compared with those without CRS. (A) Flow cytometry schematic of NK cells and T-cell subpopulations. (B) Total white blood cell and lymphocyte counts 1 month after HCT. (C) CD3+, CD4+, and CD8+ T-cell counts at 1-month after HCT. (D) Treg and Tcon counts 1 month after HCT. (E) Longitudinal evaluation of Tregs and Tcon cell populations after HCT. The numbers on the x-axis represent the months after HCT. The number of samples available for flow cytometry evaluation at each time point in each graph is shown. The Wilcoxon rank-sum test was performed for all group comparisons and the Wilcoxon-signed-rank test was performed for all paired comparisons, with all test being 2-sided with a significance level of 0.05. The bars in all plots represent median values, with error bars representing the interquartile range between the 25% and 75% quartiles.
Immune reconstitution posthaploidentical HCT in patients with CRS compared with those without CRS. (A) Flow cytometry schematic of NK cells and T-cell subpopulations. (B) Total white blood cell and lymphocyte counts 1 month after HCT. (C) CD3+, CD4+, and CD8+ T-cell counts at 1-month after HCT. (D) Treg and Tcon counts 1 month after HCT. (E) Longitudinal evaluation of Tregs and Tcon cell populations after HCT. The numbers on the x-axis represent the months after HCT. The number of samples available for flow cytometry evaluation at each time point in each graph is shown. The Wilcoxon rank-sum test was performed for all group comparisons and the Wilcoxon-signed-rank test was performed for all paired comparisons, with all test being 2-sided with a significance level of 0.05. The bars in all plots represent median values, with error bars representing the interquartile range between the 25% and 75% quartiles.
We next evaluated the association between CRS and immune reconstitution after stratification by graft source. Among patients who received BM grafts and developed CRS, we noted a marked increase in the reconstitution of CD4+ T-cell subpopulations, including Treg (P < .005) and Tcon (P < .05), as well as CD8+ T cells (P < .05) at 1-month after transplantation compared with those without CRS (Figure 4A). These patients also had a greater absolute quantity of PD-1+ Treg (P < .001) 1-month after haploidentical HCT than those who did not develop CRS (Figure 4B). As most patients who received PBSC grafts developed CRS, the comparison of immune reconstitution between patients who did and did not develop CRS was limited by the relatively small number of patients in the latter group (supplemental Figure 6B).
Immune reconstitution posthaploidentical HCT with BM grafts in patients with CRS compared with those without CRS. (A) Treg, Tcon, and CD8+ T-cell counts at 1 month after HCT. (B) PD-1+ Treg cell counts at 1-month after transplantation. The number of samples available for flow cytometry evaluation at each time point for each graph is shown. The Wilcoxon rank-sum test was performed for all group comparisons, with all tests being 2-sided with a significance level of 0.05. The bars in all plots represent median values, with error bars representing the interquartile range between the 25% and 75% quartiles.
Immune reconstitution posthaploidentical HCT with BM grafts in patients with CRS compared with those without CRS. (A) Treg, Tcon, and CD8+ T-cell counts at 1 month after HCT. (B) PD-1+ Treg cell counts at 1-month after transplantation. The number of samples available for flow cytometry evaluation at each time point for each graph is shown. The Wilcoxon rank-sum test was performed for all group comparisons, with all tests being 2-sided with a significance level of 0.05. The bars in all plots represent median values, with error bars representing the interquartile range between the 25% and 75% quartiles.
Discussion
Consistent with data from other retrospective studies,3-9 CRS is common after haploidentical HCT. The development of CRS was found to be most strongly associated with PBSC grafts. Interestingly, despite the PBSC grafts having a higher content of CD34+ and TNC cells per kilogram, there was no association between these and CRS. Further investigation is warranted to determine the association between graft content and the development of CRS after haploidentical HCT. Although CRS, which develops in the context of CAR-T therapy, has an association with disease type and burden at the time of adoptive transfer of T cells, disease-related factors had no association with post-HCT CRS. This highlights an important difference between post-HCT and CAR-T–related CRS, namely that disease type and burden play a more diminished role in its development in the former. This is consistent with CAR-T cells often being administered at a high burden of disease, whereas HCT is performed when the disease is in remission. Whether the disease type and burden would have an impact on CRS posthaploidentical HCT if the latter were to be performed with active disease, as with CAR-T therapy, remains unknown.
The data from our center support the association between the development of posthaploidentical HCT CRS and a reduced incidence of relapse. This association was not confounded by disease diagnosis or graft source. This suggests that the association of CRS with less relapse is not driven purely by immune effector cell quantity but may itself have an early effect on reconstituting immune effector populations that could then translate into a later impact on clinical outcomes. This possibility of early cytokine release being associated with later posttransplantation outcomes is further supported by the observation that only 14 of the 81 patients who received a PBSC graft in this cohort did not develop CRS, and none of these 14 patients developed moderate-to-severe chronic GVHD.
The development of CRS was associated with greater early chimerism and T-cell reconstitution after haploidentical HCT. This resulted in a higher absolute quantity of CD4+ Tcon, Treg, and CD8+ T cells at 1 month after HCT in patients who developed CRS compared with those who did not. Enhanced T-cell reconstitution was particularly notable in patients who received BM grafts, which are known to have a lower T-cell content than PBSC grafts.20,21 This suggests that the increased reconstitution of T-cell subpopulations may not be purely a function of T-cell content but may be associated with cytokine release. The relationship between CRS and T-cell reconstitution did not persist beyond the first month, further supporting the hypothesis that the transient release of cytokines early after HCT may have had an early effect on reconstituting T cells. Future work is required to better understand this, including the measurement of specific cytokine levels known to be associated with CRS early after HCT and their association with immune reconstitution. Whether treatment with tocilizumab modifies the association of CRS with immune reconstitution could not be clearly addressed in this cohort because of the small number of tocilizumab-treated patients who had longitudinal immune reconstitution data and are the subject of an ongoing study.
The significance of increased early reconstitution of Tregs in the context of CRS, particularly in patients who received BM grafts, is unclear and requires further study. The PD-1 pathway has been shown to support Treg survival in the context of IL-2 mediated expansion by inhibiting apoptosis, and the expansion of PD-1+ Treg in the context of CRS, most notably among those who received BM grafts, suggests that it may play a similar role in the post-HCT setting.22 It is possible that despite its transience, the early enhanced Treg reconstitution in the context of CRS could have beneficial effects on donor hematopoiesis, as was demonstrated for example in mouse models in which Tregs supported the proliferation of hematopoietic stem cells and improved immune tolerance.22 Alternatively, Treg expansion may be an indirect effect of cytokine secretion from other cells. For example, CD56bright NK cells are known to reconstitute early after posttransplantation cyclophosphamide and have been shown to secrete IL-10,23,24 a cytokine that promotes the generation of functional Tregs.25 Further work is needed to dissect the mechanism of Treg expansion in the context of CRS and its significance.
This study has several important limitations, including its retrospective nature and modest sample size. With respect to the association between CRS and a reduced incidence of post-HCT relapse, disease heterogeneity may bias this association and limit the generalizability of the results. Furthermore, with respect to immune reconstitution data, not all patients in the study had these data available at all evaluated time points, in part because of the interruption of correlative sample collection during the COVID-19 pandemic in 2020. As a result, the relatively small number of tocilizumab-treated patients who had sufficient immune reconstitution data limited our ability to investigate whether treatment of CRS in these patients had an effect on post-HCT outcomes and immune reconstitution. Despite these limitations, the depth of clinical, disease, and graft data collected for this patient cohort as well as the comprehensive evaluation of immune reconstitution provides plausible hypotheses about the potential pathophysiological basis of CRS and its relevance to haploidentical HCT. The latter relevance is underscored not only by associations with HCT outcomes, such as disease relapse and GVHD, but also by association with infection, given that recent data suggest an increased risk of fungal infection in haploidentical patients with HCT who develop CRS.26 Further studies on donor graft content and their association with posthaploidentical HCT CRS are ongoing.
In summary, the development of posthaploidentical HCT CRS was most strongly associated with the use of PBSC grafts but was not independently associated with CD34+ or TNC cell dose in multivariable analysis. CRS was associated with a reduced incidence of relapse, independent of the disease diagnosis or graft source. CRS was also associated with a transiently increased quantity of T-cell subpopulations, particularly Tregs, early after HCT compared with those who did not develop CRS, but this increase did not persist. Further work is needed to measure the concentration of secreted cytokines and explore their potential effects on the subpopulations of reconstituting immune effector cells, which may account for the reduced incidence of relapse and increased incidence of moderate-to-severe chronic GVHD observed in the context of posthaploidentical HCT CRS in this single-center study.
Acknowledgments
The authors are grateful to the patient volunteers who provided their time and samples for all the correlative studies. The authors acknowledge the DFCI/HCC clinical oncology and bone marrow transplantation support staff for continued care of these patients. The authors are grateful to the bone marrow transplant and research coordinators at the Dana-Farber Cancer Institute. The authors are also grateful to the staff in the Jerome Ritz laboratory, who performed flow cytometry on the stem cell products and posttransplantation samples.
Authorship
Contribution: R.M.S., S.N., and R.R. designed the study; R.M.S., H.T.K., and M.A. performed the research; V.T.H. contributed to the clinical data; S.N. and J.R. contributed to the graft content and longitudinal flow cytometry data; H.T.K. performed the statistical analysis; R.M.S., S.N., and R.R. interpreted the data; R.M.S. wrote the manuscript; R.R., S.N., H.T.K., R.J.S., and C.J.W. reviewed the manuscript and provided critical input in the preparation of the final draft; and all authors were involved in revising the manuscript critically for important intellectual content, provided final approval of the manuscript, and agreed to be accountable for all aspects of the work.
Conflict-of-interest disclosure: C.S.C. consults or is on the advisory board of Sanofi, CSL Behring, Incyte, Mallinckrodt, InhibRx, Cellarity, Astellas, Rigel, and Cimeio. J.K. reports research support from Amgen, Equillium, Bristol Myers Squibb, Miltenyi Biotec, Regeneron, and Clinigen; consulting income from Amgen, Equillium, and Moderna Therapeutics; and is a scientific advisory board member for Cugene and Therakos. S.N. reports ad hoc advisory boards for Kite/Gilead, GlaxoSmithKline, Iovance, A2 Bio, and Sobi. J.R. received research funding from Equillium, Kite Pharma, Novartis, and Oncternal, and served on advisory boards for Akron, Avrobio, Clade, Garuda, LifeVault, Novartis, Rheos, Smart Immune, Talaris, and TScan. C.J.W. holds equity in BioNTech and receives research funding from Pharmacyclics. R.J.S. serves on the board of directors for Be The Match/National Marrow Donor Program; has provided consultancy for Vor Biopharma, Neovii, CSL Behring, Bluesphere Bio, Cugene, Jasper, and Smart Immune; and is on the data safety monitoring board for Juno Therapeutics. R.R. receives funding from the Parker Institute for Cancer Immunotherapy, CRISPR Therapeutics, and Skyline Therapeutics, and is on the advisory board of Glycostem. The remaining authors declare no competing financial interests.
Correspondence: Roman M. Shapiro, Department of Medical Oncology, Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA; e-mail: Roman_shapiro@dfci.harvard.edu; and Rizwan Romee, Department of Medical Oncology, Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA; e-mail: Rizwan_romee@dfci.harvard.edu.
References
Author notes
∗S.N. and R.R. are joint senior authors.
All data in this manuscript are retrospective. Individual participant data will not be shared.
Data are available upon request from the corresponding authors, Roman M. Shapiro (Roman_shapiro@dfci.harvard.edu) and Rizwan Romee (Rizwan_romee@dfci.harvard.edu).
The full-text version of this article contains a data supplement.