TO THE EDITOR:
More than 55 000 people die annually from hematologic malignancies in the United States.1 They frequently receive aggressive care toward the end of life and are more likely to die in a hospital compared with those with solid tumors.2,3 Appropriate care is dependent on a health care infrastructure that considers the relevant needs for this population. Approximately 46 million Americans (15% of US population) live in rural areas with notable gaps in health care funding and access to hospice care. We investigated rural-urban disparities in place of death (POD) for individuals dying from hematologic malignancies in the United States.
We queried the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) database to analyze all deaths from hematologic malignancies (International Classification of Diseases C81-96, D45-47) from 2003 (first year of available nationwide hospice deaths) to 2019.4 CDC WONDER is a publicly available online database for analyzing public health data, including population estimates and deaths across several categories, previously used to study national trends in hospice use.5,6 A population classification was created using the National Center for Health Statistics Urban-Rural Classification Scheme included in the database. These classifications included large metropolitan (≥1 million), small- or medium-sized metropolitan (50 000-999 999), and rural areas (<50 000).7
We estimated the percent of deaths occurring each year in medical, hospice, and nursing facilities, and at home by geographic region. Deaths in a location specified as “other” or unknown were excluded. Odds ratios (OR) for the association between POD and geographic region were calculated using multinomial regression, adjusting for year of death. Differential changes in POD over time by geographic region were assessed with interaction tests. We calculated yearly age-adjusted mortality rates (AAMRs) and stratified results by age (<25, 25-65, and ≥65 years), sex, and race/ethnicity (Hispanic, non-Hispanic White, and non-Hispanic Black). We estimated annual percentage changes (APC) in AAMR using a robust linear regression model of the log-scale AAMR, including population size asweights. Differential changes in APC between geographic regions within subgroups and between subgroups across all regions were examined with interaction tests. Owing to use of publicly available and deidentified data, this study was considered exempt from Institutional Review Board approval. Analyses were completed using R version 4.0.3.8
From 2003 to 2019, there were a total 1 009 717 deaths from hematologic malignancies in the United States, predominantly in large (49.7%), followed by small or medium metropolitan (31.8%) and rural areas (18.5%). Region-specific trends in POD are noted in Table 1.
Number of deaths due to hematologic malignancy in 2003 to 2019, overall and by geographic area
| . | Large metropolitan . | Medium/small metropolitan . | Rural metropolitan . | . | . |
|---|---|---|---|---|---|
| . | N = 501 894 (49.7%) . | N = 320 923 (31.8%) . | N = 186 900 (18.5%) . | OR (95% CI)*,† . | OR (95% CI)*,‡ . |
| POD, no. (%) | |||||
| Medical facility | 240 935 (48.0) | 136 851 (42.6) | 83 096 (44.5) | 1.00 (ref) | 1.00 (ref) |
| Home | 155 390 (31.0) | 106 053 (33.0) | 62 139 (33.2) | 0.86 (0.85, 0.87) | 1.04 (1.02, 1.05) |
| Hospice | 41 681 (8.3) | 30 576 (9.5) | 8658 (4.6) | 1.66 (1.64, 1.67) | 2.14 (2.12, 2.16) |
| Nursing facility | 63 888 (12.7) | 47 443 (14.8) | 33 007 (17.7) | 0.67 (0.66, 0.67) | 0.87 (0.87, 0.88) |
| . | Large metropolitan . | Medium/small metropolitan . | Rural metropolitan . | . | . |
|---|---|---|---|---|---|
| . | N = 501 894 (49.7%) . | N = 320 923 (31.8%) . | N = 186 900 (18.5%) . | OR (95% CI)*,† . | OR (95% CI)*,‡ . |
| POD, no. (%) | |||||
| Medical facility | 240 935 (48.0) | 136 851 (42.6) | 83 096 (44.5) | 1.00 (ref) | 1.00 (ref) |
| Home | 155 390 (31.0) | 106 053 (33.0) | 62 139 (33.2) | 0.86 (0.85, 0.87) | 1.04 (1.02, 1.05) |
| Hospice | 41 681 (8.3) | 30 576 (9.5) | 8658 (4.6) | 1.66 (1.64, 1.67) | 2.14 (2.12, 2.16) |
| Nursing facility | 63 888 (12.7) | 47 443 (14.8) | 33 007 (17.7) | 0.67 (0.66, 0.67) | 0.87 (0.87, 0.88) |
Authors’ analysis of sites of death by rural-urban classification utilizing CDC WONDER database. ORs for the association between geographic region and POD from multinomial regression (top panel), adjusting for year of death are noted.
Odds of dying at home, in hospice, or in a nursing facility compared with a medical facility for large metropolitan areas vs rural areas.
All ORs were significant at P < .0001.
Odds of dying at home, in hospice, or in a nursing facility compared with a medical facility for medium/small metropolitan areas vs rural areas.
Compared with rural areas, deaths in hospice facility were more likely than in a medical facility for large metropolitan (OR, 1.66; 95% confidence interval [CI], 1.64, 1.67) and medium/small metropolitan (OR, 2.14; 95% CI, 2.12, 2.16), whereas deaths in a nursing facility were less likely than in a medical facility for large metropolitan (OR, 0.67; 95% CI, 0.66, 0.67) and medium/small metropolitan (OR, 0.87; 95% CI, 0.86, 0.87). Compared with rural areas, deaths at home were less likely than in a medical facility for large metropolitan (OR, 0.86; 95% CI, 0.87, 0.88) and similar for medium/small metropolitan (OR, 1.04; 95% CI, 1.02, 1.05).
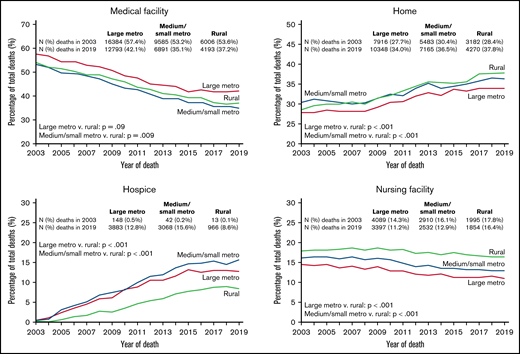
In 2019, the most recent year surveyed, 8.6% of deaths in rural areas occurred in a hospice facility, compared with 15.6% and 12.8% in a small/medium and large metropolitan area, respectively (Figure 1). A higher proportion of deaths in rural areas in 2019 occurred in a nursing facility, compared with small/medium and large metropolitan areas (16.4% vs 12.9% and 11.2%, respectively). The same pattern was true for deaths at home (37.8% vs 36.5% and 34.0%, respectively). Trends over time are noted in Figure 1.
Variation in POD by rural-urban areas for hematologic malignancies from 2003 to 2019. Authors’ analysis of sites of death by rural-urban classification utilizing representative data from the US Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database shows the change in the proportion of deaths in each location over time and separately according to geographical location. Noted P-values are tests of interaction between geographical region and time (year) in the probability of death in a given location.
Variation in POD by rural-urban areas for hematologic malignancies from 2003 to 2019. Authors’ analysis of sites of death by rural-urban classification utilizing representative data from the US Centers for Disease Control and Prevention Wide-Ranging Online Data for Epidemiologic Research (CDC WONDER) database shows the change in the proportion of deaths in each location over time and separately according to geographical location. Noted P-values are tests of interaction between geographical region and time (year) in the probability of death in a given location.
From 2003 to 2019, AAMRs declined across all sites from 21.8 to 16.7 (APC, −1.48; 95% CI, −1.60, −1.36) (supplemental Table 1). APCs between the geographic regions did not differ significantly overall, nor within any subgroup defined by sex, race/ethnicity, or <25 and >65 age groups. In the 25 to 65 age group, the improvement in AAMR over time was significantly lower in rural (APC, −2.33) compared with large metropolitan areas (APC, −2.80; P < .001)
Despite similar improvements in mortality over time across rural and urban areas, we demonstrate end-of-life disparities in patients with hematologic malignancies, with those living in rural areas having a lower likelihood of death in a hospice facility and a higher likelihood in a nursing facility.
Although a majority of patients report a preference to die at home, discordance with POD is common, and reflective of patient factors, such as income, preferences, and caregiver support,9,10 as well as larger infrastructural and geographic barriers contributing to disparities in hospice uptake. These include financial constraints (inadequate Medicare/Medicaid reimbursement for hospice services, high operational costs in running facilities not at capacity), topographical barriers (proximity to nearest facility or between homes for hospice services administered at home, inadequate road maintenance, seasonal changes, slower broadband and phone services), and lack of support infrastructure (staffing shortages, education and retention, ambulance availability, grief and bereavement services).11,12 Such challenges add to the medical complexity of all patients, but especially those with hematologic malignancies who experience high symptom burden and transfusion needs near the end of life.13,14
Larger share of deaths at home in rural areas may reflect stronger family ties and capacity to care for loved ones at home.2 However, we interpret with caution. Although hospice may be provided in other locations, significant caregiving and financial resources are often required to optimally support patients’ needs at home even with the Medicare Hospice Benefit.15 Adequate access to end-of-life care in a dedicated inpatient hospice facility costs more than routine home hospice and requires documented symptom burden for Medicare coverage. Many patients toward the end of life may be admitted to critical access hospitals in rural areas where traditional Medicare is instead billed.12 This may also result in a higher number of rural residents dying in nursing facilities where quality of care received at end of life may not be comparable to that provided by trained hospice clinicians.16 Furthermore, there are increasing nursing home closures in rural areas.17 These inequities may be exacerbated in rural populations where self-employment is common, rates of employee-sponsored insurance and paid medical leave may be lower, and many remain Medicaid ineligible.11
To investigate if recent improvements in cancer outcomes apply equally to all geographic areas, our study investigated mortality rates and did not observe a corresponding higher mortality rate in rural areas compared with urban metropolitan areas, a trend noted with other diseases in the United States.18 Considering the complex treatment planning, most patients diagnosed with a hematological malignancy may be referred to a local cancer center that specializes in the treatment of such diseases and may mitigate disparities that may otherwise exist.
Our analysis is limited by lack of information on income and insurance that may dictate access to resources. The database also lacks clinical details relevant to hospice uptake, including cancer diagnosis, therapies received, patient preferences, rate of functional decline, presence of a caregiver, and hospice use in other settings. In addition, we are unable to account for physical function, cognitive status, and timeliness of physician referral to hospice. Other limitations include potential errors of documentation of race/ethnicity and cause of death on death certificates.
Rural health infrastructure has been aggravated by facility closures especially in the previous 2 years during the COVID-19 pandemic. With ongoing congressional debate on Medicare Part B reimbursement for hospice care that will allow for billing Medicare separately for visits to patients enrolled in hospice care,19 and discussions of a retooled Build Back Better Act that could reinvest millions in state-led expansion of rural health care, we hope this study informs better deployment of palliative care resources for those living in rural areas.
Contribution: S.M.Q.H., A.L.B., A.G., and T.W.L.B. conceived, designed, and analyzed the study and interpretated the data; and S.M.Q.H., A.L.B., A.G., R.S., S.H.C., H.J.W., and T.W.L.B. drafted, revised, and approved the final draft.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Thomas W. LeBlanc, Cancer Control & Population Sciences, Duke Cancer Institute, Duke University, 2424 Erwin Rd, Durham, NC 27705; e-mail: thomas.leblanc@duke.edu.
References
Author notes
Presented in abstract form at the 63rd annual meeting of the American Society of Hematology in December 2021 in Atlanta, GA.
For data sharing, contact the corresponding author: thomas.leblanc@duke.edu.
The full-text version of this article contains a data supplement.