TO THE EDITOR:
Early diagnosis and effective use of disease-modifying and curative therapies have resulted in ≥93% of youth with sickle cell disease (SCD) living into adulthood with less disease morbidity.1 Consequently, reproductive health (including fertility, contraception, and preimplantation genetic testing) is an emerging area of importance in this population.2-5 Specifically in males with SCD, fertility can be diminished by many factors, including priapism, anemia, hypogonadism, and testicular infarction from the disease and/or antineoplastic treatments, such as hydroxyurea.2 Long-standing and recent research shows that semen abnormalities occur in males with SCD across the life course, including studies that show impaired semen parameters at baseline in adult males, which further decline after starting hydroxyurea6 ; abnormal semen parameters in adolescents and young adults (AYAs) irrespective of hydroxyurea treatment7 ; and reduced spermatogonial cell counts in prepubertal boys who received hydroxyurea.8
National organizations (eg, the American Academy of Pediatrics) are urging providers to counsel at-risk SCD patients to optimize reproductive outcomes.9 Experts also recommend fertility testing (ie, semen analysis) in male AYAs with SCD,10 yet specific guidelines have not been developed. There are limited data on male AYAs with SCD and their caregivers’ perspectives on providing semen samples for testing. This information is critical, as AYAs with SCD may face multiple barriers to obtaining testing and to fertility-related decision-making. AYAs with SCD frequently have poor access to health care11-13 that may limit their opportunities to learn about and obtain testing, compromise their understanding and use of fertility information, and prevent them from getting testing that is not covered under insurance laws in many states.14 These factors may be particularly impactful as AYAs become increasingly independent, develop life goals, and transition to adult care where they will make their own treatment decisions.15
In this context, a small pilot study approved by Nationwide Children’s Hospital's Institutional Review Board was conducted to examine knowledge and perspectives on fertility testing among male AYAs (14-21 years) with SCD and caregivers of the participating males at a large, midwestern pediatric academic medical center. English-speaking patients were approached during clinic visits and excluded if they had a preexisting developmental or cognitive deficit that would preclude their ability to independently complete electronic surveys or if they had previously undergone hematopoietic stem cell transplantation. After informed consent (assent, if <18 years of age) was obtained, participants completed the Fertility Knowledge and Attitudes Questionnaire (FKAQ), a survey developed by the research team. The FKAQ was based on constructs from the Health Belief Model (eg, perceived risk of infertility and benefits and barriers to fertility testing) and items from prior fertility-related studies among male AYAs with SCD,16 varicocele,17 and cancer18 and was refined after piloting it with an AYA and a caregiver from the SCD community. Participants completed 23 to 30 FKAQ items with branching logic (29 multiple choice, 1 open-ended) examining sociodemographic factors, parenthood goals, fertility-related knowledge, and factors influencing interest in fertility testing; they were compensated with a $10 gift card. Electronic medical records were reviewed to confirm SCD genotype and identify those who had been prescribed hydroxyurea.
Statistical analyses were conducted with SPSS (version 25.0).19 Descriptive statistics summarized the sample (Table 1). Fisher’s exact tests were used to examine the relationship between sociodemographic characteristics, fertility-related knowledge, and perspectives on fertility testing. Because of our small sample size, sociodemographic characteristics were analyzed as categorical variables: AYA age (<18 vs ≥18 years), caregiver-reported household income (≤$35,000 vs >$35,000), and caregiver educational attainment (less than an associate’s/bachelor’s degree vs an associate’s/bachelor’s degree and higher).
AYAs’ and caregivers’ demographics and responses to selected items on the FKAQ
| . | AYAs, n = 20 . | Caregivers, n= 15 . |
|---|---|---|
| . | n (%) . | n (%) . |
| Demographics | ||
| Genotype | ||
| Hemoglobin SS/SB0 | 14 (70) | — |
| Hemoglobin SC/SB+ | 6 (30) | — |
| Median Age (IQR) | 16.5 (5) | — |
| Relationship status | ||
| Single | 19 (95) | 5 (33) |
| Serious relationship/marriage | 1 (5) | 10 (67) |
| Race* | ||
| Black/African American | 17 (85) | 11 (73) |
| African | 4 (20) | 2 (13) |
| White | 1 (5) | 1 (7) |
| Asian | 2 (10) | |
| Other | 1 (7) | |
| Education | ||
| Less than an associate's/ bachelor’s degree | — | 10 (67) |
| Associate's/bachelor’s or higher degree | — | 5 (33) |
| Household income | ||
| ≤$35,000 | — | 7 (47) |
| >$35,000 | — | 7 (47) |
| Not reported | — | 1 (7) |
| FKAQ knowledge items† | ||
| 1. I received information about my (my son’s) fertility (the ability to have a biological child) from my sickle cell provider. | 9 of 18 (50) | 9 of 15 (60) |
| 2. I received information about my (my son’s) fertility (the ability to have a biological child) from my parents (my family). | 7 of 18 (39) | 3 of 15 (20) |
| 3. I received information about my (my son’s) fertility (the ability to have a biological child) from the media or Internet. | 3 of 18 (17) | 2 of 14 (14) |
| 4. My (my son’s) sickle cell disease might make it difficult for me (him) to have a biological child in the future. | 4 of 19 (21) | 4 of 15 (27) |
| 5. The treatment I (my son) receive/received for my (my son's) sickle cell disease might make it difficult for me (him) to have a biological child in the future. | 2 of 19 (11) | 1 of 15 (7) |
| 6. I would like more information about how sickle cell disease and its treatment could affect my (my son’s) ability to have a biological child. | 13 of 18 (72) | 9 of 15 (60) |
| 7. I have enough knowledge about my (my son’s) fertility (ability to have a biological child). | 4 of 19 (21) | 7 of 15 (47) |
| Testing interest/barriers | ||
| 8. Do you know what semen analysis (or sperm analysis) is? | 6 of 20 (30) | 3 of 15 (20) |
| 9. Do you know how a semen (or sperm) sample is collected? | 7 of 20 (35) | 7 of 15 (47) |
| . | AYAs, n = 20 . | Caregivers, n= 15 . |
|---|---|---|
| . | n (%) . | n (%) . |
| Demographics | ||
| Genotype | ||
| Hemoglobin SS/SB0 | 14 (70) | — |
| Hemoglobin SC/SB+ | 6 (30) | — |
| Median Age (IQR) | 16.5 (5) | — |
| Relationship status | ||
| Single | 19 (95) | 5 (33) |
| Serious relationship/marriage | 1 (5) | 10 (67) |
| Race* | ||
| Black/African American | 17 (85) | 11 (73) |
| African | 4 (20) | 2 (13) |
| White | 1 (5) | 1 (7) |
| Asian | 2 (10) | |
| Other | 1 (7) | |
| Education | ||
| Less than an associate's/ bachelor’s degree | — | 10 (67) |
| Associate's/bachelor’s or higher degree | — | 5 (33) |
| Household income | ||
| ≤$35,000 | — | 7 (47) |
| >$35,000 | — | 7 (47) |
| Not reported | — | 1 (7) |
| FKAQ knowledge items† | ||
| 1. I received information about my (my son’s) fertility (the ability to have a biological child) from my sickle cell provider. | 9 of 18 (50) | 9 of 15 (60) |
| 2. I received information about my (my son’s) fertility (the ability to have a biological child) from my parents (my family). | 7 of 18 (39) | 3 of 15 (20) |
| 3. I received information about my (my son’s) fertility (the ability to have a biological child) from the media or Internet. | 3 of 18 (17) | 2 of 14 (14) |
| 4. My (my son’s) sickle cell disease might make it difficult for me (him) to have a biological child in the future. | 4 of 19 (21) | 4 of 15 (27) |
| 5. The treatment I (my son) receive/received for my (my son's) sickle cell disease might make it difficult for me (him) to have a biological child in the future. | 2 of 19 (11) | 1 of 15 (7) |
| 6. I would like more information about how sickle cell disease and its treatment could affect my (my son’s) ability to have a biological child. | 13 of 18 (72) | 9 of 15 (60) |
| 7. I have enough knowledge about my (my son’s) fertility (ability to have a biological child). | 4 of 19 (21) | 7 of 15 (47) |
| Testing interest/barriers | ||
| 8. Do you know what semen analysis (or sperm analysis) is? | 6 of 20 (30) | 3 of 15 (20) |
| 9. Do you know how a semen (or sperm) sample is collected? | 7 of 20 (35) | 7 of 15 (47) |
Participants had the option to select all that apply for this category.
Data are the proportion (%) of AYAs and caregivers who responded “yes.”
Of 40 eligible AYAs, 22 completed clinic visits during the study time frame; 20 AYAs (91% of those approached) and 15 caregivers enrolled. Eighty-five percent of AYA participants agreed/strongly agreed that they wanted a biological child in the future, whereas 60% of enrolled caregivers believed their son was interested in having a biological child. AYAs and caregivers frequently responded incorrectly or with uncertainty to the FKAQ items assessing fertility-related knowledge (Table 1); 35% of AYAs and 47% of caregivers expressed unfamiliarity with how to obtain a semen sample and 30% of AYAs and 20% of caregivers expressed unfamiliarity with its purpose. Results of Fisher’s exact tests used to examine age, income, and education were not significant overall, except for an association between older AYA age and knowledge that SCD could make it more difficult to have a biological child (p = .02).
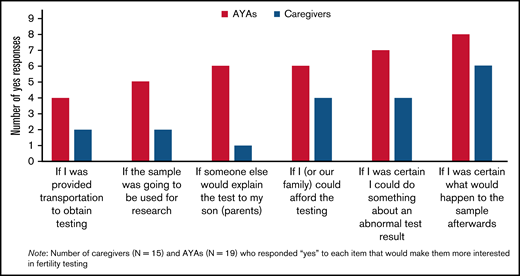
When asked about interest in testing, 37% of AYAs and 33% of caregivers reported an interest in obtaining a semen analysis, 11% of AYAs and 40% of caregivers were not interested, and 52% of AYAs and 27% of caregivers were unsure. AYAs and caregivers reported factors that would increase their interest in testing (Figure 1). Regarding procedures for providing the sample, the most preferred option among AYAs (45%) was “in a private place in the hospital and to have our family transport it to the testing center” (rather than producing the sample “at home” or “at the testing center” and “having someone else transport it to the testing center”).
Factors increasing reported interest in fertility testing among AYAs and caregivers. The x-axis represents response options asked of participants in the survey. Participants were asked to respond “yes” or “no” if the item would make them more interested in fertility testing. The y-axis represents the number of “yes” responses from caregivers and AYAs for each item. Shown on the y-axis are the number of caregivers (n = 15) and AYAs (n = 19) who responded to each item that would make them more interested in fertility testing.
Factors increasing reported interest in fertility testing among AYAs and caregivers. The x-axis represents response options asked of participants in the survey. Participants were asked to respond “yes” or “no” if the item would make them more interested in fertility testing. The y-axis represents the number of “yes” responses from caregivers and AYAs for each item. Shown on the y-axis are the number of caregivers (n = 15) and AYAs (n = 19) who responded to each item that would make them more interested in fertility testing.
As most AYAs and caregivers reported a desire for biological parenthood and prior research shows that adult men with SCD opt to bank sperm before initiating hydroxyurea,6 the unfamiliarity with fertility testing processes and other fertility-related knowledge gaps among AYAs and their caregivers are concerning. Many study participants were unsure about pursuing testing, potentially because of the lack of fertility knowledge and/or future-oriented thinking during adolescence. These findings suggest tailored fertility-focused education programs and inclusion of fertility-related topics into multidisciplinary SCD care are needed starting in early adolescence, especially considering that many AYAs do not receive this information from their providers (perhaps because providers want to avoid raising concerns that may negatively affect hydroxyurea initiation).20,21 Topics to be prioritized include fertility impacts of SCD and its treatments and information about fertility testing (eg, how to obtain a sample; purpose, cost, and interpretation; and what happens to the sample after collection) that we identified may increase AYA and caregiver interest in testing. Conversations with families should highlight known and unknown fertility-related impacts of SCD and treatments like hydroxyurea, to promote autonomy, facilitate shared decision-making, and minimize future regret.9
In addition to providing fertility-related information, study findings highlight the need to facilitate testing by ensuring that semen samples can be produced in a variety of settings. It is important to implement interventions to address structural barriers, such as navigating testing at an offsite fertility center and cost. Lastly, the findings showed differences in AYA and caregiver fertility-based knowledge and perspectives, demonstrating the potential need to facilitate these discussions between AYAs and their caregivers, given research showing AYA reliance on caregivers for assistance with medical decision-making.22 Considering the limitations of this small sample at a single site, larger multisite studies are needed to confirm and expand on these findings. Ultimately, studies examining semen parameters at earlier time points and longitudinally are needed to understand how to address fertility impairment in this population.
In summary, a developmentally appropriate and inclusive approach to creating fertility-related educational materials and addressing fertility testing barriers is critical for this population, given low health literacy considerations23 and limited health care access.24 Future programming should also be easily accessible, engaging, culturally relevant, and self-directed, given the sensitive nature of the information. Addressing fertility knowledge gaps and barriers, conducting definitive fertility studies in younger patients, and expanding provider training in fertility25 are needed to achieve equitable fertility health care for AYAs with SCD.
Acknowledgments: L.N. received National Institutes of Health, National Cancer Institute grant K08CA237338.
Contribution: S.E.C., L.N., and G.P.Q. designed the study; S.E.C. and L.N. served equally as principal investigators; C.J.S., L.N., C.I.T., and S.E.C. coordinated the project; C.I.T. and C.J.S. recruited the participants; C.I.T., C.J.S., and A.L.O. analyzed the data; L.N., C.I.T., C.J.S., and S.E.C. contributed to writing the first draft; and all authors contributed to revision of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Leena Nahata, Abigail Wexner Research Institute at Nationwide Children’s Hospital, 431 South 18th St, Columbus, OH 43205; e-mail: leena.nahata@nationwidechildrens.org.
References
Author notes
Protocols and deidentified data sets will be made available upon email request to the corresponding author (leena.nahata@nationwidechildrens.org).