Key Points
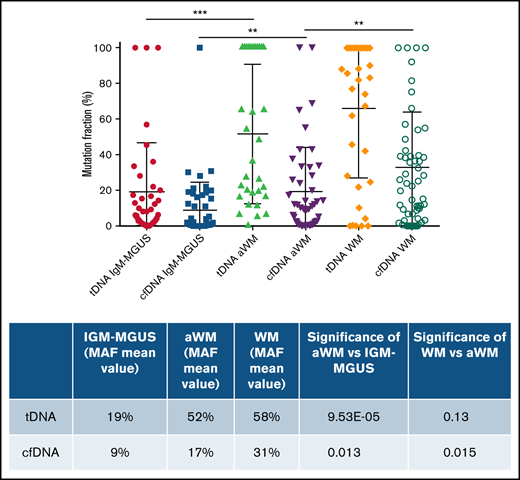
Quantitative evaluation of the tumor load in patients with IgM monoclonal gammopathies in tDNA and cfDNA samples.
Abstract
We describe a novel method for the detection of MYD88L265P mutation using a competitive allele-specific polymerase chain reaction (Cast-PCR) assay. This assay has a sensitivity of 1 × 10−3, is applicable in reactions containing very low amounts of DNA (as low as 20 pg), and allowed the detection of MYD88L265P somatic mutation in both tumor-derived DNA (tDNA) and cell-free DNA (cfDNA). In addition, using the Cast-PCR assay, we were able to determine the mutation allele fraction (MAF) in each tested sample. We then analyzed baseline tDNA and cfDNA samples from 163 patients (53 with immunoglobulin M monoclonal gammopathy of undetermined significance and 110 with Waldenström’s macroglobulinemia [WM], of whom 54 were asymptomatic and 56 were symptomatic) and also in sequential samples of 37 patients. MAF in both cfDNA and tDNA was higher among patients with symptomatic compared with asymptomatic WM and in those with asymptomatic WM compared with those with immunoglobulin M (IgM) monoclonal gammopathy of undetermined significance. In addition, the evaluation of sequential samples showed that MAF decreased after treatment, whereas it increased in patients who relapsed or progressed to symptomatic WM. Thus, Cast-PCR is a highly sensitive, cost-effective diagnostic tool for MYD88L265P detection, applicable in both tDNA and cfDNA samples, that also provides a quantitative evaluation of the tumor load in patients with IgM monoclonal gammopathies.
Introduction
Activating MYD88 mutations are present in 95% of patients with Waldenström’s macroglobulinemia (WM),1 and the presence of MYD88L265P, although it may also occur in other lymphoproliferative neoplasms, is considered one of the major findings that can aid the diagnosis of WM, thus making it important in the differential diagnostic workup.2-4 Beyond its value for the diagnosis of WM, the activating amino acid substitution p.Leu265Pro leads to the upregulation of HCK transcription, a SRC family member that triggers pro-survival Bruton’s tyrosine kinase (BTK), AKT, and ERK 1/2 signaling.5,6 Importantly, both BTK and hematopoietic cell kinase are blocked by specific BTK inhibitors such as ibrutinib, and these drugs are highly active in the treatment of patients with MYD88L265P but probably less active in patients with MYD88WT WM.6-9 The MYD88L265P mutation is also present in 50% to 60% of patients with immunoglobulin M monoclonal gammopathies of undetermined significance (IgM-MGUS), a preneoplastic asymptomatic condition, and has been associated with higher risk of progression to WM in some series10,11 ; however, due to the low burden of clonal cells in this condition, its presence may be underestimated. Thus, detection of MYD88L265P is of clinical relevance both for diagnostic and treatment purposes.
Currently used methods to detect MYD88L265P mutation most often involve allele-specific polymerase chain reaction (AS-PCR) and Sanger sequencing or use of next-generation sequencing–based protocols in bone marrow (BM) aspirates or biopsy of patients with IgM monoclonal gammopathies. AS-PCR is mainly used for the detection of MYD88L265P mutations on CD19-sorted BM samples; however, it provides a qualitative rather than a quantitative result. A recent study by Drandi et al12 indicated that droplet digital PCR (ddPCR) is a sensitive tool for mutation screening; however, it raises the issue of a costly instrument accompanied by expensive consumables, which makes it challenging to use in everyday practice.
We recently evaluated the role of peripheral blood (PB) cell-free DNA (cfDNA) in characterizing the mutational status of MYD88 and CXCR4 as a tool for noninvasive screening of patients with IgM monoclonal gammopathies.13,14 In continuation, we now describe a newly developed, highly sensitive, cost-effective competitive allele-specific quantitative real time PCR assay (Cast-PCR) for the identification of MYD88L265P mutation in BM and PB samples from patients with IgM monoclonal gammopathies; this assay can be easily applied in a typical real-time PCR protocol as part of routine clinical evaluation. Furthermore, with this assay, we were able to determine the mutation allele fraction (MAF) in both tumor-derived DNA (tDNA) and cfDNA of each patient and to assess MAF in sequential samples as a tool for noninvasive molecular evaluation of tumor burden and disease monitoring.
Methods
Sample collection and processing
PB (10-12 mL) and BM (5-10 mL) aspirates were collected from 163 patients (53 with IgM MGUS, 54 with asymptomatic WM [aWM], and 56 with symptomatic WM [sWM]) as well as 10 patients with multiple myeloma who were used as negative control subjects. We also used PB from 5 healthy donors as additional negative control subjects. All patients provided a written consent form for the collection and analysis of their biological samples according to the Declaration of Helsinki. The research was approved by the Institutional Review Board/Scientific committee of “Alexandra” Hospital.
PB was collected in EDTA tubes and was processed within 2 hours for DNA extraction using the QiaAmp circulating nucleic acid kit (Qiagen, Valencia, CA) according to manufacturer’s instructions. The quantity of cfDNA was measured by the Qubit fluorometer using the high-sensitivity double-stranded DNA kit (Thermo Fisher Scientific, Waltham, MA). BM aspirates were collected at the same time with PB and were processed for CD19 enrichment, as previously described.13 Briefly, mononuclear cells from BM aspirates were isolated by lysis buffer (BD PharmLyse buffer, BD Biosciences, San Jose, CA) followed by positive selection using CD19 magnetic beads (AutoMacs, Miltenyi Biotech, Bergisch Gladbach, Germany). DNA of the CD19+ BM selected cells (tDNA) was extracted by using the AllPrep DNA/RNA Mini Kit (QIAGEN, Valencia, CA) and quantified by using the high-sensitivity double-stranded DNA kit.
For positive control, MWCL1 and BCWM1 WM cell lines were used, which were kindly provided by Steven Treon (Bing Center for Waldenström's Macroglobulinemia Research, Boston, MA). For negative control, multiple myeloma cell lines U266 (TIB 196), H929 (CRL-9068), and RPMI 8226 (CCL-155) were used (purchased from ATCC, Manassas, VA). Also, ovarian cancer cell lines ES2 and TOV21G were used as negative controls, which were a kind gift from A. Scorilas (National and Kapodistrian University of Athens, Athens, Greece).
Cast TaqMan-PCR (Cast-PCR)
Standard AS-PCR
For the detection of MYD88L265P mutation, tDNA and cfDNA samples were also analyzed by AS-PCR using MYD88L265P (FAM-labeled) and MYD88WT predesigned (VIC-labeled) probes (Thermo Fisher Scientific). Master mixes were prepared according to the manufacturer’s instructions and distributed in 96-well plates; the reaction was conducted in the StepOne Real-Time PCR system. Thermal cycling conditions were as follows: 10 minutes at 95°C followed by 40 cycles of amplification using 15 seconds at 95°C and 60 seconds at 60°C, with a subsequent 1-minute extension at 60°C. Real-time data were collected during the last 40 cycles of amplification and analyzed by using the StepOne PCR software.
ddPCR assay
To validate our results, we analyzed tDNA and cfDNA samples for MYD88L265P using ddPCR. All samples were analyzed by using TaqMan hydrolysis probes for detecting and quantifying MYD88WT (HEX-labeled) and MYD88L265P (FAM-labeled) as previously reported.15 Master mixes were prepared according to the manufacturer’s instructions, and the cycling profile was as follows: 95°C for 10 minutes (1 cycle), 94°C for 30 seconds, and 60°C for 60 seconds (39 cycles), plus a final incubation time of 10 minutes at 98°C and infinite hold at 12°C. Each experimental procedure included a negative control (non-template control) and a positive control (MWCL1 cell line), which contained enough mutant and wild‐type DNA to create a double‐positive cluster of >100 droplets. PCR products were loaded onto the QX200 Droplet Reader (Bio‐Rad, Hercules, CA), and the data were analyzed with QuantaSoft Software (version 1.7.4, Bio-Rad).
Statistical analysis
Experiments were performed in duplicate or triplicate (for each biological replicate, n ≥ 2). Associations between variables were analyzed with Fisher’s exact test. Correlation of MAF (cfDNA and tDNA) and BM infiltration was assessed by using Pearson’s correlation. All other comparisons were assessed by using the Mann-Whitney U test. MAF of MYD88L265P is expressed as percentage. GraphPad Prism 5.0 software (GraphPad Software, La Jolla, CA) was used for this part of the statistical analysis. Performance statistics for each method, as well as Fisher’s exact test, to examine the significance of the association between Cast-PCR, AS-PCR and ddPCR, were computed by using R version 4.1.1 (R Foundation for Statistical Computing, Vienna, Austria). Confidence intervals (95% CIs) were obtained for sensitivity, specificity, and accuracy with the Clopper-Pearson method and for the likelihood ratios using the “log method.”16 For the predictive values, the CIs are the standard logit CIs.17 All P values were estimated with the conventional 5% significance level.
Results
Patients
Overall, 249 samples of tDNA and cfDNA from 163 patients were analyzed (53 with IgM MGUS, 54 with aWM, and 56 with sWM). Forty-five sequential samples were available from 37 patients: in 4 patients who progressed from aWM to sWM, in 9 aWM patients as follow-up, and in 32 sWM patients before and after therapy. The patients’ clinical features are summarized in Table 1.
Patient characteristics
| IgM patients (n) . | 163 . |
|---|---|
| IgM MGUS | 53 |
| aWM | 54 |
| Newly diagnosed sWM | 41 |
| WM in relapse | 3 |
| WM during therapy and in remission | 1 |
| WM during therapy and in stable disease | 2 |
| WM posttherapy and in remission | 8 |
| WM posttherapy and in stable disease | 1 |
| Kappa/lambda | 116/47 |
| Age, median (range), y | 69 (34-92) |
| BM infiltration, median (range), % | 20 (0-95) |
| IgM levels, median (range), mg/dL | 1050 (18-10 800) |
| Treatment | 44 |
| DRC | 30 (69%) |
| FCR | 1 (2.2%) |
| Rituximab, ibrutinib, bortezomib | 12 (27%) |
| OFA-FC | 1 (2.2%) |
| IgM patients (n) . | 163 . |
|---|---|
| IgM MGUS | 53 |
| aWM | 54 |
| Newly diagnosed sWM | 41 |
| WM in relapse | 3 |
| WM during therapy and in remission | 1 |
| WM during therapy and in stable disease | 2 |
| WM posttherapy and in remission | 8 |
| WM posttherapy and in stable disease | 1 |
| Kappa/lambda | 116/47 |
| Age, median (range), y | 69 (34-92) |
| BM infiltration, median (range), % | 20 (0-95) |
| IgM levels, median (range), mg/dL | 1050 (18-10 800) |
| Treatment | 44 |
| DRC | 30 (69%) |
| FCR | 1 (2.2%) |
| Rituximab, ibrutinib, bortezomib | 12 (27%) |
| OFA-FC | 1 (2.2%) |
DRC, dexamethasone-rituximab-cyclophosphamide; FCR, fludarabine-cyclophosphamide-rituximab; OFA-FC, cyclophosphamide-fludarabine-ofatumumab.
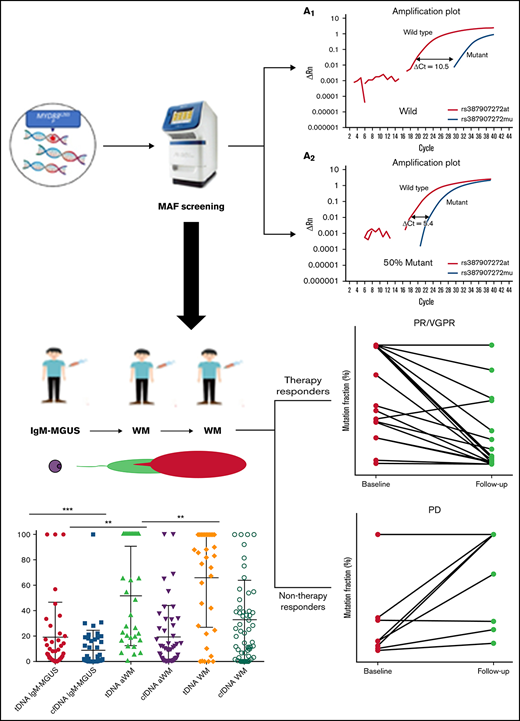
Allele specificity and sensitivity of Cast-PCR
In the Cast-PCR assay, the determination of the mutation allele status for each sample was based on the quantification of the ΔCt cutoff value. For this, the MYD88L265P mutant allele assay and the corresponding gene reference assay (MYD88WD) were initially run on 21 negative samples (cell lines, cfDNA and tDNA samples) and 20 positive samples (WM cell lines, cfDNA and tDNA), each of which was analyzed in 3 replicates. Positive control samples included the two WM cell lines, MWCL1 and BCWM1, and WM patients who had been previously screened and determined as positive for the MYD88L265P mutation.5,11,18,19 All positive controls including WM cell lines were heterozygous to the MYD88L265P mutation. ΔCt values were calculated for each sample run with a mutant allele assay/gene reference assay pair. The average ΔCt value for all samples was then calculated by using the mutation detector software and used to derive the detection ΔCt cutoff value for the mutant allele assay. From the analysis of all negative controls, a sample was defined as MYD88WD (100% wild) when the ΔCt value of MYD88L265P vs MYD88WD difference was >9.03; this means that the MYD88L265P probe was amplified 9.03 cycles after the MYD88WD probe (Figure 1A1). All tDNAs from the BM of the 10 patients with multiple myeloma used as negative controls as well as the tDNA samples from the BM of 1 patient with marginal zone lymphoma and of 1 patient with mantle cell lymphoma, were MYD88WT (ΔCt cutoff value >9.03). In positive controls, a sample was defined as 100% MYD88L265P when the ΔCt value of MYD88L265P vs MYD88WD ratio was equal to 0, meaning that at least 50% of the alleles were MYD88L265P because all positive controls, including WM cell lines, were heterozygous for the mutation.
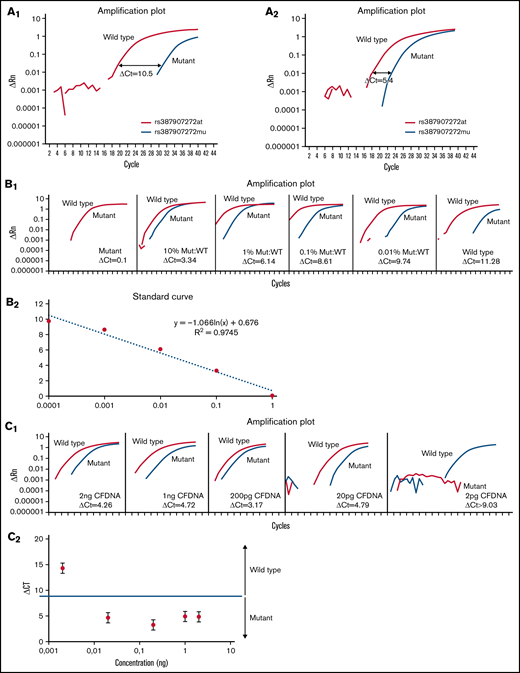
Evaluation of Cast-PCR assay. (A1) Representative amplification Cast-PCR plots for wild type cfDNA samples. (A2) Representative amplification Cast-PCR plots for MYD88L265P cfDNA samples. (B1) Evaluation of Cast-PCR sensitivity by the determination of the LOD using dilutions at different ratios of MYD88L265P MWCL1 cell line and MYD88WT gDNA clinical sample. (B2) Representation of the standard curve between ΔCt and dilution factor of MYD88L265P and MYD88WT samples. (C1) Determination of Cast-PCR efficiency by using 0.5 to 1000 times serial dilutions of mutated cfDNA sample. (C2) Determination of Cast-PCR LOD based on the quantity of DNA in the reaction.
Evaluation of Cast-PCR assay. (A1) Representative amplification Cast-PCR plots for wild type cfDNA samples. (A2) Representative amplification Cast-PCR plots for MYD88L265P cfDNA samples. (B1) Evaluation of Cast-PCR sensitivity by the determination of the LOD using dilutions at different ratios of MYD88L265P MWCL1 cell line and MYD88WT gDNA clinical sample. (B2) Representation of the standard curve between ΔCt and dilution factor of MYD88L265P and MYD88WT samples. (C1) Determination of Cast-PCR efficiency by using 0.5 to 1000 times serial dilutions of mutated cfDNA sample. (C2) Determination of Cast-PCR LOD based on the quantity of DNA in the reaction.
To evaluate the sensitivity of the Cast-PCR assay in conditions that correspond to a mixed tumor and normal cellular composition, we performed serial dilutions of the WM cell line MWCL1 (heterozygous for MYD88L265P equal copies of wild and mutant alleles) in genomic DNA (gDNA) of a clinical sample containing only the MYD88WT genotype (wild-type DNA). The ratio of mutated to wild-type DNA was 10%, 1%, 0.1%, and 0.01%, which corresponded to 4000, 400, 40, and 4 mutated copies in 40 000 copies in 100 ng gDNA. The copies of each DNA sample were determined by using the ddPCR assay. The limit of detection (LOD) was determined by using the ΔCt cutoff value as described earlier or considered as absent for either mutant or the wild-type alleles when the cycle threshold value was >38. The LOD for the Cast-PCR assay was at the 0.1% level, corresponding to 40 copies of the diluted mutant content in 40 000 wild-type copies (Figure 1B1-1B2).
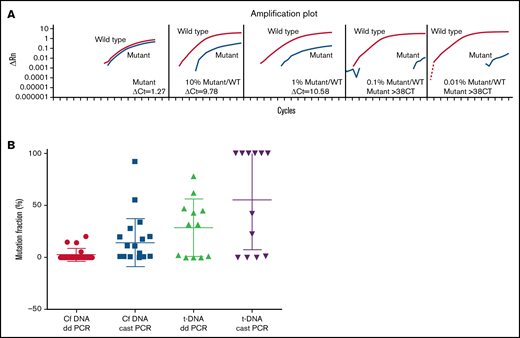
Evaluation of Cast-PCR compared with other assays. (A) Determination of the LOD in AS-PCR using different ratios of the MYD88L265P MWCL1 cell line and the MYD88WT gDNA clinical sample. (B) Comparison of Cast-PCR and ddPCR in tDNA and cfDNA samples. Cast-PCR can detect mutant copies at very low concentrations of cfDNA.
Evaluation of Cast-PCR compared with other assays. (A) Determination of the LOD in AS-PCR using different ratios of the MYD88L265P MWCL1 cell line and the MYD88WT gDNA clinical sample. (B) Comparison of Cast-PCR and ddPCR in tDNA and cfDNA samples. Cast-PCR can detect mutant copies at very low concentrations of cfDNA.
In addition, to determine the efficiency of the Cast-PCR assay in working at a low DNA concentration, we used 2 ng of the cfDNA from a patient harboring the MYD88L265P mutation, which was then serially diluted to 10%, 1%, and 0.1%. As shown in Figure 1C, the assay performed with very low quantities of DNA (as low as 20 pg per reaction), indicating the suitability of this primer set and the accuracy and sensitivity of the reaction. In addition, the reproducibility of the assay was satisfactory because the standard deviation was 1.15% for the MYD88WD control and 1.05% for MYD88L265P.
Cast-PCR vs AS-PCR
We and others have previously described the detection of the MYD88L265P mutation by AS-PCR and direct sequencing in both tDNA and cfDNA. We next compared the LOD of the Cast-PCR assay vs the standard AS-PCR used for the detection of the MYD88L265P mutation. As noted earlier, the levels of mutated DNA in the wild-type DNA corresponded to 10%, 1%, 0.1%, and 0.01% mutated to wild-type DNA ratios. AS-PCR could only detect the mutant allele at the 1% level; that is, 400 copies of diluted mutant content in 40 000 wild-type copies (Figure 2A), corresponding to 10 times lower LOD compared with Cast-PCR. In addition, to perform the standard AS-PCR, a substantially higher amount of DNA (1 ng per reaction) was required compared with the Cast-PCR assay (0.02 ng).
We then evaluated 20 samples (10 with tDNA and 10 with cfDNA) from patients with MYD88L265P IgM monoclonal gammopathies by both assays (Cast-PCR and AS-PCR) as well as 5 control MYD88WT samples. All 10 tDNA samples tested were flagged as positive by both assays. However, in cfDNA samples, 8 of 10 also tested positive in both assays, but 2 of 10 samples were found positive only by the Cast-PCR but not by AS-PCR. This was probably due to the fact that the amount of cfDNA in the particular samples was insufficient to identify the mutant allele. Sensitivity and specificity values of Cast-PCR compared with AS-PCR in cfDNA were also calculated. These values were based on the consensus result of each available assay on tDNA, which was used as the ground truth to evaluate the performance of these assays on cfDNA, which is the main focus of the current study. The sensitivity and specificity of Cast-PCR assay in cfDNA were 90.8% and 87.5%, respectively, compared with 28.57% and 100% of the AS-PCR assay (supplemental Table 1). Fisher’s exact test comparing Cast-PCR vs AS-PCR using patient samples and control samples (cfDNA and tDNA) that were performed with both assays showed a significant difference between Cast-PCR and AS-PCR (P = .028).
Cast-PCR vs ddPCR for the detection of MYD88L265P
To further evaluate Cast-PCR, a cohort of cfDNA and tDNA samples was also screened with ddPCR. As with qPCR, ddPCR technology uses Taq polymerase in a standard PCR reaction to amplify a target DNA fragment from a complex sample using prevalidated primer or primer/probe assays. However, in contrast to standard qPCR assays, it offers the advantage of direct and independent quantification of DNA without standard curves, giving more precise and reproducible data. As discussed earlier, we compared the LOD of the Cast-PCR assay vs that of the ddPCR assay used for the detection of the MYD88L265P mutation. The LOD for the ddPCR assay was at the 0.05% level, corresponding to 20 copies of the diluted mutant content in 40 000 wild-type copies; that is, 2 times higher LOD compared with Cast-PCR. Overall, 15 tDNA samples and 25 cfDNA samples from 40 patients, as well as 4 control samples (2 positive and 2 negative controls), were tested by using both Cast-PCR and ddPCR. Of the 15 tDNA samples tested by using both methods, 14 (93%) were positive and 1 (7%) was negative for the presence of MYD88L265P by both Cast-PCR and ddPCR; there were no discordances between the 2 assays. However, some discordances were observed among the 25 cfDNA samples. Specifically, 10 (60%) of 28 cfDNA samples were negative for MYD88L265P per the ddPCR assay, whereas 5 (17%) of 28 were negative for MYD88L265P per the Cast-PCR assay. Overall, the discordances in cfDNA between the 2 assays were 10 (40%) of 25 (Figure 2B). The correlation coefficient between the assays for MAF was high in tDNA (r2 = 0.7391) but low in cfDNA (r2 = 0.4288).20 This is probably because the amount of tDNA is much higher compared with cfDNA, and ddPCR requires higher amounts of DNA.12,21 Sensitivity and specificity values of ddPCR in cfDNA were also calculated as noted earlier (28.57% and 100%, respectively) (supplemental Table 1). Fisher’s exact test comparing Cast-PCR vs ddPCR using patient samples and control samples (cfDNA and tDNA) that were performed with both assays showed no significant difference between Cast-PCR and ddPCR (P = .16). Furthermore, the correlation coefficient between BM infiltration and MAF with ddPCR was r2 = 0.3, whereas the correlation coefficient between BM infiltration and MAF with Cast-PCR was r2 = 0.46. Positive controls scored as positive for MYD88L265P and negative controls scored as negative for MYD88L265P according to both methods.
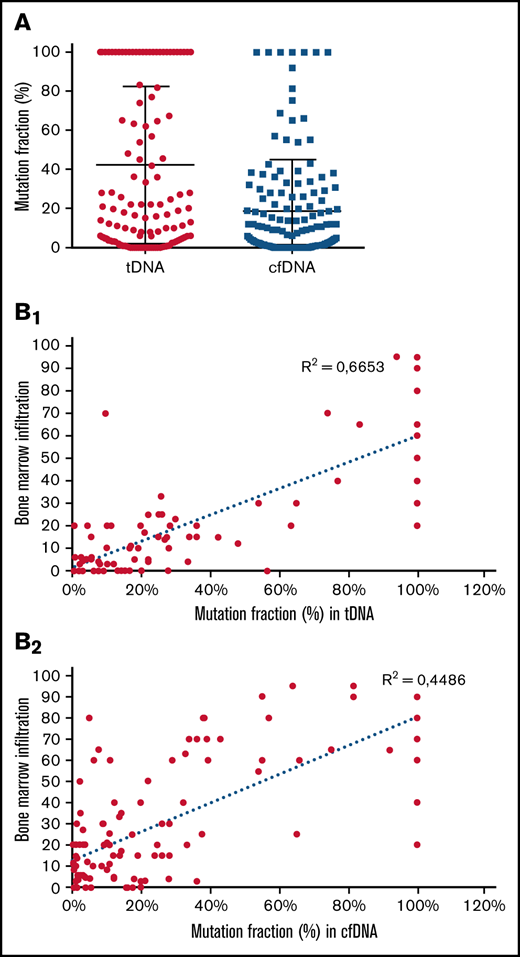
MYD88L265P MAF screening in patients with IgM monoclonal gammopathies
Using the Cast-PCR assay, we evaluated a total of 249 samples from 163 patients. Samples included 105 tDNA samples from BM aspirates and 144 cfDNA samples from PB specimens, of which 86 were paired BM and PB samples. MYD88L265P mutation was detected in 221 (89%) of 249 patients. Among the 86 paired BM and PB samples, the rate of MYD88L265P mutation detection was 92% in tDNA and 86% in cfDNA according to Cast-PCR (Table 2). Furthermore, the MYD88L265P vs MYD88WD ratio (MAF) was determined in the tDNA and cfDNA samples of all 163 patients with IgM monoclonal gammopathies (Figure 3A). In addition, a correlation analysis was performed between BM infiltration of all patients and MAF in tDNA and cfDNA samples. The analysis showed a positive moderate correlation between BM infiltration and MAF in tDNA samples (r2 = 0.6653; P < .001) (Figure 3B1) and a weaker positive correlation between BM infiltration and mutation fraction in cfDNA samples (r2 = 0.4486; P = not significant) (Figure 3B2). Regarding discordances of the mutation status between tDNA and cfDNA, 7 patients exhibited an MYD88WT phenotype in cfDNA but not in tDNA (BMI range, 0%-30%; IgM range, 292-1810; MAF range in tDNA, 16%-100%). Conversely, 3 patients exhibited an MYD88L265P phenotype in cfDNA but not in tDNA (BMI range, 0%-20%; MAF range in cfDNA, 3.7%-30%). Performance statistics for comparison between tDNA and cfDNA using Cast-PCR are displayed in supplemental Table 2. Sensitivity and specificity of Cast-PCR in tDNA were 97.39% (95% CI, 92.57- 99.46) and 92.31% (95% CI, 63.97-99.81), respectively. Sensitivity and specificity of Cast-PCR in cfDNA were 90.8% (95% CI, 82.68- 95.95) and 87.5% (95% CI, 67.64- 97.34). In addition, true-positive, true-negative, false-positive, and false-negative values in tDNA were 112, 12, 1, and 3, and in cfDNA, 79, 21, 3, and 8.
MYD88L265P presence among patients with IgM monoclonal gammopathies
| Mutation rate (%) . | IgM-MGUS (n = 53) . | aWM (n = 54) . | sWM (n = 56) . |
|---|---|---|---|
| tDNA | 89% (33/37) | 97% (32/33) | 92% (36/39) |
| cfDNA | 80% (41/51) | 82% (37/45) | 93% (44/47) |
| Mutation rate (%) . | IgM-MGUS (n = 53) . | aWM (n = 54) . | sWM (n = 56) . |
|---|---|---|---|
| tDNA | 89% (33/37) | 97% (32/33) | 92% (36/39) |
| cfDNA | 80% (41/51) | 82% (37/45) | 93% (44/47) |
MYD88L265P MAF analysis in 163 patients with IgM monoclonal gammopathies. (A) MAF analysis of 105 tDNA samples and 144 cfDNA samples shows that the MYD88L265P mutation fraction is higher in tDNA compared with cfDNA (P < .01). (B1) Correlation analysis between BM infiltration of all patients and MAF in tDNA samples showed a moderate positive correlation. (B2) Correlation analysis between BM infiltration of all patients and MAF in cfDNA samples showed a low positive correlation.
MYD88L265P MAF analysis in 163 patients with IgM monoclonal gammopathies. (A) MAF analysis of 105 tDNA samples and 144 cfDNA samples shows that the MYD88L265P mutation fraction is higher in tDNA compared with cfDNA (P < .01). (B1) Correlation analysis between BM infiltration of all patients and MAF in tDNA samples showed a moderate positive correlation. (B2) Correlation analysis between BM infiltration of all patients and MAF in cfDNA samples showed a low positive correlation.
In the subgroup of patients with IgM-MGUS and with available tDNA, 33 of 37 were MYD88L265P and had a median MAF of 7.74%; in 41 of 51 patients with IgM-MGUS and available cfDNA, the median MAF was 1.6%. Among patients with aWM, 32 of 33 with available tDNA harbored MYD88L265P, and the median MAF was 42%; in the 37 of 45 patients with available cfDNA and MYD88L265P, the median MAF was 10%. Finally, in sWM patients with MYD88L265P, 36 of 39 with available tDNA samples had a median MAF of 84.5%; in the 44 of 47 patients with available cfDNA, the median MAF was 26% (Figure 4). Thus, MAF is higher among patients with more advanced disease and higher tumor burden (analysis of variance, P < .001).
MAF among patients with IgM monoclonal gammopathy. The mutation detector analysis software revealed the following: IgM-MGUS patients had a median MYD88L265P MAF of 7.74% and 1.6% for tDNA and cfDNA, respectively; aWM patients had a median MAF of 42% and 10% for tDNA and cfDNA; and sWM patients had a median MAF of 84.5% and 26% for tDNA and cfDNA.
MAF among patients with IgM monoclonal gammopathy. The mutation detector analysis software revealed the following: IgM-MGUS patients had a median MYD88L265P MAF of 7.74% and 1.6% for tDNA and cfDNA, respectively; aWM patients had a median MAF of 42% and 10% for tDNA and cfDNA; and sWM patients had a median MAF of 84.5% and 26% for tDNA and cfDNA.
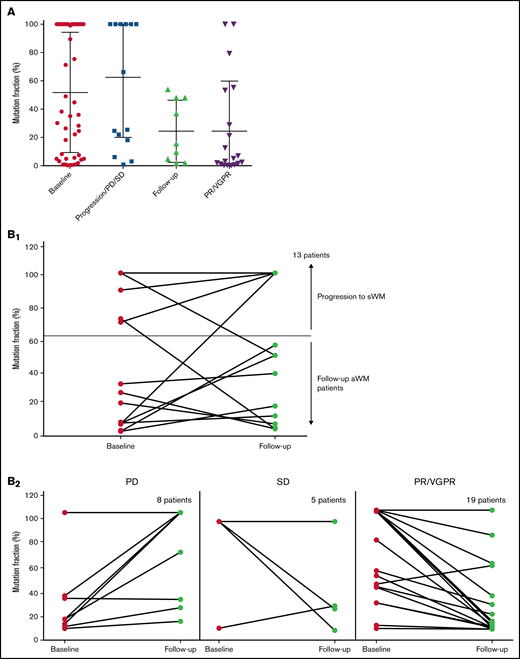
MYD88L265P for MAF screening in follow-up patients with IgM monoclonal gammopathies
To explore the use of MYD88L265 MAF as a potential tool/biomarker for evaluation of the disease course (progression and response to therapy), we also determined the MAF in the cfDNA (and in few cases in tDNA) of sequential patient samples: in 4 patients who progressed from IgM-MGUS or aWM to symptomatic WM, in 7 aWM patients at follow-up, and in 28 sWM patients before and after therapy (Figure 5A). Patients with sWM who received therapy were categorized into 3 subgroups: patients at progressive disease (n = 8), patients at stable disease (n = 5), and patients at partial or very good partial response (PR or VGPR, respectively; n = 19) (supplemental Table 3). Among patients who progressed, median MAF increased from 79% to 99% in pooled cfDNA and tDNA samples, whereas the average MAF of MYD88L265P of aWM patients at follow-up decreased from 18% to 16% in pooled cfDNA and tDNA samples (Figure 5B1). Among sWM patients who received therapy, the median MAF of MYD88L265P of patients with progressive disease increased from 7.75% to 83%, the median MAF of patients with stable disease decreased from 99% to 24.6%, and the median MAF of patients with PR/VGPR decreased from 99% to 4.9% sWM (Figure 5B2).
MAF screening in follow-up patients. (A) Sequential samples from patients at progression, follow-up visits and PR/VGPR. (B1) Patients who have progressed from aWM or IgM-MGUS the median MAF of MYD88L265P was increased while in follow-up aWM patients the median MAF was decreased. (B2) In sWM patients with progressive disease (PD), the median MAF was increased while in sWM patients with stable disease (SD) or PR/VGPR the median MAF was decreased.
MAF screening in follow-up patients. (A) Sequential samples from patients at progression, follow-up visits and PR/VGPR. (B1) Patients who have progressed from aWM or IgM-MGUS the median MAF of MYD88L265P was increased while in follow-up aWM patients the median MAF was decreased. (B2) In sWM patients with progressive disease (PD), the median MAF was increased while in sWM patients with stable disease (SD) or PR/VGPR the median MAF was decreased.
Discussion
Evaluation of cfDNA for mutational characterization and monitoring of disease burden has been recently described in several hematologic malignancies, including IgM monoclonal gammopathies, and showed remarkable results.22-24 Our group was the first to report that cfDNA derived from the plasma of patients with IgM monoclonal gammopathies could mirror the BM mutational burden, with a concordance of almost 95% compared with tDNA from CD19+ selected BM-derived cells13 ; however, we also identified that further improvement in sensitivity was necessary. In the current study, we report a methodologic approach, using Cast-PCR, in detecting MYD88L265P, the most common mutation found in patients with IgM monoclonal gammopathies, which is characterized by high sensitivity and clinical applicability, and may also provide semi-quantitative evaluations of tumor burden. Thus, Cast-PCR fulfills the requirements regarding the efficiency of MYD88L265 mutation analysis in the routine clinical setting by its capability in identifying the mutation cost-effectively with high sensitivity and specificity.
The use of the Cast-PCR assay for the detection of MYD88L265 mutation revealed an overall mutation detection rate of 92% in tDNA samples and 86% in cfDNA samples, in agreement with previously reported studies of the mutation detection ratio in patients with IgM monoclonal gammopathies.11,25-27 We evaluated Cast-PCR through comparisons with standard AS-PCR and with the more sensitive but also more costly ddPCR assay. Evaluating the LOD of Cast-PCR by using serial dilutions of clinical samples with known genotypes, we were able to make determinations with mutant copies as low as 0.1% in a large number of wild-type copies and with amounts of DNA as low as 20 pg per reaction. The LOD of Cast-PCR compared with those of standard AS-PCR and ddPCR was 0.1% vs 1% vs 0.05%, respectively. However, the advantage of this Cast-PCR compared with previously described assays is its ability to detect the mutation at especially low amounts of DNA, which is particularly the issue encountered in downstream applications of cfDNA. Because the wild-type allele present in the cfDNA is much higher compared with that of the tDNA, the Cast-PCR assay specifically works by suppressing the wild-type background by minimizing the amplification of mismatched products derived from the wild-type allele and also minimizing the risk of false-negative results in both tDNA and cfDNA samples with low content of mutated DNA. Hence, in terms of sensitivity, Cast-PCR assay in cfDNA samples seems to be much more sensitive (90.8%) compared with AS-PCR (28.57%) and ddPCR (27.27%). This level of sensitivity can further allow use of this assay for evaluation of residual disease in patients who achieve very deep responses; although this is not often achieved in WM, the introduction of new effective drugs may allow this depth of response.
Another major advantage of the Cast-PCR assay is its ability to provide a semi-quantitative evaluation of tumor burden by determining the MAF of MYD88L265 for each patient with IgM monoclonal gammopathy who harbors the mutation. This feature of the method is particularly interesting and revealed the differences in tumor burden between patients with IgM-MGUS and WM as well as between those with aWM and sWM. Thus, using Cast-PCR to assess MAF, an evaluation of tumor burden is feasible at the molecular level. Importantly, the differences in MAF that reflect tumor burden were also observed in both the cfDNA and the tDNA samples. Based on these findings, a less invasive evaluation of tumor load becomes feasible, using cfDNA from the PB. Further evaluations in larger cohorts are essential, and are in progress, to assess whether these measurements have an impact in further defining the disease status of these patients, especially for monitoring patients after initial diagnosis.
In translating our findings to the clinical setting, we also evaluated MAF of MYD88L265P at sequential time points of patients at different disease stages. Importantly, our results indicate that this method can provide dynamic results that follow the disease evolution. Although we only evaluated a small group of patients, we were able to see an increase of MAF accompanied with disease progression from asymptomatic to symptomatic stages but also an increased MAF in sWM patients with progressive disease. We also noted a decrease of MAF in patients with stable disease after therapy or patients with PR or VGPR, indicating that they responded to therapy. In this study, the time points of the sample collection in the follow-up patients are heterogeneous; however, future screening in a larger cohort of patients will help determine the most optimum time points for follow-up screening. These data provide a proof of concept that molecular methods could be implemented in the evaluation and follow-up of the disease. In addition, further refinement and inclusion of additional molecular targets could provide a tool for the molecular surveillance of tumors, especially during therapy, which could identify the development of resistant clones by targeted mutational analysis.
In conclusion, Cast-PCR provides a new tool that is sensitive and clinically available, which has, in addition to MYD88L265P detection, the potential to monitor tumor burden and disease evolution in patients with IgM monoclonal gammopathies. By using MAF screening in the cfDNA sample of patients, our goal was to use a highly sensitive technique in detecting early progression, especially in cases in which IgM might not be that informative (eg, in patients with nonmeasurable IgM levels per standard criteria). Also, because the correlation of MAF to tumor burden is better than that of IgM, it might be a useful tool for identifying patients who fail therapy or relapse early. However, this is an ongoing study that primarily aims to establish the method and second to provide the initial data for further development and validation. A next step will be a systematic sample collection and evaluation to define optimal time points and cutoffs to clinical outcomes and response to therapy. Following further validation in larger cohorts, this tool could become valuable for the molecular monitoring of WM at different stages of the disease, allowing a more personalized approach to therapy and follow-up.
Authorship
Contribution: T.B. designed the research, performed research, analyzed data, and wrote the paper; A.M. performed research and wrote the paper; D.P. performed research and analyzed data; N.M.-K., C.I.L., and A.D.S. performed research; F.A. performed the statistical analysis; F.T., I.N.-S, and M.G. analyzed data; I.P.T., E.T., and M.A.D. wrote the paper; E.L. designed research and wrote the paper; and E.K. analyzed data and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Tina Bagratuni, Department of Clinical Therapeutics, National and Kapodistrian University of Athens, School of Medicine, 80 Vas. Sofias Ave, 11528 Athens, Greece; e-mail: tbagratuni@med.uoa.gr.
References
Author notes
Requests for data sharing may be submitted to the corresponding author (Tina Bagratuni; e-mail: tbagratuni@med.uoa.gr).
The online version of this article contains a data supplement.