Key Points
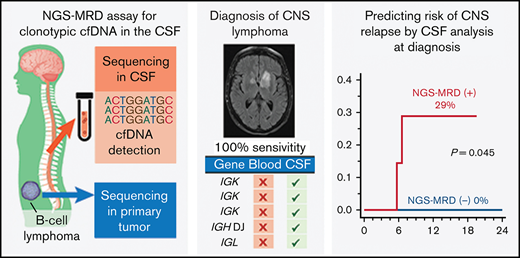
The NGS-MRD assay detected clonotypic DNA in 100% of CSF samples from patients who had lymphoma with parenchymal CNS involvement.
Clonotypic DNA in CSF was present in 36% of newly diagnosed aggressive lymphomas and was associated with a 29% risk of CNS recurrence.
Abstract
The diagnosis of parenchymal central nervous system (CNS) invasion and prediction of risk for future CNS recurrence are major challenges in the management of aggressive lymphomas, and accurate biomarkers are needed to supplement clinical risk predictors. For this purpose, we studied the results of a next-generation sequencing (NGS)–based assay that detects tumor-derived DNA for clonotypic immunoglobulin gene rearrangements in the cerebrospinal fluid (CSF) of patients with lymphomas. Used as a diagnostic tool, the NGS-minimal residual disease (NGS-MRD) assay detected clonotypic DNA in 100% of CSF samples from 13 patients with known CNS involvement. They included 7 patients with parenchymal brain disease only, whose CSF tested negative by standard cytology and flow cytometry, and 6 historical DNA aliquots collected from patients at a median of 39 months before accession, which had failed to show clonal rearrangements using standard polymerase chain reaction. For risk prognostication, we prospectively collected CSF from 22 patients with newly diagnosed B-cell lymphomas at high clinical risk of CNS recurrence, of whom 8 (36%) had detectable clonotypic DNA in the CSF. Despite intrathecal prophylaxis, a positive assay of CSF was associated with a 29% cumulative risk of CNS recurrence within 12 months of diagnosis, in contrast with a 0% risk among patients with negative CSF (P = .045). These observations suggest that detection of clonotypic DNA can aid in the diagnosis of suspected parenchymal brain recurrence in aggressive lymphoma. Furthermore, the NGS-MRD assay may enhance clinical risk assessment for CNS recurrence among patients with newly diagnosed lymphomas and help select those who may benefit most from novel approaches to CNS-directed prophylaxis.
Introduction
Central nervous system (CNS) recurrence remains a major clinical challenge in aggressive lymphoma. It occurs in 2% to 6% of patients with diffuse large B-cell (DLBCL) and high-grade B-cell (HGBCL) or Burkitt lymphoma (BL) and in up to 30% of patients in certain high-risk subcategories.1-4 Because survival after a CNS recurrence is very poor (median, 2-4 months), patients who are at high risk typically receive intensive and potentially toxic intrathecal or systemic CNS-directed therapy.5-7 Unfortunately, clinical prognostic scores (eg, the CNS-International Prognostic Index [IPI]) have limited sensitivity, as nearly half of CNS recurrences occur in groups scored as low or intermediate risk.8,9 Standard evaluations of the cerebrospinal fluid (CSF) with cytology, flow cytometry, or polymerase chain reaction (PCR) for the presence of clonal IGH rearrangements, when positive, are considered indicators of overt CNS involvement.10-12 Similarly, diagnosis of CNS recurrence with parenchymal brain disease often requires invasive neurosurgical biopsy; CSF evaluations have low sensitivity in this setting.13 Therefore, there is an ongoing need for more accurate biomarkers that can predict high risk of future CNS recurrence at the time of diagnosis of lymphoma or that can aid in diagnosis of radiographically or clinically suspected parenchymal recurrence.14
Measurement of lymphoma-specific cell-free DNA (cfDNA) has recently emerged as a potential tool for identifying minimal amounts of lymphoma through analysis of body fluids.15,16 cfDNA can be detected in the plasma of patients with DLBCL, providing a sensitive means of detecting minimal residual disease (MRD) after treatment or of predicting impending systemic recurrence.17-23 Unlike in mantle cell or follicular lymphomas, which may produce highly specific BCL1-IGH or BCL2-IGH transcripts trackable by quantitative PCR, there is no single universal sequence suitable for detecting DLBCL. The 2 currently used cfDNA strategies involve detecting specific somatic mutations in genes frequently altered in DLBCL or detecting lymphoma-specific clonotypic DNA rearrangements within the IGH, IGK, and IGL loci of the B-cell receptor. Prior studies have tested the first strategy by using next-generation sequencing (NGS) combined with digital PCR to detect lymphoma-derived single-nucleotide variants (mainly MYD88L265P) in the CSF of patients with known CNS lymphoma.24,25 We hypothesized that a high-sensitivity, clonotype-based NGS-MRD assay in the CSF may provide more streamlined and universally applicable functionality, both as a diagnostic tool for patients with suspected CNS invasion and as a prognostic biomarker for the risk of future CNS recurrence among patients with newly diagnosed systemic lymphoma.
Methods
Patients and samples
This study was approved by the Institutional Review Board at Rhode Island Hospital and included 37 patients from 3 groups (Figure 1A; supplemental Table 1) An additional 3 patients for whom no trackable clonotypic rearrangements could be obtained were excluded from the analysis. The first group included patients (n = 7) with known primary or secondary involvement of the CNS by an aggressive lymphoma, from whom CSF was collected prospectively at the time of diagnostic lumbar puncture. The second group included patients with CNS involvement (determined clinically or radiographically), who had historical stored samples of DNA (n = 8; although in 2, the amount of DNA proved insufficient for analysis) extracted from CSF collected at the time of the diagnostic procedure concurrent with known CNS involvement; these samples had tested negative or nondiagnostic in a PCR-based assay designed to detect IGH rearrangement.26 The third group (n = 22) were prospective observational patients with newly diagnosed aggressive lymphomas (including DLBCL, HGBCL/double-hit lymphoma, BL, and plasmablastic lymphoma), who had no known CNS involvement, but were deemed high risk for CNS relapse because of histology, anatomical location, or CNS-International Prognostic Index (CNS-IPI). All patients in this cohort underwent a lumbar puncture before administration of any intrathecal therapy or high-dose methotrexate, with CSF deemed negative for lymphoma by cytology, flow cytometry, and/or IGH PCR. Radiographic CNS staging was performed if indicated, at the clinician’s discretion, as was any CNS-directed therapy. Patients donating prospectively collected samples provided informed consent, and the NGS-MRD assay results were not used for any clinical decisions or management.
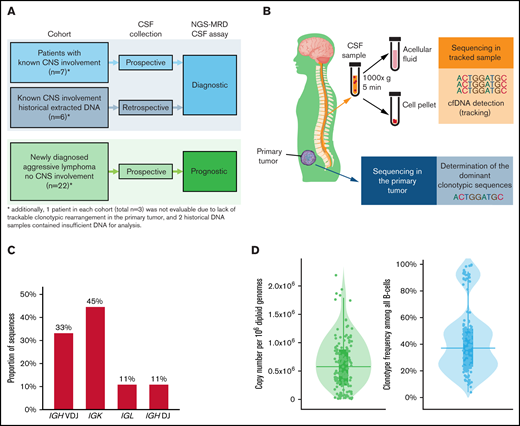
Analysis of clonotypic DNA in primary tumors from aggressive B-cell lymphomas. (A) Subject selection for analysis; the study included 3 groups: 2 groups of patients with known CNS involvement, using prospectively collected CSF (n = 7) and retrospectively obtained, previously extracted CSF DNA (n = 8), in which the NGS-MRD assay was used as a diagnostic modality, and a prospective cohort (n = 22) of patients with newly diagnosed, aggressive lymphoma and no CNS involvement, in whom the NGS-MRD assay was used as a prognostic biomarker. (B) The NGS-MRD assay includes NGS of the primary lymphoma tumor to determine the dominant clonotypic sequence, which can be subsequently “tracked” in plasma or CSF samples containing tumor-derived clonotypic DNA. (C) Distribution of clonotypic sequences (n = 139) from different loci detected by the NGS-MRD assay in all primary tumors (n = 37) in this study (see supplemental Table 1 for a complete list of sequences). (D) Violin plots showing the distribution of copy numbers (per 106 diploid genomes) and frequencies (among all B cells) of clonotypic sequences from the primary lymphoma tumor samples (n = 37). Horizontal line shows the median; box shows interquartile range. IQR, interquartile ranges.
Analysis of clonotypic DNA in primary tumors from aggressive B-cell lymphomas. (A) Subject selection for analysis; the study included 3 groups: 2 groups of patients with known CNS involvement, using prospectively collected CSF (n = 7) and retrospectively obtained, previously extracted CSF DNA (n = 8), in which the NGS-MRD assay was used as a diagnostic modality, and a prospective cohort (n = 22) of patients with newly diagnosed, aggressive lymphoma and no CNS involvement, in whom the NGS-MRD assay was used as a prognostic biomarker. (B) The NGS-MRD assay includes NGS of the primary lymphoma tumor to determine the dominant clonotypic sequence, which can be subsequently “tracked” in plasma or CSF samples containing tumor-derived clonotypic DNA. (C) Distribution of clonotypic sequences (n = 139) from different loci detected by the NGS-MRD assay in all primary tumors (n = 37) in this study (see supplemental Table 1 for a complete list of sequences). (D) Violin plots showing the distribution of copy numbers (per 106 diploid genomes) and frequencies (among all B cells) of clonotypic sequences from the primary lymphoma tumor samples (n = 37). Horizontal line shows the median; box shows interquartile range. IQR, interquartile ranges.
Evaluation of the clonotypic DNA
Both cell-free and genomic DNA were evaluated by quantitative NGS-MRD assay to identify the clonotypic, tumor-specific DNA rearrangements (clonoSEQ; Adaptive Biotechnologies, Seattle, WA; Figure 1B), as previously described.27-29 In brief, genomic DNA was extracted from formalin-fixed, paraffin-embedded (FFPE) samples of primary lymphoma tumors (blood samples in case of leukemic involvement) and then amplified by using locus-specific multiplex PCR with a mix of primers targeting the V, D, and J segments of the IGH (distinguishing IGH VDJ and DJ rearrangement sequences), IGK (including the κ-deleting element), IGL loci, as well as housekeeping genes, with added reaction-specific barcodes.27 In addition, select genomic regions were amplified to determine the total number of diploid genomes in the sample as a denominator for quantification. The amplicons were subsequently submitted to NGS with positive and negative controls for amplification and sequencing steps. CSF and plasma samples underwent genomic DNA extraction, followed by the same locus-specific amplification and NGS as for the FFPE samples. Plasma was collected from standard EDTA-coated blood tubes, frozen within 24 hours, and thawed only once, for sequencing. Five milliliters of CSF was collected during routine clinical lumbar punctures and separated by immediate centrifugation at 1000g at 4°C for 5 minutes into a spun-down cell pellet (resuspended in 0.5 mL of the CSF) and acellular fluid fraction.30 A separate aliquot of the same sample was always submitted for clinical testing, including white blood cell (WBC) and red blood cell (RBC) counts, cytology, flow cytometry, and/or standard IGH PCR. All samples were stored in −80°C until analysis and shipped frozen to the laboratory.
NGS data were analyzed by using a previously described custom pipeline with quality checks at the levels of the flowcell, PCR well, and sample.29 Aligned reads were used to determine specific immunoglobulin gene rearrangements and unique sequences resulting from additional somatic hypermutation representing specific B-cell clones. For subsequent tracking in CSF or plasma samples, “dominant” clonotypic rearrangements that met the following criteria were selected: (1) the rearrangement comprised ≥3% of all locus-specific sequences (for IGH, all IGH VDJ, and DJ rearrangements; for IGK or IGL, all light-chain rearrangements); (2) it comprised ≥0.2% of the total nucleated cells in the sample; (3) it was carried by ≥40 estimated genome equivalents in the analyzed sample; and (4) it was discontinuously distributed (defined as ≤5 sequences in the next decade of sequences when ranked by frequency).27,29 The process accounted for imperfect clonotype matching due to subclonal somatic mutations. The abundance of tumor-specific clonotypic DNA in the CSF or plasma was expressed as the number of cfDNA copies per milliliter of acellular fluid per 106 diploid genomes, for the cell pellet fraction, and as a relative frequency of the malignant clonotype in the background of all B-cell clonotypes present in the sample.
Statistical analysis
Patients’ clinical characteristics were tabulated; all values of continuous variables (including DNA concentrations) were summarized as medians and ranges or interquartile ranges (IQR). Concentrations and frequencies of the clonotypic DNA, correlation between DNA abundance and WBC or RBC in the CSF samples, or between CSF and paired plasma samples were compared between groups using the Somers’ D rank statistic. Jackknife standard errors were adjusted to account for within-patient clustering in all analyses that included multiple DNA sequences from each patient or from paired CSF/plasma samples.31 The cumulative risk of CNS recurrence in the prospective cohort was plotted using Kaplan-Meier analysis and compared using the log-rank test, as there were no competing events recorded. We censored patients’ follow-up in cases with allogeneic stem cell transplantation or chimeric antigen receptor T-cell infusion. All analyses were conducted using MP16.1 (Stata, College Station, TX).
Results
Clonotype identification in primary lymphoma tumors
Among the 40 cases of aggressive lymphoma initially included in the study, 3 (1 decalcified bone marrow biopsy, 1 fine-needle aspiration from a parotid gland, and 1 lymph node biopsy with necrotic tumor) were excluded because they did not yield trackable clonotypic rearrangements, for an overall success rate of 93% (37 of 40). Among the 37 primary tumors included, we detected 139 distinct dominant clonotype sequences, a median of 3 in each tumor (range, 1-9), at a median copy count of 0.58 × 106 per 106 diploid genomes (range, 3.0 × 103 to 2.1 × 106 per 106) and at a median frequency of 37.1% among all B-cells (range, 4.0% to 98.4%; supplemental Table 2; Figure 1C-D).
CSF NGS-MRD assay for diagnosis of CNS lymphoma
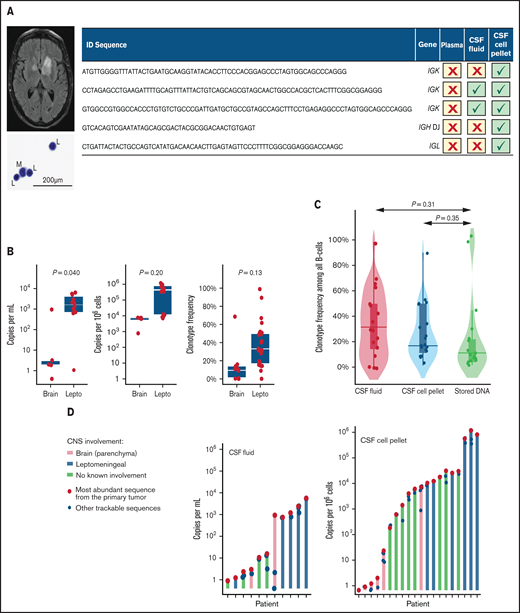
We performed the NGS-MRD assay on the CSF of patients with known CNS lymphoma from 2 cohorts: prospectively collected samples (n = 7) and historical DNA samples previously extracted from CSF (n = 8). The clinical characteristics of these patients are listed in supplemental Table 3; 4 patients had primary CNS lymphoma, and 11 had CNS recurrences of aggressive B-cell lymphomas, of whom 5 had concurrent systemic disease at the time of CSF acquisition. The assay detected clonotypic DNA in the CSF of all 7 prospectively enrolled patients with overt CNS lymphoma (supplemental Table 4). These included 2 patients who had lymphomas that involved only brain parenchyma, with negative CSF evaluations by cytology, flow cytometry, and/or standard IGH PCR (Figure 2A shows an example). The abundance of clonotypic DNA was higher in cases with leptomeningeal (vs parenchymal-only) disease detectable by routine cytology (Figure 2B). Median cfDNA copy count per milliliter of acellular CSF was 2.0 (range, 0.4-929) for parenchymal-only disease and 1649 (range, 1-5620) for leptomeningeal disease (P = .040). Median copy counts per 106 diploid genomes in the cell pellet was 6770 (range, 878-7647) and 450 526 (range, 8105-1 181 171), respectively (P = .20). Median clonotype frequency was 9.4% (range, 0.03% to 68.9%) for parenchymal-only and 33.1% (1.7% to 98.5%) for leptomeningeal lymphoma (P = .13).
CSF NGS-MRD assay for diagnosis of CNS involvement in lymphoma. (A) Case study of a primary CNS lymphoma, showing a magnetic resonance imaging gadolinium-enhanced T2 turbo spin echo sequence with intraparenchymal tumors; a standard CSF cytospin stained with Papanicolaou stain showing scant lymphocytes (L) and monocytes (M) (original magnification, ×600; cell count was 0 per cubic millimeter, and flow cytometry showed an insufficient number of events for evaluation); and clonotypic DNA sequences examined in the primary tumor, plasma (where no sequences were detectable), CSF acellular fluid, and CSF cell pellet fraction. (B) Clonotypic DNA sequences in the CSF of patients with parenchymal brain (n = 2) and leptomeningeal (Lepto, n = 5) lymphoma, measured as copy number per milliliter of acellular fluid, per 106 diploid genomes in the cell pellet fraction, and as the clonotype frequency (in both types of samples). Bars show medians and interquartile ranges; P-values are from Somers’ D statistic adjusted for intrapatient clustering. Note the logarithmic scale on the left and middle panels. (C) distribution of clonotype frequency in CSF fractions obtained from patients with known CNS lymphoma: acellular fluid, cell pellet, and stored historical DNA. (D) relative abundance of various clonotypic sequences in the CSF of each patient (data from all patients included in the study who had a positive NGS-MRD assay in the CSF). The bars and red circles indicate the amount of the most abundant sequence from the primary tumor (expressed as copy count per milliliter of CSF acellular fluid or per 106 diploid genomes in the CSF cell pellet); the blue circles indicate other clonotypic sequences in the sample.
CSF NGS-MRD assay for diagnosis of CNS involvement in lymphoma. (A) Case study of a primary CNS lymphoma, showing a magnetic resonance imaging gadolinium-enhanced T2 turbo spin echo sequence with intraparenchymal tumors; a standard CSF cytospin stained with Papanicolaou stain showing scant lymphocytes (L) and monocytes (M) (original magnification, ×600; cell count was 0 per cubic millimeter, and flow cytometry showed an insufficient number of events for evaluation); and clonotypic DNA sequences examined in the primary tumor, plasma (where no sequences were detectable), CSF acellular fluid, and CSF cell pellet fraction. (B) Clonotypic DNA sequences in the CSF of patients with parenchymal brain (n = 2) and leptomeningeal (Lepto, n = 5) lymphoma, measured as copy number per milliliter of acellular fluid, per 106 diploid genomes in the cell pellet fraction, and as the clonotype frequency (in both types of samples). Bars show medians and interquartile ranges; P-values are from Somers’ D statistic adjusted for intrapatient clustering. Note the logarithmic scale on the left and middle panels. (C) distribution of clonotype frequency in CSF fractions obtained from patients with known CNS lymphoma: acellular fluid, cell pellet, and stored historical DNA. (D) relative abundance of various clonotypic sequences in the CSF of each patient (data from all patients included in the study who had a positive NGS-MRD assay in the CSF). The bars and red circles indicate the amount of the most abundant sequence from the primary tumor (expressed as copy count per milliliter of CSF acellular fluid or per 106 diploid genomes in the CSF cell pellet); the blue circles indicate other clonotypic sequences in the sample.
The retrospective group included 8 DNA samples from patients with known CNS lymphoma, extracted from CSF obtained during historical procedures and stored in −80°C (Figure 2C). These samples had been collected at a median of 39 months (range, 23-72) before accession. All samples had tested negative or were insufficient for evaluation by standard PCR for IGH rearrangement. In 2 cases, the amount of stored DNA was below the minimum required for NGS, despite PCR amplification. In the remaining 6 cases (5 with parenchymal brain lymphoma, 1 with leptomeningeal disease), the NGS-MRD assay detected clonotypic DNA. The median clonotypic DNA count in this group was 1.2 per 106 diploid genomes (range, 0.7-25 601), which reflects differences in sample processing, storage, and DNA extraction for these historical aliquots, compared with freshly collected CSF samples. However, median clonotype frequency was 11.1% (range, 1.6% to 99.3%), which was not significantly different from freshly collected CSF samples (Figure 2C).
We also examined the correlation between the relative abundance of various clonotypic sequences in the CSF compared with the primary tumors. In most cases, the amount of clonotypic DNA was similar for all tracked sequences within each CSF sample, and the most abundant sequence from the primary tumor also had the highest copy number in the CSF (Figure 2D).
Prognostic value of a positive CSF NGS-MRD assay
The prospective observational cohort enrolled 22 patients with newly diagnosed aggressive lymphomas who did not have any CNS involvement on clinical, radiographic, and standard CSF assessments during staging procedures (Table 1). The reasons for eligibility included DLBCL with high CNS-IPI (n = 9), epidural mass (n = 3), or high-risk histology (double/triple-hit, BL, or plasmablastic lymphoma). Twenty patients (91%) received CNS prophylaxis after enrollment (2 declined), including 14 (64%) using only intrathecal methotrexate and/or cytarabine, and 6 (27%) using high-dose systemic methotrexate.
Clinical characteristics of patients with newly diagnosed lymphomas in the prospective cohort with no known CNS disease
| Variable . | All . | CSF NGS-MRD assay . | P . | |
|---|---|---|---|---|
| Positive . | Negative . | |||
| Patients, n | 22 | 8 | 14 | |
| Age, y, median (range) | 63 (27-83) | 53 (38-76) | 67 (27-83) | .34 |
| Female, n (%) | 7 (32) | 1 (13) | 6 (43) | .19 |
| Histology, n (%) | .76 | |||
| DLBCL | 10 (45) | 3 (38) | 7 (50) | — |
| HGBCL* | 7 (32) | 4 (50) | 3 (21) | — |
| THRLBCL | 1 (5) | — | 1 (7) | — |
| Plasmablastic lymphoma | 1 (5) | — | 1 (7) | — |
| BL | 3 (14) | 1 (13) | 2 (14) | — |
| CNS-IPI, n (%)† | .99 | |||
| Low | 2 (11) | 1 (14) | 1 (8) | — |
| Intermediate | 8 (42) | 3 (43) | 5 (42) | — |
| High | 9 (47) | 3 (43) | 6 (50) | — |
| LDH, U/mL, median (range) | 401 (144-1619) | 480 (191-1619) | 287 (144-1553) | .27 |
| MRI brain performed, n (%) | 11 (50) | 4 (50) | 7 (50) | .99 |
| First-line chemotherapy, n (%) | .99 | |||
| R-CHOP | 8 (36) | 3 (38) | 5 (36) | — |
| DA-EPOCH-R | 12 (55) | 4 (50) | 8 (57) | — |
| Other‡ | 2 (9) | 1 (13) | 1 (7) | — |
| CNS prophylaxis | .99 | |||
| High-dose methotrexate | 6 (27) | 2 (25) | 4 (29) | — |
| IT only | 14 (64) | 5 (63) | 9 (64) | — |
| None (declined) | 2 (9) | 1 (13) | 1 (7) | — |
| IT injections, n, median (range) | 4 (1-9) | 3.5 (2-9) | 4 (1-6) | .47 |
| CSF cell count per cubic millimeter | ||||
| WBC, median (range) | 1 (0-3) | 1 (0-3) | 0 (0-3) | .38 |
| RBC, median (range) | 14 (0-331) | 31 (0-299) | 8 (0-331) | .38 |
| Variable . | All . | CSF NGS-MRD assay . | P . | |
|---|---|---|---|---|
| Positive . | Negative . | |||
| Patients, n | 22 | 8 | 14 | |
| Age, y, median (range) | 63 (27-83) | 53 (38-76) | 67 (27-83) | .34 |
| Female, n (%) | 7 (32) | 1 (13) | 6 (43) | .19 |
| Histology, n (%) | .76 | |||
| DLBCL | 10 (45) | 3 (38) | 7 (50) | — |
| HGBCL* | 7 (32) | 4 (50) | 3 (21) | — |
| THRLBCL | 1 (5) | — | 1 (7) | — |
| Plasmablastic lymphoma | 1 (5) | — | 1 (7) | — |
| BL | 3 (14) | 1 (13) | 2 (14) | — |
| CNS-IPI, n (%)† | .99 | |||
| Low | 2 (11) | 1 (14) | 1 (8) | — |
| Intermediate | 8 (42) | 3 (43) | 5 (42) | — |
| High | 9 (47) | 3 (43) | 6 (50) | — |
| LDH, U/mL, median (range) | 401 (144-1619) | 480 (191-1619) | 287 (144-1553) | .27 |
| MRI brain performed, n (%) | 11 (50) | 4 (50) | 7 (50) | .99 |
| First-line chemotherapy, n (%) | .99 | |||
| R-CHOP | 8 (36) | 3 (38) | 5 (36) | — |
| DA-EPOCH-R | 12 (55) | 4 (50) | 8 (57) | — |
| Other‡ | 2 (9) | 1 (13) | 1 (7) | — |
| CNS prophylaxis | .99 | |||
| High-dose methotrexate | 6 (27) | 2 (25) | 4 (29) | — |
| IT only | 14 (64) | 5 (63) | 9 (64) | — |
| None (declined) | 2 (9) | 1 (13) | 1 (7) | — |
| IT injections, n, median (range) | 4 (1-9) | 3.5 (2-9) | 4 (1-6) | .47 |
| CSF cell count per cubic millimeter | ||||
| WBC, median (range) | 1 (0-3) | 1 (0-3) | 0 (0-3) | .38 |
| RBC, median (range) | 14 (0-331) | 31 (0-299) | 8 (0-331) | .38 |
DA-EPOCH-R, dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab; IT, intrathecal; LDH, lactate dehydrogenase; MRI, magnetic resonance imaging; R-CHOP, rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; THRLBCL, T-cell/histiocyte-rich large B-cell lymphoma.
With MYC and BCL2 and/or BCL6 rearrangements.
Calculated for DLBCL, HGBCL, THRLBCL, and plasmablastic lymphoma only.
One patient each for rituximab alone and R-CODOX-M/IVAC (rituximab plus cyclophosphamide, doxorubicin, vincristine, methotrexate/ifosfamide, etoposide, and high-dose cytarabine).
In this cohort, 8 of 22 patients (36%) tested positive on the NGS-MRD assay in the CSF: 4 tested positive in both acellular fluid and cell pellet fractions, and 4 only in the pellet fraction (ie, acellular fluid did not contain clonotypic sequences). Of note, in 11 of 14 negative samples, the acellular CSF fraction failed to show any clonotypic DNA (benign or malignant). The detectable median clonotype copy count was 3.2 (range, 0.9-16) per milliliter in the acellular fluid and 4016 (range, 184-31 179) per 106 diploid genomes in the cell pellet fraction. Corresponding median clonotype frequencies were 18.6% (range, 1.4% to 28.5%) and 7.9% (range, 0.2% to 50.4%), respectively (supplemental Table 5). The median number of cells in the cell pellet samples was 1129 (range, 0-12 599) and did not differ by NGS-MRD status (P = .10).
With a median follow-up of 16 months from the CSF collection, 2 patients (9%; 1 with DLBCL with MYC rearrangement and 1 with triple-hit HGBCL) experienced CNS recurrences after first-line therapy. One recurrence was both intraparenchymal and leptomeningeal, and 1 was leptomeningeal only. Both patients had a positive CSF NGS-MRD assay at diagnosis, and both had received intrathecal methotrexate for prophylaxis, but they had received no systemic high-dose CNS-directed therapy). Two patients with a positive CSF NGS-MRD assay who did not have a recurrence received high-dose methotrexate or cytarabine as part of a primary high-intensity regimen, or as CNS prophylaxis. In contrast, no patient with a negative CSF NGS-MRD assay relapsed in the CNS, although 8 had a systemic recurrence of their lymphoma. A positive CSF NGS-MRD was associated with a 28.6% (95% confidence interval [CI], 8.0% to 74.2%) cumulative risk of CNS recurrence at 12 months, compared with 0% for a negative baseline assay (log-rank P = .045; Figure 3A). We then compared the abundance of the clonotypic DNA between CSF samples from patients with or without relapse (using only samples with detectable sequences and adjusting for intrapatient correlation) and did not find a significant difference in the amount of measurable DNA (Figure 3B).
CSF NGS-MRD assay as a prognostic tool for the risk of CNS recurrence in lymphoma. (A) Cumulative incidence of CNS recurrence in the prospective cohort of patients with no known CNS involvement (n = 22), stratified by the result of the CSF NGS-MRD assay at diagnosis; P-value by log-rank test; 2 of 8 NGS-MRD+ and 0 of 14 NGS-MRD− patients with CNS relapse. (B) Amount of clonotypic DNA in the CSF (each dot represents a specific DNA sequence; sequences that were undetectable were excluded), measured as copy number per milliliter of acellular fluid, per 106 diploid genomes in the cell pellet fraction, and as the clonotype frequency (in both types of material), according to subsequent CNS relapse status. The bars show medians and interquartile ranges; note logarithmic scale on the left and middle panels; P-values are by+ nonparametric Somers’ D statistic adjusted for within-patient clustering. (C) Lack of correlation between CSF contamination by blood (as measured by red cell count per mm3 of CSF) and abundance of clonotypic DNA in the same CSF sample, measured by copy number per milliliter (of the CSF acellular fluid), copy number per 106 diploid genomes (in the CSF cell pellet), or as clonotype frequency in both fractions; P-values by nonparametric Somers’ D statistic adjusted for within-patient clustering; a linear fit with 95% CI bands is also shown. (D) Clonotypic DNA sequences in patients’ plasma (n = 10), measured as cfDNA copy count per milliliter of plasma, and as clonotype frequency among all B-cell genomes. (E) Lack of correlation between the abundance of clonotypic DNA in paired plasma and CSF samples (n = 10), as measured by copy count per milliliter and clonotype frequency in the acellular CSF. P-values by nonparametric Somers’ D statistic adjusted for within-patient clustering; a linear fit with 95% CI bands is also shown.
CSF NGS-MRD assay as a prognostic tool for the risk of CNS recurrence in lymphoma. (A) Cumulative incidence of CNS recurrence in the prospective cohort of patients with no known CNS involvement (n = 22), stratified by the result of the CSF NGS-MRD assay at diagnosis; P-value by log-rank test; 2 of 8 NGS-MRD+ and 0 of 14 NGS-MRD− patients with CNS relapse. (B) Amount of clonotypic DNA in the CSF (each dot represents a specific DNA sequence; sequences that were undetectable were excluded), measured as copy number per milliliter of acellular fluid, per 106 diploid genomes in the cell pellet fraction, and as the clonotype frequency (in both types of material), according to subsequent CNS relapse status. The bars show medians and interquartile ranges; note logarithmic scale on the left and middle panels; P-values are by+ nonparametric Somers’ D statistic adjusted for within-patient clustering. (C) Lack of correlation between CSF contamination by blood (as measured by red cell count per mm3 of CSF) and abundance of clonotypic DNA in the same CSF sample, measured by copy number per milliliter (of the CSF acellular fluid), copy number per 106 diploid genomes (in the CSF cell pellet), or as clonotype frequency in both fractions; P-values by nonparametric Somers’ D statistic adjusted for within-patient clustering; a linear fit with 95% CI bands is also shown. (D) Clonotypic DNA sequences in patients’ plasma (n = 10), measured as cfDNA copy count per milliliter of plasma, and as clonotype frequency among all B-cell genomes. (E) Lack of correlation between the abundance of clonotypic DNA in paired plasma and CSF samples (n = 10), as measured by copy count per milliliter and clonotype frequency in the acellular CSF. P-values by nonparametric Somers’ D statistic adjusted for within-patient clustering; a linear fit with 95% CI bands is also shown.
NGS-MRD assay in the CSF and blood
We investigated whether the clonotypic DNA content in the CSF could be correlated with blood cell or plasma cfDNA contamination that may occur during lumbar puncture. For these analyses, we used freshly collected CSF samples from patients in the prospective cohort with active systemic lymphoma (n = 22). The Median WBC count in the CSF was 1 per microliter (range, 0-3), and the median red blood cell RBC count was 14 per microliter (range, 0-331). These values did not significantly differ between groups with positive or negative CSF NGS-MRD assay (P = .38 for WBC and P = .38 for RBC). We also found no correlation between the RBC count and copy count of the clonotypic DNA in the CSF acellular fluid (P = .25), in cell pellets (P = .72), or between the RBC count and clonotype frequency (P = .52; Figure 3C).
cfDNA was detected in 10 of 15 (67%) available paired plasma samples, at a median copy count of 47 per milliliter (range, 2-25226) and a median frequency of 22.7% (range, 0.02% to 96.2%; Figure 3D). We observed no evident correlation between plasma and CSF fluid in the cfDNA copy count (P = 0.33) or clonotype frequency (P = 0.46; Figure 3E).
Discussion
In this study, we examined the NGS-MRD assay as a tool to detect clonotypic tumor DNA in the CSF of patients with lymphoma. We used the assay as a diagnostic method of identifying parenchymal CNS invasion and as a prognostic biomarker in systemic lymphoma. The assay identified tumor-specific clonotypic DNA in 100% of cases with parenchymal brain involvement in both fresh and historical CSF specimens, despite the failure of other CSF evaluation methods. Furthermore, the assay was positive in 36% of newly diagnosed patients without known CNS involvement, and detection of clonotypic DNA in the CSF was associated with CNS recurrence in 29% of the patients. These data lay the groundwork for novel approaches to highly sensitive molecular CSF evaluations, including a more accurate selection of patients for CNS-directed prophylaxis.
In current clinical practice, CSF evaluations rely on direct detection of malignant cells by cytology and/or flow cytometry, with molecular testing (typically, PCR-based clonality assays) reserved for confirmation of uncertain cases. However, most CNS recurrences of DLBCL after initial rituximab-containing immunochemotherapy involve only brain parenchyma, making standard CSF methods largely unsuitable for diagnosis. Among 1693 patients from the German High-Grade Non-Hodgkin Lymphoma Study Group, 37 (2.2%) had a CNS recurrence, of whom 21 (57%) had disease limited to the brain parenchyma with a negative CSF.13 In an international series of 113 patients with isolated parenchymal brain relapse, only 48% obtained any histologic confirmation, and only 16% had a positive CSF.32 Similarly, El-Galaly et al reported histologic confirmation of CNS relapse in 44% of 291 patients in a more recent cohort.5 In the British Columbia Cancer Agency experience, 79% of CNS relapses after a rituximab-based regimen occurred without any systemic involvement, 63% were parenchymal only, and 26% were diagnosed from the CSF (compared with 58%, 25%, and 58%, respectively, before rituximab).33 A brain biopsy is not always feasible and has limited diagnostic yield, especially after administration of corticosteroids. The NGS-MRD assay detected lymphoma-specific clonotypic DNA in 100% of cases of parenchymal CNS disease, offering a potentially highly sensitive method to confirm a suspected CNS relapse. One limitation of this assay is that it requires sequence identification from the primary tumor sample. However, if plasma-based MRD monitoring becomes routine in systemic DLBCL,17-21 the baseline clonotype will be readily available to compare against CSF samples collected at the time of the suspected CNS relapse. In contrast, the NGS-MRD assay is not suitable for diagnosis of primary CNS lymphoma, where the primary tumor is within the brain itself. It can still confirm a relapse that occurs after the initial biopsy and treatment.
For patients with newly diagnosed systemic lymphoma, baseline CSF evaluations by cytology and flow cytometry can reveal overt leptomeningeal involvement,10-12 but selection of patients for CNS prophylaxis relies on clinical risk factors.2,3,6,8,9,34 Performance of PCR-based IGH clonality assays has been inconsistent, and they have not been adopted to guide clinical decisions.35-37 The accuracy of other proposed CSF biomarkers such as soluble CD19 or cytokines including the C-X-C motif chemokine ligand 13 (CXCL13) in the absence of gross disease is uncertain.14,38 Relying on the CNS-IPI for delivery of CNS prophylaxis leads to both undertreatment (with half of relapses occurring among untreated patients with low or intermediate risk) and overtreatment, as >90% of high-risk patients did not experience a CNS relapse in a large clinical trial and in a retrospective cohort of >1000 individuals with DLBCL selected for CNS-directed therapy.9,34 Recent work described molecular risk factors for CNS recurrence, including HGBCL with MYC and BCL2 and/or BCL6 rearrangements, activated B-cell gene expression profile, CDKN2A/B deletions, as well as a mutational signature that includes MYD88 and CD79B mutations and correlates with extranodal invasion.3,39-42 After demonstration of cfDNA in the CSF of patients with brain metastases from solid tumors,43,44 several groups have leveraged this knowledge to detect specific mutations (particularly MYD88L265P) in the CSF of patients with CNS lymphoma.25,45,46 Bobillo et al identified specific single-nucleotide variants in the CSF of 6 patients with CNS-restricted lymphoma, but 5 of those had disease that was also detectable by standard cytology or flow cytometry.24 To identify somatic mutations, digital PCR specific to each variant was required, limiting application of this approach. This shortcoming can be overcome by deep NGS-based methods enabling simultaneous tracking of multiple mutations at high sensitivity.17,20,22,47 One advantage of methods relying on somatic mutations is the added value of identifying clinically important genomic alterations as well as their qualitative and quantitative evolutions.16,20 On the other hand, the clonotype-based NGS-MRD assay is applicable to any B-cell lymphoma, regardless of genomic characteristics. It involves a uniform, standardized method not affected by loss of prior somatic variants or acquisition of new ones. This assay can be easily integrated into current frameworks for MRD monitoring in lymphoid malignancies within the context of clinical trials or routine practice.15
The clonotypic DNA detected by our CSF assay showed no correlation with the plasma cfDNA or with the CSF contamination by blood during lumbar puncture, but further research should examine additional preanalytic variables that may affect the assay. Processing times, temperature, and additives affect the yield of cfDNA from body fluids.48 A PCR-based CSF assay in pediatric B-cell acute lymphoblastic lymphoma showed loss of DNA during routine storage and shipping of CSF at room temperature, which could be minimized by preservation in tissue culture or RPMI medium, or by handling at 4°C.49 We processed the CSF immediately and stored it in −80°C, yet the amount of clonotypic DNA was very low in cases of parenchymal-only or occult CNS disease (median copy count <5 per milliliter of CSF) and it may be affected preanalytically. Plasma-based MRD assays often use a single “dominant” sequence for longitudinal tracking, but evaluation of all trackable sequences may maximize the sensitivity in the CSF. The facts that the abundance of clonotypic DNA was higher overall in the “cell pellet” fraction than in the acellular fluid and that the DNA was sometimes detectable only in the spun-down pellet suggest that although truly “cell-free” DNA is detectable in the CSF, the NGS-MRD assay may often identify a very low tumor-derived cell content, below the sensitivity of standard tests. Using a spun-down CSF sample (as is already routinely obtained for cytospin CSF evaluation) may thus optimize sensitivity. Further aspects for investigation include repeated measurement of clonotypic DNA in the CSF to detect response to treatment or prophylaxis, or as surveillance after the initial therapy.
The association between the NGS-MRD assay in the CSF and clinical outcomes described in our study requires examination in a larger cohort. This study is the first, to our knowledge, to include prospective evaluation of a molecular CSF analysis as a prognostic biomarker in aggressive lymphoma, but it is limited by the low number of enrolled patients, of whom only 2 had a CNS recurrence. Furthermore, these patients had various aggressive lymphomas and received diverse systemic and CNS-directed therapies, which in some cases may have eradicated the microscopic source of clonotypic DNA in the CSF. To fully understand the prognostic value of the NGS-MRD CSF assay, a future cohort with uniform histology and treatment selection is necessary. We studied only patients at high clinical risk who underwent lumbar puncture as part of their medical care, so the potential value of the NGS-MRD assay in that situation is in refining the clinical risk prediction rather than replacing it. Determining performance characteristics of the assay would require testing patients at low clinical risk, but they do not undergo CSF sampling in clinical practice. Nevertheless, our proof-of-concept study proposes a more accurate approach to risk stratification, complementary to the CNS-IPI. The NGS-MRD assay split the clinical high-risk group (with an expected CNS relapse rate of ∼10%) into subgroups with a risk of 0% and 29%, although, admittedly, these estimates require a larger sample to be precise. CNS relapses in aggressive lymphoma typically occur within months of initial diagnosis and are believed to arise from occult disease already present before treatment initiation.2,9 Combining clinical factors with a highly accurate CSF assay may thus obviate unnecessary CNS prophylaxis for nearly two thirds of seemingly “high-risk” patients. Conversely, because many recent studies have questioned the efficacy of standard intrathecal prophylaxis,34,50,51 the subgroup with a positive NGS-MRD assay is a prime target for the study of novel strategies that could mitigate the increased risk of CNS recurrence.
Acknowledgment
Support for this study was provided by a collaborative agreement with Adaptive Biotechnologies, Seattle, WA.
Authorship
Contribution: A.J.O., H.K., and P.M.D. designed the research; A.J.O., A.D.C., M.P., T.A.O., A.Z., H.K., D.O.T., J.L.R., A.H., P.C.E., J.B., R.N., J.V., J.R., I.S., and P.M.D. acquired and processed the samples and clinical data; A.P.J. and C.D.M. supervised the sequencing, produced the sequencing data, and assisted with the interpretation of sequencing results; A.J.O. conducted statistical analyses; A.J.O., T.A.O., H.K., A.P.J., C.D.M., and P.M.D. interpreted the data; A.J.O., H.K., A.P.J., and .P.M.D. wrote the manuscript; and all authors approved the final version of the manuscript.
Conflict-of-interest disclosure: A.P.J. and C.D.M. are employees of Adaptive Biotechnologies. The remaining authors declare no competing financial interests.
Correspondence: Adam J. Olszewski, Rhode Island Hospital, 593 Eddy St, Providence, RI; 02903; e-mail: adam_olszewski@brown.edu.
References
Author notes
Presented in part as a poster at the 61st American Society of Hematology (ASH) Annual Meeting and Exposition, Orlando, FL, 7-10 December 2019; as a poster at the American Association for Cancer research (AACR) Annual Meeting 2020, 27-28 April 2020 and 22-24 June 2020, Philadelphia, PA; as a poster at the AACR Advances in Malignant Lymphoma Conference, 17-19 August 2020; and as an oral presentation at the 62nd ASH Annual Meeting and Exposition, 5-8 December 2020.
Clinical and sequencing data may be found in a data supplement available with the online version of this article. Additional data are available from the corresponding author upon request.
Requests for data sharing may be submitted to Adam J. Olszewski (adam_olszewski@brown.edu).
The full-text version of this article contains a data supplement.