Key Points
The condensed HDAC-123 regimen induces faster hematological recovery and therefore considerably reduces the length of hospital stay.
The condensed HDAC-123 regimen does not affect outcome and minimal residual disease response in younger AML patients.
Abstract
Postremission treatment is crucial to prevent relapse in acute myeloid leukemia (AML). High-dose cytarabine delivered every 12 hours on days 1, 3, and 5 (HDAC-135) is the standard of care for younger adult patients with AML. Although this standard has been unsuccessfully challenged by other treatment regimens, including multiagent chemotherapy, the timing of HDAC administration has attracted little attention. Here, we retrospectively compared the safety, efficacy, and health care resource consumption associated with HDAC-135 and another standard, condensed HDAC-123 regimen, as consolidation treatment in younger AML patients in first complete response. This study included 221 patients (median age, 46.6 years; range, 18-60 years). HDAC-123 and HDAC-135 were used in 92 and 129 patients, respectively. Both regimens were associated with similar rates of relapse-free survival, cumulative incidence of relapse, nonrelapse mortality, and overall survival, including in core binding factor AML subgroup in which levels of minimal residual disease reduction were similar in both schedules. Hematological recovery times regarding neutrophils and platelets were significantly shorter in patients receiving HDAC-123, with an average difference of 3 to 4 days for each consolidation cycle. The total duration of hospitalization for the whole postremission program was shorter with HDAC-123 (32 days; interquartile ratio [IQR], 22.0,36.5) compared with HDAC-135 (41 days; IQR, 30.5, 50.0) (P < .0001). In conclusion, the condensed HDAC-123 regimen induced faster hematological recovery and therefore significantly reduced the length of hospital stay without affecting treatment response or outcome in younger AML patients.
Introduction
The treatment of younger patients with newly diagnosed acute myeloid leukemia (AML) consists of 2 phases (ie, remission-inducing chemotherapy and consolidation), which are both crucial for cure. Following induction chemotherapy, most patients (>70%) do achieve complete remission (CR) with a very low mortality rate and enter the consolidation phase.1 This postremission therapy, the objective of which is to prevent relapse, is based on repeated courses of intermediate- to high-dose cytarabine with or without allogeneic stem cell transplantation (SCT) according to relapse risk. The standard consolidation chemotherapy regimen was established more than 25 years ago by a randomized phase 3 trial from the Cancer and Leukemia Group B, which stated that high-dose cytarabine delivered as a bolus infusion of 3000 mg/m2 every 12 hours on days 1, 3, and 5 (HDAC-135) was superior to continuous infusion at a dose of 100 or 400 mg/m2 per day over 5 days.2,3 Since this seminal study, the gap between 400 mg/m2 and 3000 mg/m2 has been studied in several reports and has shown that intermediate-dose cytarabine (1000-1500 mg/m2) could be as effective as HDAC.4,5
Although the optimal number of cytarabine courses as postremission treatment has been explored, the method of delivery of HDAC (ie, every other day) and the delay between courses of HDAC have not been explored in detail. Indeed, the rationale for delivery of HDAC-135 every other day has remained elusive. In the setting of active disease, such as frontline treatment or salvage for relapsed or refractory AML, it is necessary to monitor renal function carefully by daily measurement of creatinine level to allow dose adjustment in the event of tumor lysis syndrome. In the pivotal trial of postremission treatment, the HDAC regimen was given on days 1, 3, and 5 to ensure equivalent 5-day duration of exposure in the 3 comparative arms.2
This retrospective study was performed to compare the safety, efficacy, and health care resource consumption of HDAC-135 and HDAC-123 regimens as postremission treatment of patients in first CR after 1 cycle of induction chemotherapy.
Methods
Patients and treatments
This retrospective study included patients with newly diagnosed de novo or secondary AML according to the World Health Organization classification,6 excluding acute promyelocytic leukemia, who received at least 1 cycle of HDAC as postremission strategy between 1 January 2008, and 31 June 2017. Patients were included in the present study if they were ≥18 and ≤60 years of age, treated with intensive chemotherapy, and in CR or CR with incomplete hematological recovery (CRi) after 1 course of intensive induction chemotherapy. The study population consisted of CR1/CRi1 AML patients who received 1 to 3 cycles of HDAC 3 g/m2 every 12 hours for 3 days (18 g/m2) per 1 of 2 schedules: HDAC-123 (3 g/m2 per 12 hours, days 1, 2, and 3) or HDAC-135 (3 g/m2 per 12 hours, days 1, 3, and 5). In general, the standard HDAC-135 schedule was used in clinical trials, whereas the condensed HDAC-123 schedule was delivered in a routine setting. Patients in HDAC-123 and HDAC-135 arms were treated in parallel in the same periods. In the same way, the prophylactic use of granulocyte colony-stimulating factor (G-CSF), either the pegylated formulation of G-CSF, pegfilgrastim (6 mg on day 5 with HDAC-123 or day 7 with HDAC-135 in a routine setting), or standard daily dose of G-CSF (5 μg/kg per day from day 8 in clinical trials), was recommended. Patients who received G-CSF in priming were excluded. In our practice, patients receive HDAC treatment on an inpatient basis and are then discharged on day 4 after HDAC-123 or day 6 after HDAC-135. All patients are systematically readmitted for management of pancytopenia on days 10 to 12 according to blood cell counts. No bacterial prophylaxis with quinolone or other antibiotics was used. Primary refractory AML was defined as a failure to achieve CR1/CRi1 after induction chemotherapy, and such cases were not included in the present study. Patients who received multiagent chemotherapy as a postremission strategy were also excluded. Written informed consent was obtained from all patients in accordance with the Declaration of Helsinki, allowing the collection of clinical data in the anonymized French Toulouse-Bordeaux DATAML registry. Institutional review board approval (DR-2015-529) was received.
Cytogenetic risk classification was defined according to the UK Medical Research Council classification.7 Intensive induction chemotherapy was based on daunorubicin at a daily dose of 60 to 90 mg/m2 for 3 days or idarubicin at a daily dose of 8 to 9 mg/m2 for 5 days, together with continuous intravenous infusion of cytarabine at a daily dose of 100 to 200 mg/m2 for 7 days.8 Bone marrow (BM) assessment was performed in patients treated with intensive chemotherapy after hematological recovery or, in the case of delayed recovery, between days 35 and 45. Response to treatment, relapse, relapse-free survival (RFS), cumulative incidence of relapse (CIR), nonrelapse mortality (NRM), and overall survival (OS) were defined according to the European Leukemia Net (ELN) criteria.1
Minimal residual disease (MRD) levels were determined by serial monitoring of RUNX1-RUNX1T1 or CBFB-MYH11 messenger RNA expression by reverse transcription quantitative polymerase chain reaction. MRD evaluation was scheduled in BM and blood samples at diagnosis, and then before initiation of the first, second, and third HDAC cycle in both arms (MRD1, MRD2, and MRD3 time points, respectively), and 3 months after the end of treatment (MRD4).
Statistical analysis
The patients’ characteristics at diagnosis are described using numbers and frequencies for qualitative data, and the mean ± standard deviation or median, interquartile range (IQR), and range (minimum-maximum) for quantitative data. Categorical variables were compared between HDAC-123 and HDAC-135 arms using the χ2 test (or Fisher’s exact test when necessary). Student t test was used to compare the distributions of continuous data (Mann-Whitney U test was used when the distribution departed significantly from normality or when homoscedasticity was rejected). For white blood cell (WBC) (>1.0 × 109/L), platelet (>50.0 × 109/L), and neutrophil (>0.5 × 109/L) recovery delay (from day 1 of chemotherapy), RFS, and OS, differences in survival functions between HDAC-123 and HDAC-135 arms were described using median with IQR and tested using the log-rank test. For relapse (CIR), cumulative incidence functions were drawn (because NRM was used as a competing event) and compared using Gray’s test. Adjusted hazard ratios (aHR) and 95% confidence intervals (95% CI) were assessed using a standard Cox model for neutrophil recovery delay, RFS, and OS, and a proportional subdistribution hazard model (an extension of the Cox model) for competing risks for CIR.9 For the incidence of microbiologically documented bacteremia during postremission treatment, adjusted odds ratios (aOR) and 95% CI, were assessed using a standard logistic regression model. Multivariate analyses included HDAC-123 vs HDAC-135 together with potential confounding factors (center, ELN 2010 prognosis, AML status [de novo or secondary AML], age, performance status [for neutrophil recovery delay, bacteremia during postremission treatment, RFS, CIR, and OS], number of HDAC cycles, prophylactic G-CSF [for neutrophil recovery delay and bacteremia during postremission treatment], WBC at diagnosis, delay between first induction course and consolidation cycle 1 plus delay among all 3 consolidation cycles [for RFS, CIR, and OS], and allogeneic SCT in CR1/CRi1 [for RFS and CIR]) associated with end points with P < .20 in univariate analyses. Stepwise regression analysis was then used to assess variables that were significantly and independently associated with the endpoints (P < .05). The proportional hazard assumption was tested for each covariate of the Cox model using log-log plot curves and was always supported. When the linear hypothesis was not supported, continuous potential confounding factors were transformed into ordered data. Interactions between variables that were significantly and independently associated with endpoints were tested in the final models. None were significant. Allogeneic SCT in CR1/CRi1 was evaluated as a time-dependent qualitative covariate. All reported P values were 2-sided, and the significance threshold was <.05. Statistical analyses were performed using STATA, version 14.2 (STATA Corp., College Station, TX).
Results
Study population
Of 2914 patients with newly diagnosed AML included in the DATAML registry between 2008 and 2017, a total of 221 AML patients fulfilled the inclusion criteria (supplemental Figure 1), and were retrospectively included in this study: 92 (41.6%) in the HDAC-123 arm and 129 (58.4%) in the HDAC-135 arm. Their characteristics are presented in Table 1. The median age of the cohort was 46.6 years (range, 18.7-60.8). There were no significant differences between the HDAC-123 and the HDAC-135 arms with respect to demographic features, disease characteristics, or prognostic features, including cytogenetics, FLT3 internal tandem duplication (FLT3-ITD), and NPM1 mutational status, whereas CEBPA mutations were more frequent in the HDAC-135 arm. A total of 144 patients (65.2%) received daunorubicin-based induction therapy and 77 patients (34.8%) received idarubicin-based induction therapy. Eight (10.4%) and 6 patients (6.3%) with ≥5% blasts in BM at day 15 received a second course at day 16 in HDAC-123 and HDAC-135 groups, respectively. Twenty-five (27.2%) and 26 patients (20.2%) were admitted to an intensive care unit either during induction therapy or in the first 3 months following the first course of induction therapy in HDAC-123 and HDAC-135 arms, respectively (P = .22).
Baseline characteristics of 221 newly diagnosed AML patients in CR1/CRi1 receiving intensive treatment
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . | Total, N = 221 (100%) . |
|---|---|---|---|---|
| Age at diagnosis, y | .55 | |||
| Median (IQR) | 46.1 (36.2, 53.4) | 47.6 (37.2, 54.9) | 46.6 (36.5, 54.3) | |
| Range | 19.2-60.6 | 18.7-60.8 | 18.7-60.8 | |
| ECOG at diagnosis, n (%) | .16 | |||
| 0-1 | 65 (75.6) | 106 (83.5) | 171 (80.3) | |
| ≥2 | 21 (24.4) | 21 (16.5) | 42 (19.7) | |
| WBC at diagnosis, ×109/L | .59 | |||
| Median (IQR) | 17.5 (4.1, 76.7) | 13.8 (4.1, 47.7) | 14.1 (4.1, 55.3) | |
| Range | 0.8-236.0 | 0.9-342.0 | 0.8-342.0 | |
| AML status, n (%) | .48 | |||
| De novo | 84 (91.3) | 121 (93.8) | 205 (92.8) | |
| Secondary AML* | 8 (8.7) | 8 (6.2) | 16 (7.2) | |
| Cytogenetic risk, n (%) | .72 | |||
| Favorable | 33 (35.9) | 40 (31.0) | 73 (33.0) | |
| Intermediate | 48 (52.2) | 74 (57.4) | 122 (55.2) | |
| Adverse | 11 (12.0) | 15 (11.6) | 26 (11.8) | |
| ELN 2010 prognosis, n (%) | .96 | |||
| Favorable | 43 (47.8) | 61 (47.7) | 104 (47.7) | |
| Intermediate I/II | 36 (40.0) | 52 (40.6) | 88 (40.4) | |
| Adverse | 11 (12.2) | 15 (11.7) | 26 (11.9) | |
| FLT3-ITD, n (%) | .56 | |||
| Mutation | 17 (29.3) | 22 (25.0) | 107 (73.3) | |
| No mutation | 41 (70.7) | 66 (75.0) | 39 (26.7) | |
| NPM1, n (%) | .28 | |||
| Mutation | 22 (38.6) | 41 (47.7) | 63 (44.1) | |
| No mutation | 35 (61.4) | 45 (52.3) | 80 (55.9) | |
| CEBPA, n (%) | .03 | |||
| Single mutation | 1 (3.3) | 2 (2.7) | 3 (3.5) | |
| Double mutation | 0 (0) | 9 (16.7) | 10 (11.7) | |
| No mutation | 29 (96.7) | 43 (79.6) | 72 (84.7) |
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . | Total, N = 221 (100%) . |
|---|---|---|---|---|
| Age at diagnosis, y | .55 | |||
| Median (IQR) | 46.1 (36.2, 53.4) | 47.6 (37.2, 54.9) | 46.6 (36.5, 54.3) | |
| Range | 19.2-60.6 | 18.7-60.8 | 18.7-60.8 | |
| ECOG at diagnosis, n (%) | .16 | |||
| 0-1 | 65 (75.6) | 106 (83.5) | 171 (80.3) | |
| ≥2 | 21 (24.4) | 21 (16.5) | 42 (19.7) | |
| WBC at diagnosis, ×109/L | .59 | |||
| Median (IQR) | 17.5 (4.1, 76.7) | 13.8 (4.1, 47.7) | 14.1 (4.1, 55.3) | |
| Range | 0.8-236.0 | 0.9-342.0 | 0.8-342.0 | |
| AML status, n (%) | .48 | |||
| De novo | 84 (91.3) | 121 (93.8) | 205 (92.8) | |
| Secondary AML* | 8 (8.7) | 8 (6.2) | 16 (7.2) | |
| Cytogenetic risk, n (%) | .72 | |||
| Favorable | 33 (35.9) | 40 (31.0) | 73 (33.0) | |
| Intermediate | 48 (52.2) | 74 (57.4) | 122 (55.2) | |
| Adverse | 11 (12.0) | 15 (11.6) | 26 (11.8) | |
| ELN 2010 prognosis, n (%) | .96 | |||
| Favorable | 43 (47.8) | 61 (47.7) | 104 (47.7) | |
| Intermediate I/II | 36 (40.0) | 52 (40.6) | 88 (40.4) | |
| Adverse | 11 (12.2) | 15 (11.7) | 26 (11.9) | |
| FLT3-ITD, n (%) | .56 | |||
| Mutation | 17 (29.3) | 22 (25.0) | 107 (73.3) | |
| No mutation | 41 (70.7) | 66 (75.0) | 39 (26.7) | |
| NPM1, n (%) | .28 | |||
| Mutation | 22 (38.6) | 41 (47.7) | 63 (44.1) | |
| No mutation | 35 (61.4) | 45 (52.3) | 80 (55.9) | |
| CEBPA, n (%) | .03 | |||
| Single mutation | 1 (3.3) | 2 (2.7) | 3 (3.5) | |
| Double mutation | 0 (0) | 9 (16.7) | 10 (11.7) | |
| No mutation | 29 (96.7) | 43 (79.6) | 72 (84.7) |
ECOG, Eastern Cooperative Oncology Group performance status.
Non-de novo AML.
There were no differences in evolution of renal function or weight with the number of cycles between the 2 arms (Table 2). One, 2, or 3 cycles of HDAC were performed in 12 (13.0%), 32 (34.8%), and 48 (52.2%) patients, respectively, in the HDAC-123 arm and in 16 (12.4%), 36 (27.9%), and 77 (59.7%) patients, respectively, in the HDAC-135 arm, for a total of 539 HDAC cycles (supplemental Figure 1) (P = .50). Virtually all patients received prophylactic G-CSF except 1 (0.5%) patient during the first course, 5 (2.6%) during the second course, and 1 (0.8%) during the third course. In the HDAC-123 arm, 97.8%, 95.0%, and 95.7% of patients received pegfilgrastim after the first, second, and third HDAC course, respectively. In the HDAC-135 arm, 62.8%, 62.8%, and 66.2% of patients received pegfilgrastim after the first, second, and third HDAC course, respectively, with the remaining patients receiving standard G-CSF by daily injection until WBC recovery (>1.0 × 109/L) (P < .001 for each comparison HDAC-123 vs HDAC-135 by course 1, 2, or 3 for pegfilgrastim vs standard G-CSF use).
Baseline renal function, weight, G-CSF use, and transplantation rate at each HDAC cycle
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . |
|---|---|---|---|
| Creatinine at day 1 of each cycle, median (IQR), µM/L | |||
| Cycle 1 | 60.5 (52.5, 71.5) | 70.0 (57.0, 80.0) | .001 |
| Cycle 2 | 63.0 (55.0, 72.0) | 68.0 (58.0, 76.0) | .04 |
| Cycle 3 | 63.0 (57.0, 71.0) | 67.0 (57.0, 78.0) | .11 |
| Weight at day 1 of each cycle, median (IQR), kg | |||
| Cycle 1 | 70.6 (63.0, 81.0) | 69.5 (59.0, 82.0) | .34 |
| Cycle 2 | 73.0 (67.0, 83.0) | 71.0 (61.3, 84.0) | .23 |
| Cycle 3 | 74.0 (65.0, 85.5) | 72.0 (60.5, 82.0) | .23 |
| Prophylactic G-CSF, n (%) | |||
| Cycle 1 | <.001 | ||
| Standard G-CSF | 1 (1.1) | 48 (37.2) | |
| Pegylated G-CSF | 90 (97.8) | 81 (62.8) | |
| None | 1 (1.1) | 0 (0.0) | |
| Cycle 2 | <.001 | ||
| Standard G-CSF | 4 (5.0) | 37 (32.7) | |
| Pegylated G-CSF | 76 (95.0) | 71 (62.8) | |
| None | 0 (0.0) | 5 (4.4) | |
| Cycle 3 | <.001 | ||
| Standard G-CSF | 2 (4.3) | 25 (32.5) | |
| Pegylated G-CSF | 45 (95.7) | 51 (66.2) | |
| None | 0 (0.0) | 1 (1.3) | |
| Allogeneic SCT rate after each cycle, n (%) | .39 | ||
| Cycle 1 | 8 (8.7) | 11 (8.5) | |
| Cycle 2 | 30 (32.6) | 31 (24.0) | |
| Cycle 3 | 7 (7.6) | 7 (5.4) | |
| None | 47 (51.1) | 80 (62.0) |
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . |
|---|---|---|---|
| Creatinine at day 1 of each cycle, median (IQR), µM/L | |||
| Cycle 1 | 60.5 (52.5, 71.5) | 70.0 (57.0, 80.0) | .001 |
| Cycle 2 | 63.0 (55.0, 72.0) | 68.0 (58.0, 76.0) | .04 |
| Cycle 3 | 63.0 (57.0, 71.0) | 67.0 (57.0, 78.0) | .11 |
| Weight at day 1 of each cycle, median (IQR), kg | |||
| Cycle 1 | 70.6 (63.0, 81.0) | 69.5 (59.0, 82.0) | .34 |
| Cycle 2 | 73.0 (67.0, 83.0) | 71.0 (61.3, 84.0) | .23 |
| Cycle 3 | 74.0 (65.0, 85.5) | 72.0 (60.5, 82.0) | .23 |
| Prophylactic G-CSF, n (%) | |||
| Cycle 1 | <.001 | ||
| Standard G-CSF | 1 (1.1) | 48 (37.2) | |
| Pegylated G-CSF | 90 (97.8) | 81 (62.8) | |
| None | 1 (1.1) | 0 (0.0) | |
| Cycle 2 | <.001 | ||
| Standard G-CSF | 4 (5.0) | 37 (32.7) | |
| Pegylated G-CSF | 76 (95.0) | 71 (62.8) | |
| None | 0 (0.0) | 5 (4.4) | |
| Cycle 3 | <.001 | ||
| Standard G-CSF | 2 (4.3) | 25 (32.5) | |
| Pegylated G-CSF | 45 (95.7) | 51 (66.2) | |
| None | 0 (0.0) | 1 (1.3) | |
| Allogeneic SCT rate after each cycle, n (%) | .39 | ||
| Cycle 1 | 8 (8.7) | 11 (8.5) | |
| Cycle 2 | 30 (32.6) | 31 (24.0) | |
| Cycle 3 | 7 (7.6) | 7 (5.4) | |
| None | 47 (51.1) | 80 (62.0) |
Influence of HDAC schedule on hematological recovery, infection, and adverse event rates
During the 3 consolidation cycles, median hematological recovery times regarding WBC (>1.0 × 109/L) and neutrophils (>0.5 × 109/L) were significantly shorter with HDAC-123 compared with HDAC-135, whereas the median platelet recovery time (>50.0 × 109/L) was significantly shorter in the HDAC-123 arm only after the third HDAC cycle (Table 3). The average difference between both arms was 3 to 4 days for each consolidation cycle. Of note, neutrophil and platelet recovery times were stable following 3 consolidation cycles. Multivariate analyses of factors associated with neutrophil recovery showed that HDAC-135 was consistently associated with longer delay following all 3 consolidation cycles (aHR, 0.30; 95% CI, 0.22-0.41; P < .001 for cycle 1; aHR, 0.32, 95% CI, 0.23-0.45; P < .001 for cycle 2; aHR, 0.44, 95% CI, 0.30-0.65; P < .001 for cycle 3). Multivariate analyses of factors associated with platelet recovery showed that HDAC-135 was associated with longer delay only for the third consolidation cycle (aHR, 0.79; 95% CI, 0.56-1.10; P = .16 for cycle 1; aHR, 0.81; 95% CI, 0.56-1.17; P = .26 for cycle 2; aHR, 0.51; 95% CI, 0.32-0.81; P = .004 for cycle 3). We did not find significant reductions in median delay between induction chemotherapy and the first HDAC cycle, or between HDAC cycles (Table 3).
Impact of HDAC schedules on hematological recovery
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . |
|---|---|---|---|
| WBC >1.0 × 109/L recovery, median (IQR), d | |||
| Cycle 1 | 14 (13.0-15.0) | 17 (16.0-19.0) | <.0001 |
| Cycle 2 | 16 (15.0-17.0) | 19 (17.0-22.0) | <.0001 |
| Cycle 3 | 15 (15.0-17.0) | 19 (17.0-20.0) | <.0001 |
| Platelets >50.0 × 109/L recovery, median (IQR), d | |||
| Cycle 1 | 16 (15.0, 26.0) | 20 (18.0, 23.0) | .16 |
| Cycle 2 | 18 (16.0, 27.0) | 22 (19.0, 25.0) | .06 |
| Cycle 3 | 16 (16.0, 22.0) | 20 (19.0, 25.0) | <.01 |
| Neutrophils >0.5 × 109/L recovery, median (IQR), d | |||
| Cycle 1 | 15 (14.0, 16.0) | 18 (17.0, 20.0) | <.0001 |
| Cycle 2 | 16 (15.0, 17.0) | 20 (18.0, 22.0) | <.0001 |
| Cycle 3 | 16 (15.0, 17.0) | 19 (17.0, 21.0) | <.0001 |
| Delay between chemotherapies, median (IQR), d | |||
| Induction-cycle 1 | 41 (37.0, 50.0) | 42 (39.0, 49.0) | .61 |
| Cycle 1-cycle 2 | 36 (33.0, 42.5) | 37 (35.0, 44.0) | .07 |
| Cycle 2-cycle 3 | 37 (34.5, 50.5) | 39 (36.0, 47.0) | .54 |
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . |
|---|---|---|---|
| WBC >1.0 × 109/L recovery, median (IQR), d | |||
| Cycle 1 | 14 (13.0-15.0) | 17 (16.0-19.0) | <.0001 |
| Cycle 2 | 16 (15.0-17.0) | 19 (17.0-22.0) | <.0001 |
| Cycle 3 | 15 (15.0-17.0) | 19 (17.0-20.0) | <.0001 |
| Platelets >50.0 × 109/L recovery, median (IQR), d | |||
| Cycle 1 | 16 (15.0, 26.0) | 20 (18.0, 23.0) | .16 |
| Cycle 2 | 18 (16.0, 27.0) | 22 (19.0, 25.0) | .06 |
| Cycle 3 | 16 (16.0, 22.0) | 20 (19.0, 25.0) | <.01 |
| Neutrophils >0.5 × 109/L recovery, median (IQR), d | |||
| Cycle 1 | 15 (14.0, 16.0) | 18 (17.0, 20.0) | <.0001 |
| Cycle 2 | 16 (15.0, 17.0) | 20 (18.0, 22.0) | <.0001 |
| Cycle 3 | 16 (15.0, 17.0) | 19 (17.0, 21.0) | <.0001 |
| Delay between chemotherapies, median (IQR), d | |||
| Induction-cycle 1 | 41 (37.0, 50.0) | 42 (39.0, 49.0) | .61 |
| Cycle 1-cycle 2 | 36 (33.0, 42.5) | 37 (35.0, 44.0) | .07 |
| Cycle 2-cycle 3 | 37 (34.5, 50.5) | 39 (36.0, 47.0) | .54 |
Considering the whole population of patients receiving HDAC consolidation, the overall incidence rates of microbiologically documented bacteremia were 19.5%, 21.8%, and 29.6% after cycles 1, 2, and 3, respectively. The incidence of microbiologically documented bacteremia during postremission treatment was 35.9% in the HDAC-123 arm and 48.1% in the HDAC-135 arm (P = .25). There were also no statistically significant differences in terms of bacteremia for each HDAC-123 vs HDAC-135 cycle (Table 4). The mean cases of bacteremia per patient-HDAC cycle were 0.19 (range, 0.00-1.00) in the HDAC-123 arm and 0.25 (range, 0.00-1.00) in the HDAC-135 arm (P = .12). However, the incidence of documented Streptococcus sp. bacteremia during postremission treatment was significantly higher in the HDAC-135 arm than the HDAC-123 arm (9.3% vs 1.1%, respectively; P = .01). Logistic regression analysis did not identify HDAC-135 as an independent risk factor associated with microbiologically documented bacteremia during postremission treatment (aOR, 1.28; 95% CI, 0.69-2.38; P = .43), whereas the cumulative number of HDAC cycles (aOR, 2.71; 95% CI, 0.94-7.80; P = .07 and aOR, 4.11; 95% CI, 1.50-11.21; P < .01 for 2 and 3 cycles, respectively) and prophylactic pegfilgrastim use (aOR, 0.46; 95% CI, 0.23-0.90; P = .02 vs standard G-CSF) were significantly and independently associated with the incidence of bacteremia (Table 5). Other infectious adverse events, including fungal or viral infections, were uncommon with no difference in incidence between the HDAC-123 and HDAC-135 arms (Table 4). There were also no significant differences in incidence rates of cutaneous or mucosal adverse events except for the number of mucosal events per patient, which was higher in the HDAC-135 arm (P = .019). Only 2 patients in the HDAC-123 arm (2.2%) and 2 patients in the HDAC-135 arm (1.6%) had cerebellar neurotoxicity.
Incidence of infections and cytarabine-related adverse events according to HDAC schedule
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . |
|---|---|---|---|
| Microbiologically documented bacteremia, n (%) | |||
| Cycle 1 | 14 (15.2) | 29 (22.5) | .18 |
| Cycle 2 | 14 (17.5) | 28 (24.8) | .23 |
| Cycle 3 | 12 (25.0) | 25 (32.5) | .37 |
| Documented Streptococcus sp. bacteremia during postremission treatment, n (%) | 1 (1.1) | 12 (9.3) | .01 |
| IFI requiring systemic antifungal therapy, n (%) | |||
| Cycle 1 | 4 (4.3) | 2 (1.6) | .23 |
| Cycle 2 | 1 (1.3) | 4 (3.5) | .40 |
| Cycle 3 | 1 (2.1) | 2 (2.6) | 1 |
| Virus requiring systemic antiviral therapy, n (%) | |||
| Cycle 1 | 0 (0.0) | 2 (1.6) | .51 |
| Cycle 2 | 1 (1.3) | 3 (2.7) | .64 |
| Cycle 3 | 0 (0.0) | 1 (1.3) | 1 |
| Grade 3-4 mucositis, n (%) | |||
| Cycle 1 | 0 (0.0) | 5 (3.9) | .15 |
| Cycle 2 | 0 (0.0) | 1 (0.9) | 1 |
| Cycle 3 | 0 (0.0) | 0 (0.0) | — |
| Grade 1-2 erythema, n (%)* | |||
| Cycle 1 | 9 (9.8) | 20 (15.5) | .21 |
| Cycle 2 | 6 (7.5) | 5 (4.4) | .53 |
| Cycle 3 | 4 (8.3) | 2 (2.6) | .20 |
| Acute cerebellar syndrome, n (%) | |||
| Cycle 1 | 2 (2.2) | 2 (1.6) | 1 |
| Cycle 2 | 0 (0.0) | 0 (0.0) | — |
| Cycle 3 | 0 (0.0) | 0 (0.0) | — |
| . | HDAC-123, n = 92 (41.6%) . | HDAC-135, n = 129 (58.4%) . | P . |
|---|---|---|---|
| Microbiologically documented bacteremia, n (%) | |||
| Cycle 1 | 14 (15.2) | 29 (22.5) | .18 |
| Cycle 2 | 14 (17.5) | 28 (24.8) | .23 |
| Cycle 3 | 12 (25.0) | 25 (32.5) | .37 |
| Documented Streptococcus sp. bacteremia during postremission treatment, n (%) | 1 (1.1) | 12 (9.3) | .01 |
| IFI requiring systemic antifungal therapy, n (%) | |||
| Cycle 1 | 4 (4.3) | 2 (1.6) | .23 |
| Cycle 2 | 1 (1.3) | 4 (3.5) | .40 |
| Cycle 3 | 1 (2.1) | 2 (2.6) | 1 |
| Virus requiring systemic antiviral therapy, n (%) | |||
| Cycle 1 | 0 (0.0) | 2 (1.6) | .51 |
| Cycle 2 | 1 (1.3) | 3 (2.7) | .64 |
| Cycle 3 | 0 (0.0) | 1 (1.3) | 1 |
| Grade 3-4 mucositis, n (%) | |||
| Cycle 1 | 0 (0.0) | 5 (3.9) | .15 |
| Cycle 2 | 0 (0.0) | 1 (0.9) | 1 |
| Cycle 3 | 0 (0.0) | 0 (0.0) | — |
| Grade 1-2 erythema, n (%)* | |||
| Cycle 1 | 9 (9.8) | 20 (15.5) | .21 |
| Cycle 2 | 6 (7.5) | 5 (4.4) | .53 |
| Cycle 3 | 4 (8.3) | 2 (2.6) | .20 |
| Acute cerebellar syndrome, n (%) | |||
| Cycle 1 | 2 (2.2) | 2 (1.6) | 1 |
| Cycle 2 | 0 (0.0) | 0 (0.0) | — |
| Cycle 3 | 0 (0.0) | 0 (0.0) | — |
IFI, invasive fungal infection.
No grade 3-4 erythema.
Logistic regression model for factors associated with microbiologically documented bacteremia during postremission treatment
| . | . | . | Multivariate analysis . | ||
|---|---|---|---|---|---|
| . | n . | No. of events . | aOR . | 95% CI . | P . |
| HDAC regimen | |||||
| HDAC-123 | 91 | 33 | 1 | — | — |
| HDAC-135 | 129 | 62 | 1.28 | 0.69-2.38 | .43 |
| Prophylactic G-CSF* | |||||
| Standard G-CSF | 49 | 27 | 1 | — | — |
| Pegylated G-CSF | 171 | 68 | 0.46 | 0.23-0.90 | .02 |
| No. of HDAC cycles | |||||
| 1 | 27 | 6 | 1 | — | — |
| 2 | 68 | 27 | 2.71 | 0.94-7.79 | .06 |
| 3 | 125 | 62 | 4.11 | 1.50-11.21 | <.01 |
| . | . | . | Multivariate analysis . | ||
|---|---|---|---|---|---|
| . | n . | No. of events . | aOR . | 95% CI . | P . |
| HDAC regimen | |||||
| HDAC-123 | 91 | 33 | 1 | — | — |
| HDAC-135 | 129 | 62 | 1.28 | 0.69-2.38 | .43 |
| Prophylactic G-CSF* | |||||
| Standard G-CSF | 49 | 27 | 1 | — | — |
| Pegylated G-CSF | 171 | 68 | 0.46 | 0.23-0.90 | .02 |
| No. of HDAC cycles | |||||
| 1 | 27 | 6 | 1 | — | — |
| 2 | 68 | 27 | 2.71 | 0.94-7.79 | .06 |
| 3 | 125 | 62 | 4.11 | 1.50-11.21 | <.01 |
*Prophylactic G-CSF during first cycle of HDAC.
Influence of HDAC schedule on health care resource consumption
The requirement for red blood cell and platelet transfusions had a median of ∼2 to 3 units per patient-HDAC cycle, and there was no significant difference between the 2 arms (supplemental Table 1). There were also no differences in terms of intensive care unit admission during postremission treatment in the HDAC-123 arm (1.1%, 2.5%, and 6.3% during cycles 1, 2, and 3, respectively) compared with the HDAC-135 arm (0.0%, 4.4%, and 2.6% during cycles 1, 2, and 3, respectively). Despite a significant reduction in neutrophil recovery time with HDAC-123 compared with HDAC-135 following each cycle, there was no significant decrease in median duration of antibiotic treatment between the 2 arms (supplemental Table 1). Finally, the shorter median recovery time for neutrophils and platelets by an average of 3 to 4 days for all 3 consolidation cycles in the HDAC-123 arm translated into a significant decrease in period of hospitalization during each cycle and, thus, for the whole postremission program: 32 days (IQR, 22.0, 36.5; range, 8.0-69.0) in the HDAC-123 arm compared with 41 days (IQR, 30.5, 50.0; range, 10.0-75.0) in the HDAC-135 arm (P < .0001).
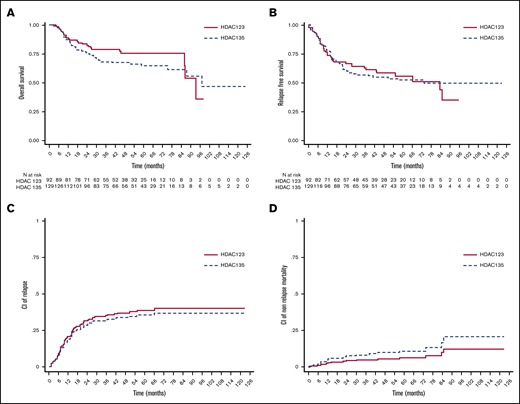
Influence of HDAC schedule on survival, relapse, and nonrelapse mortality
The median follow‐up periods were 53.2 months (IQR, 38.2, 63.7) in the HDAC-123 arm and 60.8 months (IQR, 42.7, 74.1) in the HDAC-135 arm. The median OS was 93.2 months (IQR, 85.8, not reached [NR]) in the HDAC-123 arm and 97.0 months (IQR, 25.8, NR) in the HDAC-135 arm (Figure 1A) (P = .23). Factors significantly associated with OS in multivariate analyses were ELN 2010 intermediate prognosis (aHR, 2.93; 95% CI, 1.62-5.32; P < .001), ELN 2010 adverse prognosis (aHR, 4.86; 95% CI, 2.32-10.19; P < .001), and delay between cycle 1 and cycle 2 ≥40 days (aHR, 1.89; 95% CI, 1.10-3.24; P = .02) (Table 6). The median RFS was 83.5 months (IQR, 14.2, NR) in the HDAC-123 arm and 73.6 months (IQR, 11.9, NR) in the HDAC-135 arm (Figure 1B) (P = .77). Factors significantly associated with RFS in multivariate analyses were ELN 2010 intermediate prognosis (aHR, 2.64; 95% CI, 1.67-4.18; P < .001) and ELN 2010 adverse prognosis (aHR, 3.55; 95% CI, 1.97-6.41; P < .001) (Table 6). Five-year CIR was 38.6% (95% CI, 31.5-45.7) in the HDAC-123 arm and 36.2% (95% CI, 29.70-42.76) in the HDAC-135 arm (Figure 1C) (P = .64). Factors significantly associated with CIR in multivariate analyses were ELN 2010 intermediate prognosis (aHR, 2.71; 95% CI, 1.62-4.51; P < .001) and ELN 2010 adverse prognosis (aHR, 3.42; 95% CI, 1.70-6.90; P = .001) (Table 6). Five-year NRM was 8.2% (95% CI, 4.95-12.46) in the HDAC-123 arm and 11.1% (95% CI, 6.32-17.44) in the HDAC-135 arm (Figure 1D) (P = .22). Allogeneic SCT as time dependent covariate was the only factor associated with NRM in multivariate analyses (aHR, 4.95; 95% CI, 1.84-13.34; P = .002). Therefore, HDAC-123 and HDAC-135 regimens were not independently associated with OS, RFS, CIR, or NRM.
Outcomes among 221 patients with newly diagnosed acute myeloid leukemia. Overall survival by treatment arm (A); relapse-free survival by treatment arm (B); cumulative incidence (CI) of relapse by treatment arm (C); and cumulative incidence of nonrelapse mortality by treatment arm (D).
Outcomes among 221 patients with newly diagnosed acute myeloid leukemia. Overall survival by treatment arm (A); relapse-free survival by treatment arm (B); cumulative incidence (CI) of relapse by treatment arm (C); and cumulative incidence of nonrelapse mortality by treatment arm (D).
Cox model for factors associated with overall survival, relapse-free survival, cumulative incidence of relapse, and nonrelapse mortality
| . | n . | No. of events . | aHR . | 95% CI . | P . |
|---|---|---|---|---|---|
| Overall survival | |||||
| HDAC regimen | |||||
| 123 | 92 | 24 | 1 | — | — |
| 135 | 129 | 46 | 1.40 | 0.85-2.31 | .19 |
| ELN 2010 prognosis | |||||
| Favorable | 104 | 17 | 1 | — | — |
| Intermediate | 88 | 35 | 2.93 | 1.62-5.32 | <.001 |
| Adverse | 26 | 17 | 4.86 | 2.32-10.19 | <.001 |
| Delay between cycle 1 and 2 | |||||
| <40 d | 116 | 26 | 1 | — | — |
| ≥40 d | 77 | 29 | 1.89 | 1.10-3.24 | .02 |
| No cycle 2 | 28 | 15 | 2.05 | 1.02-4.13 | .04 |
| Relapse-free survival | |||||
| HDAC regimen | |||||
| 123 | 92 | 40 | 1 | — | — |
| 135 | 129 | 60 | 1.10 | 0.73-1.64 | .65 |
| ELN 2010 prognosis | |||||
| Favorable | 104 | 29 | 1 | — | — |
| Intermediate | 88 | 52 | 2.64 | 1.67-4.18 | <.001 |
| Adverse | 26 | 18 | 3.55 | 1.97-6.41 | <.001 |
| Cumulative incidence of relapse | |||||
| HDAC regimen | |||||
| 123 | 92 | 34 | 1 | — | — |
| 135 | 129 | 45 | 0.89 | 0.56-1.41 | .63 |
| ELN 2010 prognosis | |||||
| Favorable | 104 | 22 | 1 | — | — |
| Intermediate | 88 | 43 | 2.70 | 1.63-4.51 | <.001 |
| Adverse | 26 | 14 | 3.41 | 1.69-6.90 | .001 |
| Nonrelapse mortality | |||||
| HDAC regimen | |||||
| 123 | 92 | 6 | 1 | — | — |
| 135 | 129 | 15 | 2.27 | 0.85-6.01 | .10 |
| Allogeneic SCT | |||||
| No | 127 | 6 | 1 | — | — |
| Yes | 94 | 15 | 4.95 | 1.84-13.34 | .002 |
| . | n . | No. of events . | aHR . | 95% CI . | P . |
|---|---|---|---|---|---|
| Overall survival | |||||
| HDAC regimen | |||||
| 123 | 92 | 24 | 1 | — | — |
| 135 | 129 | 46 | 1.40 | 0.85-2.31 | .19 |
| ELN 2010 prognosis | |||||
| Favorable | 104 | 17 | 1 | — | — |
| Intermediate | 88 | 35 | 2.93 | 1.62-5.32 | <.001 |
| Adverse | 26 | 17 | 4.86 | 2.32-10.19 | <.001 |
| Delay between cycle 1 and 2 | |||||
| <40 d | 116 | 26 | 1 | — | — |
| ≥40 d | 77 | 29 | 1.89 | 1.10-3.24 | .02 |
| No cycle 2 | 28 | 15 | 2.05 | 1.02-4.13 | .04 |
| Relapse-free survival | |||||
| HDAC regimen | |||||
| 123 | 92 | 40 | 1 | — | — |
| 135 | 129 | 60 | 1.10 | 0.73-1.64 | .65 |
| ELN 2010 prognosis | |||||
| Favorable | 104 | 29 | 1 | — | — |
| Intermediate | 88 | 52 | 2.64 | 1.67-4.18 | <.001 |
| Adverse | 26 | 18 | 3.55 | 1.97-6.41 | <.001 |
| Cumulative incidence of relapse | |||||
| HDAC regimen | |||||
| 123 | 92 | 34 | 1 | — | — |
| 135 | 129 | 45 | 0.89 | 0.56-1.41 | .63 |
| ELN 2010 prognosis | |||||
| Favorable | 104 | 22 | 1 | — | — |
| Intermediate | 88 | 43 | 2.70 | 1.63-4.51 | <.001 |
| Adverse | 26 | 14 | 3.41 | 1.69-6.90 | .001 |
| Nonrelapse mortality | |||||
| HDAC regimen | |||||
| 123 | 92 | 6 | 1 | — | — |
| 135 | 129 | 15 | 2.27 | 0.85-6.01 | .10 |
| Allogeneic SCT | |||||
| No | 127 | 6 | 1 | — | — |
| Yes | 94 | 15 | 4.95 | 1.84-13.34 | .002 |
Influence of HDAC schedule on core binding factor AML
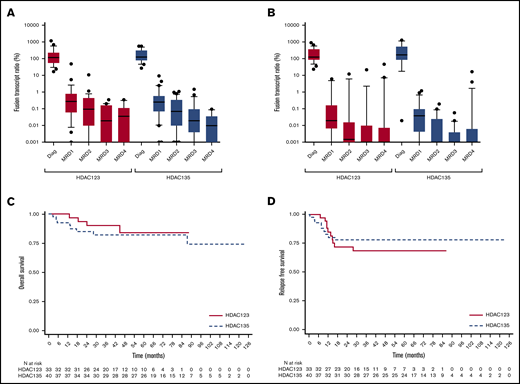
We then focused our analyses on patients with core binding factor (CBF)-AML because HDAC consolidation has proven particular efficacious in this subset and most patients usually complete 3 cycles without the need for allogeneic SCT in CR1. Moreover, the depth of disease response can be evaluated with MRD monitoring during postremission therapy. Thirty-three patients received the HDAC-123 schedule, with 27 (81.8%) completing 3 HDAC cycles, whereas 40 patients received the HDAC-135 schedule, with 34 (85.0%) completing 3 HDAC cycles (supplemental Table 2). Median hematological recovery times for neutrophils but not platelets were significantly shorter with HDAC-123 compared with HDAC-135 (supplemental Table 2). The incidence of microbiologically documented bacteremia during postremission treatment in CBF-AML patients was 33.3% in the HDAC-123 arm and 60.0% in the HDAC-135 arm (P = .06). The mean incidence of bacteremia per patient-HDAC cycle was significantly lower in the HDAC-123 arm than the HDAC-135 arm (0.13; range, 0.00-0.67 vs 0.33; range, 0.00-1.00, respectively; P = .008). The median durations of hospitalization for each cycle (supplemental Table 2) and for the whole postremission program were significantly shorter in the HDAC-123 arm (35.0 days; IQR, 31.0, 41.0) than the HDAC-135 arm (46.5 days; IQR, 39.0, 56.5) (P < .0001).
Median BM MRD levels at diagnosis (120.0 vs 128.5, respectively; P = .35), postinduction MRD1 (0.28 vs 0.27, respectively; P = .87), post-cycle 1 MRD2 (0.097 vs 0.070, respectively; P = .67), post-cycle 2 MRD3 (0.020 vs 0.020, respectively; P = .98), and post-cycle 3 MRD4 (0.035 vs 0.010, respectively; P = .32) were comparable in the HDAC-123 and HDAC-135 arms (Figure 2A). Moreover, BM MRD decreased similarly in both arms with a median log reduction between diagnosis and MRD2 of 3.05 log (IQR, 3.65, 2.47) vs 3.14 log (IQR, 3.83, 2.78) (P = .27) in HDAC-123 and HDAC-135 arms, respectively. The median OS and RFS of CBF-AML patients did not differ significantly according to treatment arm (Figure 2B-C).
Reduction of fusion transcript ratio in 73 CBF AML patients. Thirty-three (45.2%) in the HDAC-123 arm and 40 (54.8%) in the HDAC-135 arm, at CR1/CRi1, median ratio at diagnosis (Diag), and at the MRD1, MRD2, MRD3, and MRD4 time points, for the HDAC-123 arm (red bars) and HDAC-135 arm (blue bars), in bone marrow (A) and in blood (B). Outcomes among patients with newly diagnosed CBF-AML in CR1/CRi1: overall survival by treatment arm (n = 73; P = .54) (C) and relapse-free survival by treatment arm (n = 73; P = .52) (D).
Reduction of fusion transcript ratio in 73 CBF AML patients. Thirty-three (45.2%) in the HDAC-123 arm and 40 (54.8%) in the HDAC-135 arm, at CR1/CRi1, median ratio at diagnosis (Diag), and at the MRD1, MRD2, MRD3, and MRD4 time points, for the HDAC-123 arm (red bars) and HDAC-135 arm (blue bars), in bone marrow (A) and in blood (B). Outcomes among patients with newly diagnosed CBF-AML in CR1/CRi1: overall survival by treatment arm (n = 73; P = .54) (C) and relapse-free survival by treatment arm (n = 73; P = .52) (D).
Discussion
In the present study, we retrospectively compared 2 different schedules of HDAC 3000 mg/m2 every 12 hours for 3 days (18 g/m2 total dose), and the results showed that, although both regimens were associated with similar RFS, CIR, and OS, there was considerable difference in terms of hematological toxicity. Patients receiving the HDAC-123 regimen spent 9 days less in hospital over the whole period of postremission treatment. Indeed, clinically relevant durations of leukopenia, neutropenia, and thrombocytopenia were significantly shortened by 3 to 4 days with use of the HDAC-123 regimen compared with the HDAC-135 regimen. The HDAC-123 arm was also associated with a lower rate of documented Streptococcus sp. bacteremia, although the overall incidence of microbiologically documented bacteremia was not significantly different between the 2 groups. The HDAC-123 regimen was significantly associated with fewer cases of bacteremia in CBF-AML patients. Interestingly, multivariate analysis revealed that pegfilgrastim use was significantly associated with a lower incidence of bacteremia compared with standard G-CSF. In a phase 2 randomized clinical trial comparing pegfilgrastim and the standard filgrastim G-CSF in AML patients, both formulations were shown to be effective in reducing neutropenia duration and incidence of febrile neutropenia, but bacteremia was not reported in this trial.10 The reason for this apparent protective effect of pegfilgrastim in the present study remains unclear, and further investigations are required. Because the dose and type of G-CSF were not controlled in this study, these results should be interpreted with caution.
To our knowledge, this is the second study to assess retrospectively the impact of HDAC schedule in the consolidation treatment of younger AML patients in first CR. Indeed, the German-Austrian Acute Myeloid Leukemia Study Group (AMLSG) also compared the impact of condensed vs standard HDAC in AML patients.11 Several methodological differences must nevertheless be highlighted between the 2 studies. The AMLSG study was an analysis of prospective data from 2 clinical trials.12,13 Induction chemotherapy before postremission treatment in the AMLSG study was somewhat different from ours with the randomized addition of all-trans retinoic acid or valproic acid and all patients received double induction chemotherapy, including 2 cycles of idarubicin, cytarabine, and etoposide, or 2 cycles of daunorubicin-based 3 + 7 therapy. During consolidation, pegfilgrastim was given on day 8 after HDAC-123 and on day 10 after HDAC-135, whereas some patients did not receive prophylactic G-CSF. In the present study, almost all patients received prophylactic G-CSF, and pegfilgrastim was given sooner, on day 5 or day 7, according to HDAC schedule. Despite these differences, both studies reached the same major conclusions, including a 4-day reduction in duration of neutropenia, lower rates of infection (defined as both microbiologically documented infection and/or febrile neutropenia in the AMLSG study), shorter hospitalization period, and similar survival end points with HDAC-123 compared with HDAC-135. In addition, we did not observe any cumulative hematological toxicity with increasing number of HDAC cycles, as in the AMLSG study. However, we did not find any reduction in platelet transfusion rate following HDAC-123 in contrast to the AMLSG study. The median number of platelet transfusions following HDAC-135 was 6 to 8 in the AMLSG study but only 2 to 3 in our study, likely reflecting differences in routine practice regarding the platelet threshold for transfusion.
To date, the prognostic impact of time interval between HDAC cycles has not been explored in AML. However, the concept of dose intensity has been established in diffuse large B-cell lymphoma14,15 or even in acute lymphoblastic leukemia.16 We found that a delay ≥40 days between HDAC cycles 1 and 2 was independently and significantly associated with poorer OS rate. We have no clear explanation for this intriguing result, which should be interpreted with caution and should prompt additional investigations. If confirmed, this could have important implications for routine practice.
The main limitation of the present study was its retrospective nature. We could not exclude selection bias, which could only be addressed by a prospective randomized study. However, because our results were the same as the AMLSG study, we recommend broadly adopting the HDAC-123 regimen for both routine and clinical trials in younger AML patients, as in the ELN 2017 recommendations. The question remains open in older AML patients for whom postremission treatment is not standardized.
In conclusion, by reducing hematological toxicity using a condensed HDAC regimen in routine practice instead of the standard regimen, we reduced the hospitalization period in our patients by several days. Registry studies questioning our long-established practices, sometimes based on limited background, remain relevant because they can help to improve treatment safety and quality of life but also limit health care costs.
Send data sharing requests via e-mail to the corresponding author, Pierre-Yves Dumas, at pierre-yves.dumas@u-bordeaux.fr.
Acknowledgments
The English in this document has been checked by at least 2 professional editors, both native speakers of English. For a certificate, please see: http://www.textcheck.com/certificate/TFq6bn. The authors thank all the members of the Gaël Adolescent Espoir Leucémie association, the Toulouse Cancer Santé Foundation, and the FONROGA Foundation and the “Cancéropôle Grand Sud-Ouest et le Groupement Interrégional de Recherche Clinique et d’Innovation Sud-Ouest Outre-Mer” for the “Appel à Projets Interrégional Cancer 2016 (API-K).”
This study was funded by the data management unit of Toulouse University Hospital and the Cancer Pharmacology of Toulouse Oncopole and Region project (ANR-11-PHUC-001), enabling e-CRF.
Authorship
Contribution: P.-Y.D., S.B., E.B., and C.R. designed research; P.-Y.D., S.B., T.L., S.T., J.G., C.A., A.B., E.D., J.B.R., J.-P.V., F.V., N.L., I.L., E.K., A.S., H.R., A.-C.d.G., F.D., A.P., and C.R. performed research; P.-Y.D., E.B., and C.R analyzed data; P.-Y.D., E.B., and C.R wrote the paper; and all authors have read and agreed to the published version of the manuscript.
Conflict-of-interest disclosure: P.-Y.D. has served on advisory boards for Daiichi-Sankyo and Astellas. S.B. has served on advisory boards for Daiichi-Sankyo, Astellas, Sanofi, and Jazz Pharmaceuticals. A.B. has served on advisory boards for Daiichi-Sankyo and Novartis. A.P. has received research grants to his institution from Incyte, Janssen, Gilead, Sanofi, Amgen, Novartis, Celgene, Jazz Pharma, Daiichi-Sankyo, Astellas, Roche; and served on advisory boards for Sanofi, Takeda, AbbVie, Janssen, Jazz Pharma, Daiichi-Sankyo, Astellas, Novartis, Celgene, Otsuka, Sunesis, Roche, and Pfizer. C.R. has received research grants to his institution from AbbVie, Amgen, Novartis, Celgene, Jazz Pharma, Agios, Daiichi-Sankyo, Astellas, Sunesis, Roche, and MaatPharma; and served on advisory boards for AbbVie, Janssen, Jazz Pharma, Daiichi-Sankyo, Astellas, Novartis, Celgene, Otsuka, Sunesis, Roche, Otsuka, Macrogenics, and Pfizer. The remaining authors declare no competing financial interests.
Correspondence: Pierre-Yves Dumas, CHU Bordeaux, Hématologie Clinique et Thérapie Cellulaire, F-33000 Bordeaux, France; e-mail: pierre-yves.dumas@u-bordeaux.fr; or Christian Récher, Service d’Hématologie, Institut Universitaire du Cancer de Toulouse Oncopole, 1 Av Irène Joliot-Curie, 31059 Toulouse cedex 9, France; e-mail: recher.christian@iuct-oncopole.fr.
References
Author notes
P.-Y.D. and S.B. are joint first authors.
A.P. and C.R. are joint last authors.
The full-text version of this article contains a data supplement.