Key Points
Pembrolizumab can be safely given as consolidation after ASCT for R/R DLBCL.
The 18-month PFS observed in this trial does not support a larger confirmatory study.
Abstract
Disease relapse remains the leading cause of failure after autologous stem cell transplantation (ASCT) for patients with relapsed/refractory diffuse large B-cell lymphoma (R/R DLBCL). We conducted a phase 2, multicenter, single-arm study of the anti–PD-1 monoclonal antibody pembrolizumab given after ASCT in patients with chemosensitive DLBCL, hypothesizing that it would improve the progression-free survival (PFS) at 18 months after ASCT (primary endpoint) from 60% to 80%. Pembrolizumab was administered at 200 mg IV every 3 weeks for up to 8 cycles, starting within 21 days of post-ASCT discharge. Twenty-nine patients were treated on this study; 62% completed all 8 cycles. Seventy-nine percent of patients experienced at least one grade 3 or higher adverse event, and 34% experienced at least one grade 2 or higher immune-related adverse event. Overall, 59% of patients were alive and progression free at 18 months, which did not meet the primary endpoint. The 18-month overall survival was 93%. In conclusion, pembrolizumab was successfully administered as post-ASCT consolidation in patients with R/R DLBCL, but the PFS did not meet the protocol-specific primary objective and therefore does not support a larger confirmatory study. This trial was registered at www.clinicaltrials.gov as #NCT02362997.
Introduction
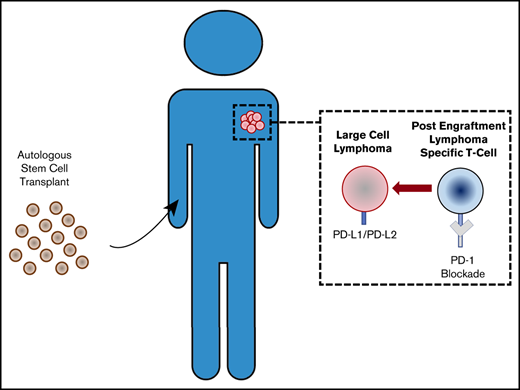
The leading cause of treatment failure after high-dose chemotherapy and autologous stem cell transplantation (ASCT) for patients with chemosensitive relapsed/refractory (R/R) diffuse large B-cell lymphoma (DLBCL) remains disease relapse. Although DLCBL, with the exception of primary mediastinal B-cell lymphoma (PMBCL), does not classically harbor genetic amplification at 9p24.1 leading to overexpression of PD1 ligands (PD-L1 and PD-L2), early results with PD-1 blockade in the R/R setting suggested a potential benefit across B-cell non-Hodgkin lymphoma subtypes, including a 36% overall response rate.1,2 Administering PD-1 blockade after ASCT is ideal for multiple reasons: (1) this setting is characterized by a minimal disease state; and (2) there exists a preponderance of lymphocytes after immune reconstitution that are the target for PD-1 blockade. PD-1 blockade early after ASCT could therefore leverage the remodeling immune landscape to decrease disease relapse. Because most relapses after ASCT occur within the first year following transplantation, maintenance with PD-1 blockade is likely to offer the most benefit during this early phase of immune reconstitution.3 Any benefits from such a strategy are likely to be durable, as previous studies using PD-1 blockade suggest that responses continue after discontinuation of drug treatment despite a half-life of only 14 to 22 days.4,5 We consequently conducted a phase 2 study administering maintenance anti–PD-1 antibody pembrolizumab after ASCT for patients with R/R DLBCL.
Methods
This phase 2, investigator-initiated, open-label, multicenter trial enrolled patients at 6 centers in the United States. The study accrued patients in 3 cohorts, 1 for classical Hodgkin lymphoma (cHL), 1 for DLBCL, and 1 for T-cell lymphoma. The current article presents the results of the DLBCL cohort. Patients aged ≥18 years with R/R DLBCL (per World Health Organization 2008 guidelines) or PMBCL who had received ≤3 lines of previous therapy and underwent ASCT who had chemosensitive disease (defined as partial response or better to salvage therapy, per International Harmonization Project criteria) were eligible.6,7 Patients could not have received previous anti–PD-1 therapy. Subjects who were enrolled before ASCT were required to re-screen and meet all eligibility criteria after transplantation. Treatment was started within 60 days of ASCT once participants had appropriate hematologic recovery (grade 2 or lower per Common Terminology Criteria for Adverse Events version 4.0) with a goal of starting pembrolizumab 200 mg intravenously every 3 weeks for 8 cycles within 21 days of hospital discharge. Dose modification was not allowed; however, subsequent dosing could be delayed up to 12 weeks for toxicity. Participants could not receive any additional therapy (including radiotherapy, chemotherapy, or immunotherapy) after ASCT. Drug was permanently held for grade 4 treatment-related adverse events (AEs) and selected grade 3 immune-related AEs. The primary endpoint was progression-free survival (PFS) at 18 months after ASCT, following the International Harmonization Project 2007 criteria using PET and CT scans.6
All patients signed informed consent. The study was registered at clinicaltrials.gov (NCT02362997), Institutional Review Board approved, monitored by an independent Data and Safety Monitoring Board, and conducted in accordance with the principles of the Declaration of Helsinki. Merck & Co. (Kenilworth, NJ) provided study drug and funding. Data collection and analysis were independently performed by investigators. PFS and overall survival rates were estimated as the proportion of evaluable patients alive and progression-free, or alive, respectively, at 18 months after ASCT. We hypothesized that pembrolizumab could improve the 18-month progression-free rate from 60% to 80%. Eighteen-month PFS 60% was determined based on previous studies of DLBCL after ASCT.8,9 With a sample size of 30 patients, the treatment would be considered promising if ≥22 of 30 patients remained progression free at 18 months. This design had a power of 87%, at a significance level of 0.09 as calculated by using the exact binomial method. We also calculated Kaplan-Meier estimates of PFS and overall survival; PFS was defined as time from transplantation to death from any cause, relapse, or progression, with patients censored at the last time seen alive and progression free, and overall survival was defined as the time from study entry to death from any cause, with patients censored at the last time seen alive.
When available, correlative studies were performed in patients who relapsed on or after treatment comparing pretransplantation and posttransplantation biopsy results. We specifically examined immune cell infiltrates, immune checkpoint, and major histocompatibility complex (MHC) expression via immunohistochemistry (IHC), a methodology previously reported.10
Results and discussion
Thirty-one subjects were enrolled, and two subjects withdrew consent before starting treatment. Clinical characteristics of the 29 eligible subjects are shown in Table 1. The median age was 57 years (range, 22-76 years). Eight patients were primary refractory to first-line therapy. Median International Prognostic Index and second-line age-adjusted International Prognostic Index for relapsed patients (n = 21) at time of salvage were 2 and 1, respectively. The median number of previous therapies before ASCT was 2, with R-ICE (rituximab-ifosfamide, carboplatin, etoposide) being the primary salvage regimen used. Before ASCT, 18 (62%) patients were in complete remission (CR), and 11 (38%) were in partial remission. At study baseline (post-ASCT), 25 (86%) patients were in CR. Eleven patients (38%) stopped pembrolizumab early due to the following: patient choice (n = 1), toxicity (n = 6), or progressive disease (n = 4). Twenty-three patients (79%) experienced a total of 57 grade 3 or higher AEs. Of the 6 patients who discontinued due to toxicity, 2 patients discontinued for grade 3 pneumonitis, 1 discontinued for grade 3 hepatitis, 1 discontinued for grade 4 aplastic anemia, 1 discontinued for grade 3 pneumonitis/rash/neutropenia, and 1 discontinued for febrile neutropenia. The most common grade 3 to 4 AE was neutropenia (n = 15 [26%]). Ten subjects (34%) experienced at least 1 immune-related AE of grade 2 or higher severity (15 total events) that included pneumonitis (n = 1, grade 2; n = 2, grade 3), transaminitis (n = 2, grade 2; n = 1, grade 3), and rash (n = 1, grade 2; n = 1, grade 3). Nine subjects (31%) experienced at least one grade 3 to 4 AE (14 total events) that was probably or definitely related to pembrolizumab, including neutropenia (four grade 3, one grade 4), leukopenia (two grade 3, one grade 4), and thrombocytopenia (one grade 3, one grade 4). Because hematologic recovery to grade 2 or lower was required before initiation of therapy, most subsequent hematologic toxicities were believed to be probably or definitely related to pembrolizumab therapy as determined by the treating investigator. There were no treatment-related deaths.
Baseline patient characteristics (N = 29)
| Variable . | Value . |
|---|---|
| Total | 29 (100) |
| Median age (range), y | 57 (22-76) |
| Histology | |
| DLBCL | 12 (41) |
| PMBCL | 5 (17) |
| TCR-BCL | 2 (7) |
| Transformed indolent NHL | 6 (21) |
| Relapsed after first-line therapy | 21 (72) |
| Relapse <12 mo (n = 21) | 11 (52) |
| Primary refractory to first-line therapy | 8 (28) |
| Baseline at relapse | |
| Median IPI (range) | 2 (1-3) |
| Median saaIPI (range) | 1 (0-2) |
| Median previous lines of therapy | 2 |
| Salvage regimens before ASCT | |
| R-ICE | 24 (84) |
| R-GDP | 2 (7) |
| DA-EPOCH-R | 1 (3) |
| R-HIDAC | 1 (3) |
| R-DHAP | 1 (3) |
| Conditioning regimen | |
| BEAM | 27 (93) |
| TBC | 2 (7) |
| Median time (range) from ASCT to first dose of pembrolizumab, d | 34 (28-57) |
| Disease status before ASCT | |
| Partial remission | 11 (38) |
| CR | 18 (62) |
| Disease status at study entry (post-ASCT) | |
| Partial remission | 4 (14) |
| CR | 25 (86) |
| Variable . | Value . |
|---|---|
| Total | 29 (100) |
| Median age (range), y | 57 (22-76) |
| Histology | |
| DLBCL | 12 (41) |
| PMBCL | 5 (17) |
| TCR-BCL | 2 (7) |
| Transformed indolent NHL | 6 (21) |
| Relapsed after first-line therapy | 21 (72) |
| Relapse <12 mo (n = 21) | 11 (52) |
| Primary refractory to first-line therapy | 8 (28) |
| Baseline at relapse | |
| Median IPI (range) | 2 (1-3) |
| Median saaIPI (range) | 1 (0-2) |
| Median previous lines of therapy | 2 |
| Salvage regimens before ASCT | |
| R-ICE | 24 (84) |
| R-GDP | 2 (7) |
| DA-EPOCH-R | 1 (3) |
| R-HIDAC | 1 (3) |
| R-DHAP | 1 (3) |
| Conditioning regimen | |
| BEAM | 27 (93) |
| TBC | 2 (7) |
| Median time (range) from ASCT to first dose of pembrolizumab, d | 34 (28-57) |
| Disease status before ASCT | |
| Partial remission | 11 (38) |
| CR | 18 (62) |
| Disease status at study entry (post-ASCT) | |
| Partial remission | 4 (14) |
| CR | 25 (86) |
Values are n (%) unless otherwise noted.
BEAM, carmustine, etoposide, cytarabine, melphalan; DA-EPOCH, dose-adjusted, etoposide, prednisone, vincristine, cyclophosphamide, hydroxydaunorubicin; DHAP, dexamethasone, high-dose cytarabine, cisplatin; GDP, gemcitabine, dexamethasone, cisplatin; HIDAC, high-dose cytarabine; ICE, ifosfamide, carboplatin, etoposide; IPI, International Prognostic Index; NHL, non-Hodgkin lymphoma; R, rituximab; saaIPI, second-line age-adjusted International Prognostic Index; TBC, thiotepa, busulfan, cyclophosphamide; TCR-BCL, T-cell–rich B-cell lymphoma.
Among the 29 eligible subjects, 1 patient withdrew consent after cycle 1 and 1 was lost to follow-up after the 12-month assessment (CR). Twenty-seven patients (93%) were evaluable for the primary endpoint (Figure 1A-B). Ten patients (34%; 95% CI, 18-54) experienced relapse at a median of 5 months (range, 3-18 months), and all other evaluable patients (n = 17; 59% [95% CI, 39-76]) were in CR at the 18-month time point. Only 1 of 7 PMBCL or T-cell–rich B-cell lymphoma patients relapsed at the 18-month time point. Kaplan-Meier estimate of PFS at 18.5 months (chosen to account for variability of restaging timing) was 58% (95% CI, 34-76). In a prespecified comparison, the 18.5-month PFS for the 11 patients in partial remission before ASCT was 0% vs 87% (95% CI, 57-97) for those in CR (P = .0003). Two subjects died of disease relapse within 3 months of ASCT.
PFS, overall survival, and examples of tumor characteristics pre- and posttreatment. PFS in all evaluable patients (n = 29) (A) and patients stratified according to disease response before ASCT (partial remission [PR], n = 11; CR, n = 18) (B). (C) Representative IHC for pretransplant (pre) samples and posttransplant (post) relapse biopsy samples (original magnification ×200) showing CD3 (white), PD-1 (red), and 4′,6-diamidino-2-phenylindole (DAPI; blue) with corresponding quantification of CD3+ infiltrates and PD-1 staining in 4 patients. (D) Representative IHC for pretransplant samples and posttransplant relapse biopsy samples (original magnification ×200) showing Pax5 (pink), CD68 (orange), PD-L1 (green), and DAPI (blue) with corresponding quantification of CD68+PD-L1+ infiltrates in 4 patients.
PFS, overall survival, and examples of tumor characteristics pre- and posttreatment. PFS in all evaluable patients (n = 29) (A) and patients stratified according to disease response before ASCT (partial remission [PR], n = 11; CR, n = 18) (B). (C) Representative IHC for pretransplant (pre) samples and posttransplant (post) relapse biopsy samples (original magnification ×200) showing CD3 (white), PD-1 (red), and 4′,6-diamidino-2-phenylindole (DAPI; blue) with corresponding quantification of CD3+ infiltrates and PD-1 staining in 4 patients. (D) Representative IHC for pretransplant samples and posttransplant relapse biopsy samples (original magnification ×200) showing Pax5 (pink), CD68 (orange), PD-L1 (green), and DAPI (blue) with corresponding quantification of CD68+PD-L1+ infiltrates in 4 patients.
Overall, therefore, the study did not meet its primary endpoint. A previous phase 2 study tested the monoclonal antibody pidilizumab, which was believed to bind PD-1, as post-ASCT consolidation for DLBCL; this study met its prespecified efficacy endpoint, suggesting the potential value of this strategy.11 However, the specificity of pidilizumab has recently been reconsidered, with more recent evidence suggesting that its target is delta-like protein 1 and not PD-1.12 In addition, a phase 2 study of nivolumab, which was not available at the inception of the current trial, showed that PD-1 blockade has, in fact, very limited activity in unselected DLBCL.13 Our results suggest that deploying PD-1 blockade post-ASCT does not seem to increase its therapeutic benefit in this disease.
Pretreatment (from diagnosis or relapse) and postprogression biopsy samples were available for 4 patients whose disease progressed during the study. Although most postprogression biopsy results demonstrated lower CD3+ T-cell infiltrates compared with pretreatment ones, according to both density and percentage of total cellularity, PD-1 expression on the remaining CD3+ cells was roughly unchanged (Figure 1C). PD-L1 expression was observed predominantly on CD68+ macrophages and did not significantly differ between time points (Figure 1D), a finding previously described in the de novo setting without significant prognostic implication.14,15 To investigate alternative mechanisms of resistance, samples were also analyzed for MHC class II expression, as well as its ligand LAG3. The relative expression of MHC class II on PAX5+ tumor cells was increased in postprogression samples (P = .04) (supplemental Figure 1). There was no corresponding increase in LAG3 expression on infiltrating T cells (supplemental Figure 2). These results argue that relapse in this context may not be related to alteration in expression of PD-1 or PD-L1. It is possible that LAG-3/MHC II–mediated inhibition could participate in the mechanism of relapse; however, full elucidation of those mechanisms will definitely require further studies.
In conclusion, pembrolizumab after ASCT in patients with R/R DLBCL is feasible, with potentially higher hematologic toxicity compared with the recently reported cHL arm of this trial.10 These differences are likely attributable to differences in previous treatment regimens when comparing disease subtypes. Alternatively, it could reflect an accentuated toxicity of pembrolizumab in this specific context, although the rate of severe neutropenia was lower in the cHL arm of the trial, arguing against a general post-ASCT immuno-oncology phenomenon. The 18-month PFS rate did not meet the protocol-specified primary objective and therefore does not support a larger confirmatory study in R/R DLBCL. Future studies of PD-1 blockade in the post-ASCT setting should likely focus on specific subsets of DLBCL (eg, PMBCL,16 Epstein-Barr virus–positive DLBCL,17,18 T-cell histiocyte-rich large cell lymphoma18 ), which may be especially sensitive to PD-1 blockade.
Acknowledgments
The authors are indebted to the nursing and research staff who were involved in this study, and to all the participants and their families.
The study was funded by Merck & Co. P.A. gratefully acknowledges the support of the Leukemia and Lymphoma Society (Scholar in Clinical Research), as well as the Harold and Virginia Lash Foundation and the Pasquarello Tissue Bank in Hematologic Malignancies. A.F.H. was supported by the Lymphoma Research Foundation Larry and Denise Mason Clinical Investigator Career Development Award and the National Cancer Institute of the National Institutes of Health (NIH) (2K12CA001727 and P50CA107399). M.J.F. was supported by the NIH/National Cancer Institute (K12CA087723).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Authorship
Contribution: M.J.F. collected data, analyzed and interpreted data, and wrote the manuscript; P.A., Y.-B.C., and R.M.J. designed research, performed research, collected data, analyzed/interpreted data, performed statistical analysis, and helped in manuscript preparation; and R.A.R., E.J., R.W.M., K.C.C., A.F.H., P.D., Y.N., A.S.L., D.C.F., S.Y.N., O.O.O., A.S.F., A.I.K., J.L.C., C.A.J., E.D.J., J.L.W., J.B., S.S.P., J.R., S.J.R., and M.A.S. performed research, analyzed data, and helped in manuscript preparation.
Conflict-of-interest disclosure: M.J.F. has served as a consultant for Novartis, Xenetic, Foundation Medicine, Arcellx, Nkarta, Incyte, and June/Celgene; and received honoraria from Kite/Gilead. P.A. has served as a consultant for Merck, Bristol-Myers Squibb, Pfizer, Affimed, Adaptive, Infinity, ADC Therapeutics, Celgene, and MorphoSys; received research funding (institution) from Merck, Bristol-Myers Squibb, Affimed, Adaptive, Roche, Tensha, Otsuka, Sigma-Tau, Genentech, and IGM; and has received honoraria from Bristol-Myers Squibb and Merck. A.F.H. has served as a consultant for Bristol-Myers Squibb, Genentech, Merck & Co., Kite Pharma/Gilead, Adaptive Biotechnologies, and Seattle Genetics; and has received research funding from Bristol-Myers Squibb, Genentech, Immune Design, AstraZeneca, Merck & Co., Pharmacyclics, Seattle Genetics, Kite Pharma, and Gilead Sciences. Y.N. has received research funding from Otsuka, AstraZeneca, Affimed, Celgene, Sanofi Aventis, and Novartis. A.S.L. has served as a consultant for Bristol-Myers Squibb; and has received honoraria/speakers bureau fees from Seattle Genetics, Humanigen, and Research to Practice. C.A.J. has served as a consultant for Kite, Novartis, Pfizer, Humanigen, Precision Bioscience, Bayer, and Celgene; and has received research funding from Pfizer and Kite. E.D.J. has served as a consultant for Merck, AstraZeneca, and Seattle Genetics; and received research funding from Pharmacyclics and Celgene. J.R. has served as a consultant for Avrobio, Celgene, Draper Labs, Falcon Therapeutics, LifeVault Bio, Talaris Therapeutics, and TScan Therapeutics; and has received research funding from Equillium and Kite Pharma. S.J.R. has received research funding from Bristol-Myers Squibb, Merck, Kite/Gilead, and Affimed Pharmaceuticals. M.A.S. has served as a consultant for Bristol-Myers Squibb; and has received research funding from Bayer, Bristol-Myers Squibb, and Merck. Y.-B.C. has served as a consultant for Magenta, Takeda, Kiadis, Incyte, and AbbVie. The remaining authors declare no competing financial interests.
Correspondence: Philippe Armand, Dana-Farber Cancer Institute, 450 Brookline Ave, Boston, MA 02215; e-mail: philippe_armand@dfci.harvard.edu.
References
Author notes
The full-text version of this article contains a data supplement.
M.J.F. and P.A. contributed equally to this work.
Y.-B.C. and R.M.J. contributed equally to this work.
All available data can be obtained by contacting the corresponding author (Philippe Armand; e-mail: philippe_armand@dfci.harvard.edu).

![PFS, overall survival, and examples of tumor characteristics pre- and posttreatment. PFS in all evaluable patients (n = 29) (A) and patients stratified according to disease response before ASCT (partial remission [PR], n = 11; CR, n = 18) (B). (C) Representative IHC for pretransplant (pre) samples and posttransplant (post) relapse biopsy samples (original magnification ×200) showing CD3 (white), PD-1 (red), and 4′,6-diamidino-2-phenylindole (DAPI; blue) with corresponding quantification of CD3+ infiltrates and PD-1 staining in 4 patients. (D) Representative IHC for pretransplant samples and posttransplant relapse biopsy samples (original magnification ×200) showing Pax5 (pink), CD68 (orange), PD-L1 (green), and DAPI (blue) with corresponding quantification of CD68+PD-L1+ infiltrates in 4 patients.](https://ash.silverchair-cdn.com/ash/content_public/journal/bloodadvances/4/1/10.1182_bloodadvances.2019000784/5/m_advancesadv2019000784f1.png?Expires=1769085004&Signature=FSa0S36YzXlWFPHr1dcUgo9fdWQ5TOlfKPzeLxcq7ne0HXgwIT1g7o~BXL469b3WdeCt3R6Kdck~qglhS8dhFrl4~3BO76vSBljNB6cmtnueCC8fHsZAh-OwNbX0spGsNzM1BHt5zq8bQhrTqli1ZQ0SO1nB6qYFYqCcG0inH3CbDln2nS3NMGiP1xTe-9CpUGSWjy2Ll8HS5UxPUma2f-sAMFFWDQWmDE2~34piYQ--lunpcjoNM4apbVgZsbAxJwDyQP1SI79XLmCmKJQMdxkmYGSluJioIasMJDDakXjuCL2cAs6Oh7il4b-bY53z3wusoW5a47hyBSP3naMUNA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)