Key Points
Infusion of exa-cel in patients with severe SCD improved overall HRQoL.
Clinically meaningful improvements in HRQoL and reduction in pain were observed in both adults and adolescents across health domains.
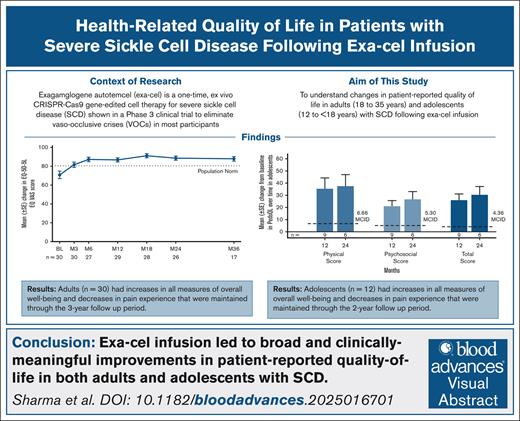
Visual Abstract
Severe sickle cell disease (SCD), an inherited blood disorder characterized by recurrent vaso-occlusive crises (VOCs), significantly impairs health-related quality of life (HRQoL). Exagamglogene autotemcel (exa-cel), a one-time, ex vivo CRISPR/Cas9 gene-edited cell therapy, eliminated VOCs in 97% of participants with severe SCD in the phase 3 CLIMB SCD-121 trial. Here, we describe changes in patient-reported outcomes (PROs) in 30 adults and 12 adolescents with ≥16 months follow-up. Adult PROs include EuroQol Quality of Life Scale–5 dimensions–5 levels of severity (EQ-5D-5L), Functional Assessment of Cancer Therapy Bone Marrow Transplant (FACT-BMT), Adult Sickle Cell Quality of Life Measurement Information System (ASCQ-Me), and 11-point pain Numerical Rating Scale (NRS). In adolescents, EuroQol Quality of Life Scale–5 dimensions–youth (EQ-5D-Y), Pediatric Quality of Life Inventory (PedsQL), and pain NRS were used. Adult EQ-5D-5L US and UK healthy utility index and EQ visual analog scale (VAS) scores, which were lower than general population norm at baseline, substantially improved by month 6 after exa-cel infusion and were sustained through month 36, with similar improvements in FACT-General (FACT-G) total and bone marrow transplant subscale. All FACT-G (physical, social/family, emotional, functional well-being) and ASCQ-Me (emotional, social functioning, stiffness, sleep impact) subscales showed clinically meaningful improvement, including ASCQ-Me pain subscales (impact, episode frequency, severity), with substantial decreases in pain episode frequency by month 6. Mean pain NRS score decreased by month 6 and was sustained. Consistent with adults, adolescents had improvements in mean EQ-5D-Y VAS score, PedsQL score, and pain NRS. Exa-cel led to broad and clinically meaningful HRQoL benefits in adults and adolescents with SCD. The CLIMB SCD-121 and CLIMB-131 trials were registered at www.clinicaltrials.gov as #NCT03745287 and #NCT04208529, respectively.
Introduction
Sickle cell disease (SCD) is an inherited disorder caused by a single point mutation in the gene that encodes the β-subunit of adult hemoglobin (HBB), leading to the production of abnormal hemoglobin and sickled red blood cells.1,2 SCD can also occur in individuals who coinherit the sickle cell mutation in conjunction with an additional β-globin gene mutation.1 Clinically, SCD is characterized by acute and life-long complications, including recurrent vaso-occlusive crises (VOCs), avascular necrosis, and chronic hemolytic anemia, which can lead to end-organ damage and early mortality.1-4 Individuals with SCD have impaired health-related quality of life (HRQoL) due to the debilitating pain associated with VOCs, as well as other acute and chronic complications, which affect school achievement and/or ability to work, and increase the prevalence of depression and anxiety.5,6
For people with severe SCD, treatment options are limited and consist of therapies that aim to reduce disease severity. Allogeneic hematopoietic stem cell transplantation (HSCT) is a potentially curative therapy for patients with SCD7; however, the limitation of available HLA-matched donors and the potential risk of graft failure, graft-versus-host disease, and other immunologic side effects has limited the more widespread use of this treatment option.8-10 Exagamglogene autotemcel (exa-cel) is a cell therapy that is designed to reactivate the synthesis of fetal hemoglobin (HbF) via nonviral, ex vivo CRISPR/Cas9 gene-editing of autologous CD34+ hematopoietic stem and progenitor cells (HSPCs) at the erythroid-specific enhancer region of the BCL11A gene.11 Elevated levels of HbF, observed in people with hereditary persistence of HbF, are associated with reductions in clinical complications, morbidity, and mortality in patients with SCD.12 In a prespecified interim analysis of the pivotal phase 3 CLIMB SCD-121 trial, a single infusion of exa-cel increased mean HbF levels to >40%, eliminating severe VOCs in 97% of participants (primary end point) and hospitalizations due to severe VOCs in 100% of participants (key secondary end point) for a period of ≥12 months and having a safety profile consistent with a myeloablative, busulfan-based conditioning regimen and autologous HSCT.13 These results suggest that exa-cel also has the potential to be a curative option for people with severe SCD. Participants who completed the CLIMB SCD-121 trial were offered the opportunity to enroll in the 13-year extension study, CLIMB-131.
The impact of exa-cel on quality of life using patient-reported outcome (PRO) measures was a secondary objective of the CLIMB SCD-121 and CLIMB-131 trials. PRO measures evaluate HRQoL in patients, providing information on the physical, social, and emotional well-being and insights into the impact of clinical treatments on patient experience, including disease-specific impacts. In the prespecified interim analysis of CLIMB SCD-121, adults with ≥16 months of follow-up after exa-cel infusion had robust improvements in PRO measures at month 24, including improvements in pain, health status, and general well-being indicative of an overall improved quality of life.13 Here, we report changes in PRO measures assessing general well-being, HSCT experience, and SCD-specific HRQoL for up to 3 years in adults and up to 2 years in adolescents with SCD following the infusion of exa-cel in the CLIMB SCD-121 clinical trial and the CLIMB-131 long-term extension study.
Methods
Study design and patients
CLIMB SCD-121 is an ongoing, 24-month, phase 3 trial of a single dose of exa-cel in participants aged 12 to 35 years with severe SCD (defined as a history of ≥2 severe VOCs per year in the previous 2 years). Participants received plerixafor for HSPC mobilization followed by apheresis to collect CD34+ cells for gene editing. Before infusion, all participants received myeloablative conditioning with pharmacokinetically adjusted busulfan. Exa-cel was administered IV at least 48 hours, but no more than 7 days, after conditioning. Further details on the exa-cel infusion procedure can be found in a previously published report by Frangoul et al.13 Participants who completed the 2-year study period in CLIMB SCD-121 were offered the opportunity to enroll in the 13-year follow-up extension study, CLIMB-131.
The primary end point of the CLIMB SCD-121 trial was the proportion of participants free of severe VOCs for ≥12 consecutive months (VF12). The key secondary end point was the proportion of participants free from in-patient hospitalization for severe VOCs for ≥12 consecutive months (HF12). Other secondary end points included changes from baseline in total hemoglobin and HbF, duration of time free of VOCs, and changes from the baseline PRO measures in adults and adolescents.
The CLIMB SCD-121 and CLIMB-131 clinical trials were designed by Vertex Pharmaceuticals Incorporated and CRISPR Therapeutics in collaboration with a steering committee. Each participant or legal guardian provided written informed consent, and an independent data monitoring committee monitored safety. Study protocols were approved by the institutional review board at each participating institution. Data collection and analyses were conducted by Vertex Pharmaceuticals Incorporated in collaboration with the authors. Trials were conducted in accordance with the Declaration of Helsinki, local applicable laws and regulations, and the current Good Clinical Practice Guidelines described by the International Council for Harmonization.
Data collection and patient-reported QoL assessments
PRO measures assessed in the CLIMB SCD-121 and CLIMB-131 trials include the validated generic and disease-specific measures, such as EuroQoL Quality of Life Scale–5 dimensions–5 levels of severity (EQ-5D-5L; health utility index scores derived country-specific value sets for the United States and United Kingdom); Functional Assessment of Cancer Therapy Bone Marrow Transplant (FACT-BMT, FACT-General [FACT-G], and bone marrow transplant subscale [BMTS]); 11-point pain Numerical Rating Scale (NRS); and Adult Sickle Cell Quality of Life Measurement Information System (ASCQ-Me) for adults, along with EuroQol Quality of Life Scale–5 dimensions–youth (EQ-5D-Y), Pediatric Quality of Life Inventory (PedsQL), and PedsQL SCD module, and pain NRS for adolescents. A description of these PRO measures is provided in supplemental Table 1.
Statistical analysis
The analyses of the PRO measurements used descriptive statistics (eg, mean, standard error, and standard deviation [SD]) and no hypothesis testing was performed at any stage after collection of these data. All plots used mean and standard error to show the precision of sample mean, whereas mean and SDs were used for all plot time points provided in the online supplemental. Change from baseline, defined as the most recent nonmissing measurement (namely, latest time point with a valid measurement not considered to be null) obtained before the start of HSPC mobilization and collection before exa-cel infusion, was determined for the total and domain scores of PRO measures at each postbaseline time point using all available data at the time of analysis. To determine the minimal clinically important differences (MCIDs) for PRO measures, literature searches were conducted. MCIDs were identified based on literature using anchor- and/or distribution-based methods.14 MCIDs were estimated to be 7 to 10 points for EQ-5D-5L visual analog scale (VAS) and 0.078 and 0.08 points for the US and UK index scores, respectively15,16; 3 to 7 points for FACT-G17; 2 to 3 points for BMTS18; and a 1-point reduction or 30% reduction for pain NRS.19 For the ASCQ-Me scales, scores were transformed into T-scores (0-100), with 1 SD of 10 points and a change of 5 points (1/2 SD) representing the MCID. MCIDs for the PedsQL domain score ranged from 4.36 to 9.12 points.20 Data cuts are conducted throughout both studies to allow for study review by the independent data monitoring committee.
Results
Participant demographics and baseline clinical characteristics
As of August 2024, 46 participants with SCD had received exa-cel, 42 of whom had ≥16 months of follow-up after infusion and were therefore included in the analyses of PRO measures at the time of the data cut (defined hereafter as the primary efficacy set). The mean historical number of VOCs per year in the 2-year period before screening for these participants was 4.2 (SD, 3.1) and the mean number of annual in-patient hospitalizations for VOCs was 2.8 (SD, 2.1) (Table 1). Of the 42 participants in the primary efficacy set, 30 were adults aged ≥18 years and 12 were adolescents aged ≥12 years and <18 years, all of whom were included in analyses of PROs (Table 1).
At time of the data cut, the median duration of follow-up was 33.6 months (range, 17.2-62.2). For the analysis of PRO measures, we report follow-up data for up to 36 months for adults and up to 24 months for adolescents. A total of 34 of the 42 participants in the primary efficacy set completed the 24-month CLIMB SCD-121 trial and were enrolled in the CLIMB-131 extension study.
PRO assessments in adults in primary efficacy set
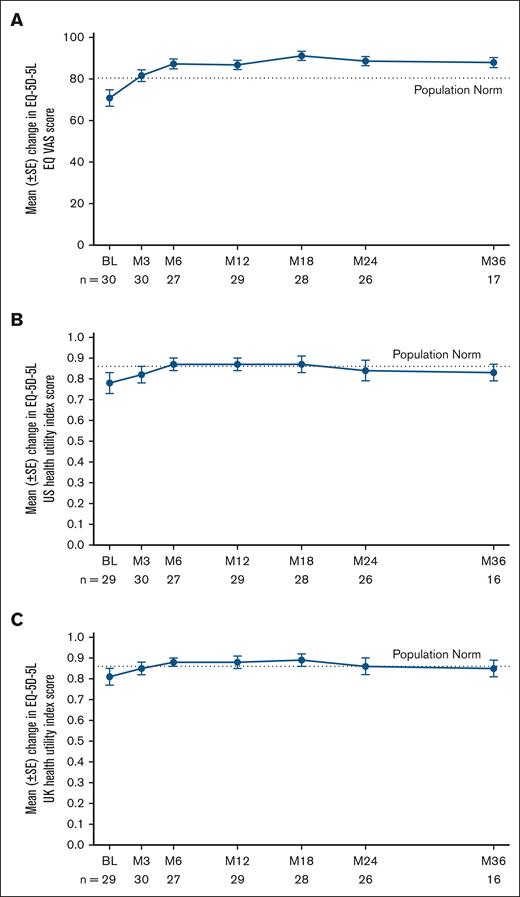
Evaluation of the measures of general well-being and quality of life included EQ VAS and EQ-5D-5L. For the adults in the primary efficacy set, the mean EQ VAS and EQ-5D-5L health utility US and UK index scores at baseline were lower than those of the general population norms and consistent with the baseline scores reported for adults with SCD who have recurrent VOCs (Figure 1), indicating significant impairment in overall health status. By month 6 after exa-cel infusion, substantial improvements exceeding the MCID were observed in the mean EQ VAS score (mean [SD] change from baseline, 17.7 points [26.5]; MCID, 7-10; n = 27) (Figure 1A, supplemental Figure 2A, supplemental Table 2). Similarly, the EQ-5D-5L health utility US index score (mean [SD] change from baseline 0.10 points [0.20], MCID 0.078; n = 27) and EQ-5D-5L health utility UK index score (0.07 [0.17], MCID 0.08; n = 27) also showed substantial improvements by month 6 (Figure 1B-C, supplemental Figure 2B-C, supplemental Table 2). Overall, the 3 measures were at or above general population norms by month 6 and were generally maintained through month 36 (Figure 1).
Changes in EQ-5D-5L EQ VAS and EQ-5D-5L US and UK index scores in adults in the primary efficacy set after exa-cel infusion. (A) Mean EQ-5D-5L EQ VAS score by study visit. (B) Mean EQ-5D-5L US health utility index score by study visit. (C) Mean EQ-5D-5L UK health utility index score by study visit. Dashed lines depict the established population norms for each measure. Error bars indicate the standard error of the mean. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. BL, baseline; M, month; SE, standard error.
Changes in EQ-5D-5L EQ VAS and EQ-5D-5L US and UK index scores in adults in the primary efficacy set after exa-cel infusion. (A) Mean EQ-5D-5L EQ VAS score by study visit. (B) Mean EQ-5D-5L US health utility index score by study visit. (C) Mean EQ-5D-5L UK health utility index score by study visit. Dashed lines depict the established population norms for each measure. Error bars indicate the standard error of the mean. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. BL, baseline; M, month; SE, standard error.
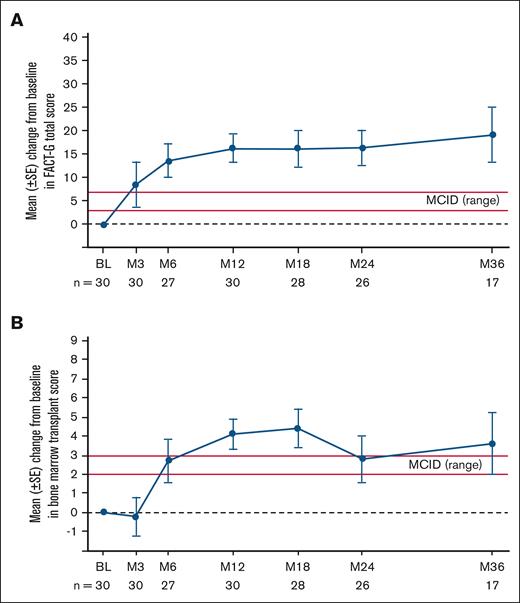
The assessment of HSCT-related impact used FACT-BMT, which includes a general well-being and quality of life component (FACT-G) and an HSCT specific component (BMTS). The mean FACT-G score showed substantial improvement by month 6 (mean [SD] change from baseline, 13.7 points [18.9]; MCID, 3-7; n = 27) and was sustained through month 36 (mean [SD] change from baseline 19.2 [24.1]; n = 17) (Figure 2A, supplemental Figure 3A, supplemental Table 3). Critically, improvements exceeded MCIDs across all 4 FACT-G subscales (physical, social/family, emotional, and functional well-being) (supplemental Table 4). Improvements in fatigue were also observed, with fewer adults reporting that they lacked energy following exa-cel infusion (supplemental Figure 1A). Consistent with these broad improvements in FACT-G scores, mean BMTS score (a measure of transplant-related well-being) showed clinically meaningful improvement by month 6 (mean [SD] change from baseline, 2.7 points [5.9]; MCID, 2-3; n = 27) and was then sustained through month 36 (mean [SD] change from baseline, 3.6 [6.7]; n = 17) (Figure 2B, supplemental Figure 3B, supplemental Table 3).
Changes in FACT-G total and BMTS scores in adults in the primary efficacy set after exa-cel infusion. (A) Mean change from baseline by study visit in FACT-G total score. (B) Mean change from baseline by study visit in BMTS. Red lines in figures depict the established MCID range. Error bars indicate the standard error of the mean. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. BL, baseline; M, month; SE, standard error.
Changes in FACT-G total and BMTS scores in adults in the primary efficacy set after exa-cel infusion. (A) Mean change from baseline by study visit in FACT-G total score. (B) Mean change from baseline by study visit in BMTS. Red lines in figures depict the established MCID range. Error bars indicate the standard error of the mean. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. BL, baseline; M, month; SE, standard error.
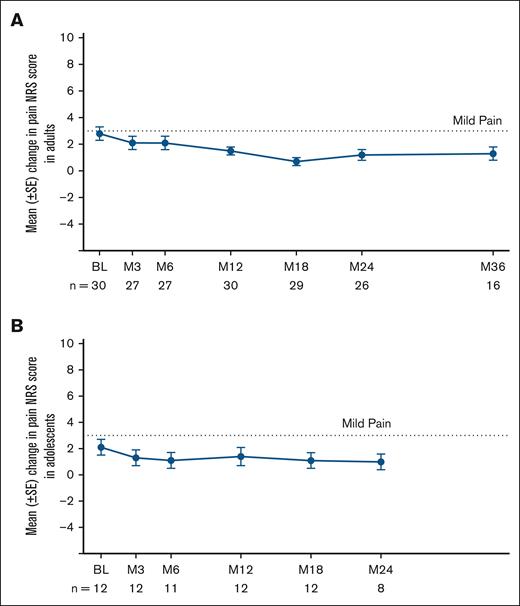
The PRO tool ASCQ-Me is an SCD-specific instrument that assesses multiple domains of HRQoL in adults with SCD. At month 6, several domains of ASCQ-Me showed substantial improvement exceeding MCID. At month 36, all domains of the ASCQ-Me, including pain impact (mean [SD] change from baseline, 8.1 points [7.9]), emotional impact (8.5 [7.8]), social functioning impact (16.5 [9.8]), stiffness impact (5.1 [10.9]), and sleep impact (5.7 [8.3]) (MCID = 5 points for all these domains), as well as the pain episode domains of pain episode frequency (–21.0 [8.0]) and pain episode severity (–5.1 [14.3]) (MCID = –5 points for pain episode domains) showed clinically meaningful improvement that exceeded MCID (Figure 3, supplemental Figure 4, supplemental Table 5). Further supporting reductions in pain following exa-cel infusion, the mean pain NRS score, a scale used to measure pain, improved by month 6 (mean [SD] change from baseline, –0.9 points [3.3]; MCID, –1; n = 27) and was then sustained through month 36 (–1.8 [2.1]; n = 16) (Figure 4A, supplemental Figure 5A, supplemental Table 6).
Changes in ASCQ-Me scores from baseline in adults in the primary efficacy set after exa-cel infusion. Dotted lines indicate the MCIDs for each measure. I-bars indicate standard error. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. SE, standard error.
Changes in ASCQ-Me scores from baseline in adults in the primary efficacy set after exa-cel infusion. Dotted lines indicate the MCIDs for each measure. I-bars indicate standard error. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. SE, standard error.
Change in pain NRS scores in adults and adolescents in the primary efficacy set after exa-cel infusion. (A) Mean adult pain NRS score by study visit. (B) Mean adolescent pain NRS score by study visit. Dotted lines indicate the measure for mild pain (3 points). Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. BL, baseline; M, month; SE, standard error.
Change in pain NRS scores in adults and adolescents in the primary efficacy set after exa-cel infusion. (A) Mean adult pain NRS score by study visit. (B) Mean adolescent pain NRS score by study visit. Dotted lines indicate the measure for mild pain (3 points). Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. BL, baseline; M, month; SE, standard error.
PRO assessments in adolescents in primary efficacy set
Consistent with the improvements in overall health status observed in the adults, adolescents who received exa-cel had improvement in overall general well-being with EQ-5D-Y VAS and EQ-5D-Y US index scores increasing by month 6 (mean [SD] change from baseline at month 6, 4.1 points [34.9], and 0.10 [0.30], respectively; n = 11) that were sustained through month 24 (mean [SD] change from baseline at month 24, 10.7 [24.4] and 0.14 [0.26], respectively; n = 7) (Table 2). Robust improvements in mean PedsQL total score, a measure of HRQoL in children or adolescents with chronic diseases, were seen by month 6 (mean [SD] change from baseline 23.0 points [18.2], MCID 4.36; n = 11) and were maintained through month 24 (30.4 [16.8]; n = 6), with improvements seen across all subcomponents and subscales of the PedsQL (ie, physical health and psychosocial health, including social, emotional, and school functioning) (Figure 5, supplemental Figure 6, supplemental Tables 7 and 8). Similar to adults, fewer adolescents reported having low energy following exa-cel infusion (supplemental Figure 1B). SCD-specific HRQoL improvements were observed with the PedsQL SCD module, with improvements that exceeded MCID (supplemental Table 9). Consistent with this, mean Pain NRS score improved by month 6 (mean [SD] change from baseline −1.1 points [2.1], n = 11) and was maintained through month 24 (−0.9 [0.6], n = 8) (Figure 4B, supplemental Figure 5B, supplemental Table 10).
Changes in PedsQL scores from baseline in adolescents in the primary efficacy set after exa-cel infusion. (A) Change from baseline in PedsQL physical, psychosocial, and total scores at month 12 and month 24 after exa-cel infusion. (B) Change from baseline in PedsQL psychosocial domain emotional, social, and school functioning subscores at month 12 and month 24 after exa-cel infusion. Dotted lines indicate the MCIDs for each measure. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. SE, standard error.
Changes in PedsQL scores from baseline in adolescents in the primary efficacy set after exa-cel infusion. (A) Change from baseline in PedsQL physical, psychosocial, and total scores at month 12 and month 24 after exa-cel infusion. (B) Change from baseline in PedsQL psychosocial domain emotional, social, and school functioning subscores at month 12 and month 24 after exa-cel infusion. Dotted lines indicate the MCIDs for each measure. Baseline is defined as the most recent nonmissing measurement (scheduled or unscheduled) collected before the start of mobilization. SE, standard error.
Discussion
In a pivotal phase 3 clinical trial, exa-cel was shown to increase HbF levels in participants with SCD, leading to elimination of VOCs in >95% of patients.13 To understand the impact of this change in SCD disease trajectory on quality of life, PRO measures were assessed as a secondary end point in the exa-cel clinical trials. Following exa-cel infusion, there were clinically meaningful improvements in all PRO measures assessed in both adult and adolescent participants, including improvements in overall health and general well-being, as well as specific improvements in physical, emotional, social functioning well-being, and pain experience. All pain measures indicated participants had reductions in pain and frequency of pain events following exa-cel infusion. Taken together, these results, which represent the largest PRO data set for patients with SCD following HSCT or gene therapy, show exa-cel infusion leads to clinically meaningful improvements in quality of life in patients with severe SCD.
Adults and adolescents in the CLIMB SCD-121 clinical trial had severe SCD, as reflected by the inclusion criteria that specified a history of ≥2 VOCs per year in each of the 2 years before screening. The severity of SCD disease in these participants can also be observed in the impairments to their overall quality of life and health status as reflected in the baseline EQ-5D scores, which were below population norms. The low HRQoL reported by participants in this trial was consistent with the observed disease burden and the frequency of VOCs before baseline and in line with values reported in literature for patients with SCD who have recurrent VOCs. Following the infusion of exa-cel, substantial and clinically meaningful improvements in health-related quality of life measures were observed as early as month 6, with mean scores at or above the population norm (indicating quality of life had been normalized), which were then maintained throughout the follow-up period. Although a population norm value and an MCID are not available for adolescents, a similar improving trend in both EQ-5D-Y VAS and EQ-5D-Y US index score was observed.
To elucidate the impact of exa-cel treatment on specific aspects of health status in people with severe SCD, adults were given the FACT-BMT and ASCQ-Me assessments and adolescents the PedsQL (including the SCD module) assessment. Consistent with an improved overall health status, FACT-G total score also substantially improved by month 6 after exa-cel, exceeding the MCID and the population norm, and was sustained through month 36. FACT-G subscales showed that all four domains (including physical, social/family, emotional, and functional well-being) improved, suggesting that exa-cel has a broad impact on HRQoL. As the participants had to undergo myeloablation, the substantial improvement observed in mean BMTS score suggests improved well-being following infusion of edited cells. The early clinically meaningful improvements by month 6 also reflect the profile of the autologous HSCT using single agent busulfan for myeloablative conditioning prior to exa-cel, in which the majority of adverse events occur in the first 6 months post-HSCT.13 This is unlike allogeneic HSCT, in which HRQoL improvements take longer (≥1 year) to be consistently observed.21
The results for adolescents showed a similar improvement in HRQoL. Mean total PedsQL score, which measures self-reported health status in adolescents aged 12 to 17 years,22 along with all subcomponents of the PedsQL, improved early after exa-cel infusion and were maintained throughout the follow-up period. Before exa-cel infusion, adolescents had mean values for the psychosocial domains of the PedsQL (ie, school functioning, social, and emotional) below the population norm. Following exa-cel infusion, substantial improvements from baseline (often multifold greater than the MCID) were seen in school functioning score (mean increase of 45.0 at month 24), social score (+18.3), and emotional score (+16.7), resulting in mean scores higher than populations norms for these measures. Consistent with psychosocial scores, the mean baseline physical score was also below population norm (54.8), but it was at population norm by month 24 (85.9). The increase in mean physical score to near population norms following exa-cel infusion differs from the findings in patients who have undergone allogeneic HSCT, where physical function was noted to be depressed in many post-HSCT patients and physical function/mobility scores remained below population norms,23,24 suggesting potential differences in the impact of these treatments on patient physical function/mobility. Taken together, these results demonstrate that the quality of life improvements noted in adults and adolescents following exa-cel infusion are broad, affecting physical activity as well as psychosocial health.
Although FACT-BMT and PedsQL are general PRO instruments that assess HRQoL, the ASCQ-Me and PedsQL SCD module are SCD-specific tools. Consistent with the general EQ-5D-5L and FACT-BMT instruments, all domains of the ASCQ-Me showed improvements in adults throughout the follow-up period. The largest changes in the nonpain domains of the ASCQ-Me were social impact (+16.5), emotional impact (+8.5), sleep impact (+5.7), and stiffness impact (+5.1). For the pain-specific domains of the ASCQ-Me, pain episode frequency substantially declined (a reduction of 21.0 points), whereas a smaller decline was observed in pain episode severity (a reduction of 5.1 points). The pain episode frequency domain asks the participant to provide the number of SCD pain crises that they had experienced in the past 12 months, whereas the pain episode severity domain asks specifically about the last pain crises experienced. Given that the majority of participants in the CLIMB SCD-121 trial were free from VOCs following exa-cel infusion, the substantial decline in the pain episode frequency domain is expected. By contrast, the decline in pain episode severity domain, while also pointing to a reduced pain experience for participants, should be interpreted with caution because in many instances, the last pain episode was experienced before exa-cel infusion, which in most participants was over 1 year earlier.13 Interestingly, changes in pain experience following exa-cel infusion were even more notable in adolescents, which might be due to generally less severe or overt chronic end-organ damage, including chronic pain syndromes and vascular necrosis. All pain domains assessed in the PedsQL SCD module (eg, pain and hurt, pain impact, and pain management) showed substantial and clinically meaningful improvement by month 6 and were sustained through the 24 months of follow-up. Overall, the pain impact domain showed the largest improvement, with a change from baseline at month 24 of 61.7 points (range of scale 0-100). These results strongly suggest that following exa-cel, participants had rapid and dramatic decreases in pain impact and hurt from pain leading to improved HRQoL.
Reductions in pain experiences following exa-cel infusion were also reflected in the mean pain NRS scores, which substantially declined from baseline in adults and adolescents. It should be acknowledged that pain is complex and there are limitations to assessing the pain experience using PRO measures. For example, pain NRS score measures pain intensity, the recall of which has been shown to rapidly decline as early as 48 hours after a pain event.25 However, the consistency of the data between the different PRO instruments used in these clinical trials would strongly suggest that the overall pain experience among participants with severe SCD substantially improved following exa-cel infusion.
There are some limitations that should be considered when interpreting these results. First, with the exception of the ASCQ-Me and PedsQL SCD module, the PRO tools used here were not developed specifically for SCD. However, it should be noted that these validated tools are often used in hematologic diseases, such as hematologic malignancies, and yield interpretable results, even if not developed specifically for these diseases. Second, the MCIDs were not disease specific. The MCIDs used here have been developed for other hematologic (malignant) disease states and thus can be used to interpret the clinical results generated here. Third, as noted previously, PROs that assess pain do have limitations. For example, the questions for some PRO pain subscales (eg, ASCQ-Me pain episode intensity) may capture information on pain events that occurred before exa-cel infusion and/or instances of chronic pain, and therefore may be imperfect in capturing the acute pain experience post–exa-cel. There were no quantitative pre–exa-cel or post–exa-cel opioid logs that could be used to further interpret data on the pain experience following exa-cel administration because this was not captured during the clinical trial. However, it is important to note that patients in the exa-cel trial had a dramatic decrease in the number of VOCs following exa-cel infusion. Finally, trends over time should be interpreted with caution as the clinical trial is ongoing and not all individuals have had all of their follow-up visits. However, all participants in the trials who had ≥16 months of follow-up since exa-cel infusion (and were therefore considered for the primary end point of the trial) contributed available PRO data at each study visit to the conducted analyses.
In conclusion, adults and adolescents with SCD had early, sustained, and clinically meaningful improvements in HRQoL measures following exa-cel infusion, with improvements observed across different instruments and domains, including physical, emotional, social/family, and functional well-being; pain experience; and overall health status. These results confirm the broad clinical benefits of exa-cel, including associated improvements in quality of life and reductions in pain experience, in patients with severe SCD.
Acknowledgments
The authors thank the patients and their families for participating in these trials, and all site trial investigators and coordinators for their contributions. The authors are also grateful to Nathan Blow and Concetta G. Marfella of Vertex Pharmaceuticals Incorporated, who own stock or stock options in the company, for providing medical writing and editorial support under the guidance of the authors. The authors thank Alexandra Battaglia, of Vertex Pharmaceuticals Incorporated, who owns stock or stock options in the company, for providing graphical design support.
The study sponsor (Vertex Pharmaceuticals Incorporated) designed the protocol in collaboration with the academic authors. Site investigators collected the data, which were analyzed by the sponsor.
Authorship
Contribution: A.S., N.L., P.K., and H.F. developed the initial draft of the manuscript, with writing assistance from the study sponsor (Vertex Pharmaceuticals Incorporated); the sponsor designed the protocol in collaboration with the academic authors, and site investigators collected the data, which were analyzed by the sponsor; and all authors had full access to the study data, all authors participated in subsequent revisions, and all authors approved the final version submitted for publication.
A list of CLIMB SCD-121 and CLIMB-131 Study Group members appears on page 32 and 33 of the “Supplementary Material.”
Conflict-of-interest disclosure: A.S. has been a consultant for Editas Medicine, Medexus Pharmaceuticals, Inc, Renegade Therapeutics, Sangamo, Spotlight Therapeutics, and Vertex Pharmaceuticals Incorporated; has received a research grant from CRISPR Therapeutics; and has received honoraria from Vindico Medical Education. F.L. is on the advisory board for Amgen, Neovii, Novartis, Sanofi, and Vertex Pharmaceuticals Incorporated; and on the speaker’s bureau for Amgen, bluebird bio, Gilead, Jazz Pharmaceuticals, Medac, Miltenyi, Neovii, Novartis, and Sobi. M.Y.M. has been a consultant for bluebird bio, CRISPR Therapeutics, Incyte Corp, and Ossium Health. R.I.L. has participated in clinical trials for bluebird bio, Editas Medicine, Global Blood Therapeutics, and Vertex Pharmaceuticals Incorporated. D.W. is an advisory member for Editas Medicine; and steering committee member for Editas Medicine and Vertex Pharmaceuticals Incorporated. M.J.E. is a consultant with Vertex Pharmaceuticals Incorporated. K.H.M.K. has received grants or contracts from Agios Pharmaceuticals and Pfizer; has received consulting fees from Alexion, Agios, Biossil, Bristol Myers Squibb, Forma Therapeutics, Pfizer, Novo Nordisk, and Vertex Pharmaceuticals Incorporated; has received honoraria from Agios and Bristol Myers Squibb; and has participated in a data safety monitoring board for Sangamo. S.I., P.K., N.L., T.L., J.R., and W.H. are employees of Vertex Pharmaceuticals Incorporated and may hold stock or stock options in the company. S.A.G. is consultant for Vertex Pharmaceuticals Incorporated. H.F. has received consulting fees from Vertex Pharmaceuticals Incorporated, Editas Medicine, and Rocket Pharmaceuticals; has received honoraria from Jazz Pharmaceuticals; has received advisory fees from Rocket Pharmaceuticals; and has served in a leadership or fiduciary position for Vertex Pharmaceuticals Incorporated. The remaining authors declare no competing financial interests.
Correspondence: Haydar Frangoul, Sarah Cannon Pediatric Hematology/Oncology and Cellular Therapy, TriStar Centennial Children’s Hospital, 330 23rd Ave N, Suite 450, Nashville, TN 37203; email: haydar.frangoul@hcahealthcare.com.
References
Author notes
H.F. and S.A.G. contributed equally to this study.
Vertex Pharmaceuticals Incorporated is committed to advancing medical science and improving patient health. This includes the responsible sharing of clinical trial data with qualified researchers. Proposals for the use of these data will be reviewed by a scientific board. Approvals are at the discretion of Vertex Pharmaceuticals Incorporated and will be dependent on the nature of the request, the merit of the research proposed, and the intended use of the data. Please contact CTDS@vrtx.com if you would like to submit a proposal or need more information.
The full-text version of this article contains a data supplement.