TO THE EDITOR:
Chronic lymphocytic leukemia (CLL) exhibits heterogeneous clinical courses, with many patients experiencing indolent disease requiring minimal intervention, whereas others develop aggressive forms characterized by high-risk genetic features or early relapse, which are associated with shorter survival,1-13 especially in time-limited therapies and in relapsed/refractory patients. Targeted therapies, including Bruton tyrosine kinase inhibitors (BTKis) and BCL-2 inhibitors, significantly improved outcomes for these patients.2,5,7,8,14,15 Nevertheless, optimal timing for retreatment is unclear, and strategies to achieve long-term control of high-risk CLL need to be defined.
Current treatment guidelines recommend initiating therapy in patients with advanced or symptomatic disease16 and using minimal residual disease (MRD) status for clinical evaluation, recognizing its growing role as a surrogate end point in trials.16 In clinical trials, MRD assessment is used for response assessment with the aim of achieving undetectable MRD (uMRD). Achieving uMRD is associated with prolonged progression-free survival and overall survival.15,17-22 Although MRD is not routinely used in clinical practice, its potential to guide treatment decisions, particularly in high-risk patients,16 is gaining attention.
Given the poor outcomes of relapsed high-risk CLL, with short progression-free survival and overall survival,3,10,11,23-25 we adopted a strategy of early intervention in selected patients to achieve sustained disease control. This retrospective analysis reports our experience using MRD levels to trigger retreatment with anti-CD20 antibodies in patients with high-risk CLL after prior therapy. We hypothesized that initiating anti-CD20 treatment triggered by rising MRD levels before clinical relapse could proactively improve long-term outcomes in these patients.
This single-center case series included 12 patients with high-risk CLL who experienced MRD relapse after prior treatment. High-risk CLL was defined by complex karyotype (≥3 cytogenetic abnormalities), TP53 abnormalities (del(17p) or TP53 mutations), and/or early relapse (disease progression within 2 years after the end of induction treatment). MRD levels were assessed using 4-color flow cytometry, with uMRD defined as <1 CLL cell in 10 000 leukocytes. MRD relapse was defined as the presence of ≥1 CLL cell in 10 000 leukocytes (detectable MRD [dMRD]) after prior CLL therapy.
Upon MRD relapse, patients were (re-)treated with obinutuzumab or rituximab, depending on previous exposure and tolerability to previous therapies. The objective of this study was to evaluate whether this could delay clinical relapse over an extended time period.
Adverse events (AEs) and serious AEs were considered treatment related when reported from the start of MRD-triggered retreatment until 28 days after the last dose of treatment or at the physician’s discretion.
The 12 patients included in the study represented a heterogeneous group regarding prior therapies and genetic risk factors. Patient characteristics are detailed in Table 1. Six patients (50%) had del(17p), 4 (33%) had TP53 mutations, 2 (17%) had complex karyotype, and 2 (17%) had experienced early relapse. Previous treatments included chemoimmunotherapy (n = 7), venetoclax with (n = 1) or without obinutuzumab (n = 2), ibrutinib (n = 1), or a combination of venetoclax, obinutuzumab, and ibrutinib (n = 1). The duration from uMRD to dMRD after treatment ranged from 2.5 months to 8.8 years. The duration from MRD ≤1% to MRD relapse with MRD >1% after induction treatment ranged from 0.4 months to 17.1 years.
Upon MRD relapse, patients were re-treated with obinutuzumab (n = 8), rituximab (n = 3), or a combination of both (n = 1). All patients (100%) experienced a reduction in MRD levels to <1% of leukocytes after retreatment, with a median duration of MRD ≤1% of 2 years. All patients (100%) experienced a reduction in MRD levels to <10–4 after retreatment, with a median duration of uMRD of 10.7 months. Seven patients (58%) required additional treatment for clinical relapse: venetoclax (n = 2), BTKi (n = 1), or venetoclax plus BTKi (n = 4). Two patients (17%) received allogeneic stem cell transplantation due to Richter transformation or due to CLL progression. Time to next treatment varied, ranging from 0 months to 15.8 years after induction treatment, with a median time of 2.3 years.
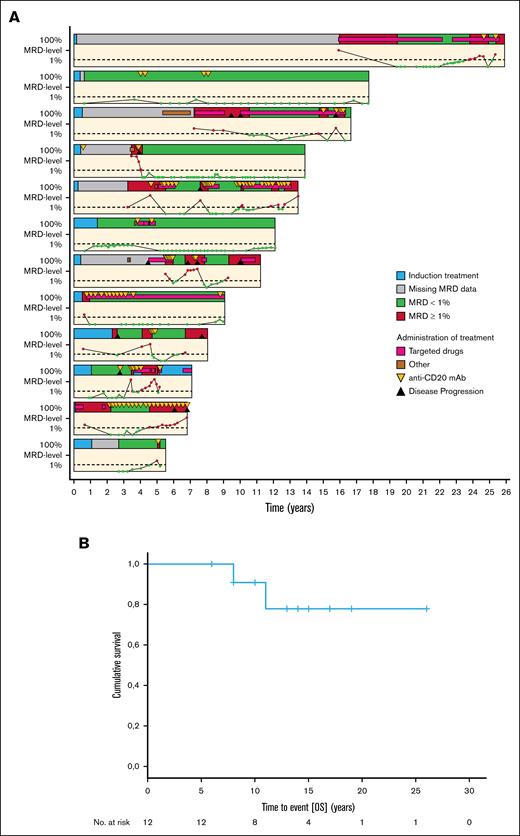
The swimmer plot (Figure 1A) illustrates the long-term control of MRD levels for each patient, demonstrating that MRD-triggered retreatment with anti-CD20 antibodies was effective in maintaining disease control in many cases, with some patients achieving prolonged remission without requiring further treatment. With a median observation time of 14 years, 2 patients died due to CLL progression/Richter transformation. Overall survival is depicted in Figure 1B.
MRD kinetics and survival. (A) Swimmer plot representing the different therapies and MRD levels (<1% and ≥1% CLL cells of all leukocytes) over time for 12 patients with high-risk CLL. (B) Kaplan-Meier curve depicting the OS of the 12 observed patients, with median OS time not reached. mAb, monoclonal antibody; OS, overall survival.
MRD kinetics and survival. (A) Swimmer plot representing the different therapies and MRD levels (<1% and ≥1% CLL cells of all leukocytes) over time for 12 patients with high-risk CLL. (B) Kaplan-Meier curve depicting the OS of the 12 observed patients, with median OS time not reached. mAb, monoclonal antibody; OS, overall survival.
Seven treatment-related AEs were reported in 3 patients (25%), including 5 AEs (71%) of Common Terminology Criteria grade ≥ 3. Five hematologic AEs were reported, including anemia (n = 2) and neutropenia (n = 3). A total of 21 serious AEs were reported in 8 patients (67%), with 2 (17%) defined as treatment related (pleural/pericardial effusion and infusion-related reaction). Two deaths occurred due to disease progression. An overview of AEs is provided in Table 2.
This case series reports an approach to proactively manage patients with high-risk CLL by MRD-guided retreatment with anti-CD20 antibodies before clinical relapse. We demonstrate that patients with high-risk CLL features, including TP53 abnormalities, complex karyotype, and early relapse, could benefit from this MRD-triggered intervention.
The results suggest that this approach can effectively reduce MRD levels and potentially delay clinical relapse in selected patients. Concurrent with International Workshop on CLL guidelines, MRD assessment is recommended for clinical evaluation and as a surrogate end point in clinical trials. By monitoring MRD levels and initiating therapy at the time of dMRD, before clinical disease progression, we could achieve long-term disease control in the majority of patients, some for more than a decade. Therefore, we propose that dMRD can serve as a biomarker to identify patients with high-risk CLL benefiting from early therapeutic intervention with anti-CD20 antibodies. This strategy represents an approach aiming for deep remissions as opposed to continuous treatment until progression, a key consideration when balancing efficacy with long-term toxicity.
One of the most striking findings was the prolonged uMRD duration in some patients after MRD-triggered retreatment, with some individuals remaining in remission for up to 8.8 years without further therapeutic intervention. This suggests that MRD-driven anti-CD20 therapy may not only delay the need for subsequent treatments but also offer the potential for long-term disease control, if not cure, in certain high-risk patients with CLL. This contrasts with continuous treatment with BTKis, in which the acquisition of resistance mechanisms over time is concerning.
Despite these interesting findings, we acknowledge several limitations, including the small sample size, retrospective design, variable MRD assessment time points, and lack of a control group. The study did not evaluate quality of life, and frequent MRD-monitoring may increase the burden on patients and health care resources. Without a control group, we cannot rule out the potential risk of overtreatment in patients who might have remained clinically stable despite rising MRD levels.
However, the results support the hypothesis that an MRD-triggered management strategy may improve outcomes in selected high-risk patients with CLL. Based on this, we plan to design a prospective trial to validate the concept of MRD-guided retreatment compared to standard treatment triggered by clinical relapse and test various MRD thresholds for initiating retreatment.
This retrospective case series demonstrates the potential of MRD-guided retreatment with anti-CD20 antibodies in high-risk patients with CLL. This approach showed promise in reducing MRD levels and delaying clinical relapse, with some patients achieving very long remissions in a situation usually defined by short survival.3,10,11,23-25 All patients experienced a reduction in MRD levels to <1% of leukocytes after retreatment. The duration of uMRD ranged from 2.5 months to 8.8 years. MRD-guided retreatment with anti-CD20 antibodies shows promise as a proactive strategy for managing high-risk CLL, potentially enabling long-term disease control. Further research is needed to define the role of this approach in clinical practice.
The research was approved by the relevant institutional review boards, and all human participants gave written informed consent.
Acknowledgment: The authors thank the patients and their families for contributing to this research article.
Contribution: E.G. provided primary authorship; E.G., P.L., and M.H. provided input and data interpretation; R.L. and S.R. performed statistical analysis, analyzed and interpreted data, and provided figures; and K.F., B.E., P.L., and M.H. enrolled patients, performed research, and contributed to the manuscript.
Conflict-of-interest disclosure: E.G. reports honoraria from AbbVie and AstraZeneca; and travel support from AbbVie. S.R. reports honoraria from Merck Sharp & Dohme (MSD). K.F. reports advisory board fees from AstraZeneca and AbbVie; and speakers’ honoraria and research funding from AbbVie and Roche. B.E. reports advisory board fees from Janssen, AbbVie, AstraZeneca, BeiGene, MSD, Lilly, and Galapagos; honoraria from AbbVie, AstraZeneca, BeiGene, Bristol Myers Squibb (BMS), Lilly, MSD, and Roche; and research funding from AbbVie, AstraZeneca, BeiGene, Janssen, and Roche. P.L. reports research funding from Janssen; and honoraria/advisory board fees and travel support from Janssen, AstraZeneca, BeiGene, and AbbVie. M.H. reports honoraria (speaker’s bureau and/or advisory board) from Roche, Gilead, Janssen, BMS, AbbVie, and AstraZeneca; and research support from Roche, Gilead, Janssen, BMS, AbbVie, and AstraZeneca. R.L. declares no competing financial interests.
Correspondence: Ellinor Goergen, Department I of Internal Medicine, University of Cologne, Kerpener Str 62, 50937 Cologne, Germany; email: ellinor.goergen@uk-koeln.de.
References
Author notes
Original data are available on request from the corresponding author, Ellinor Goergen (ellinor.goergen@uk-koeln.de).