Key Points
This study confirms that transfer gaps <6 months are effective in reducing acute health care utilization for SCD.
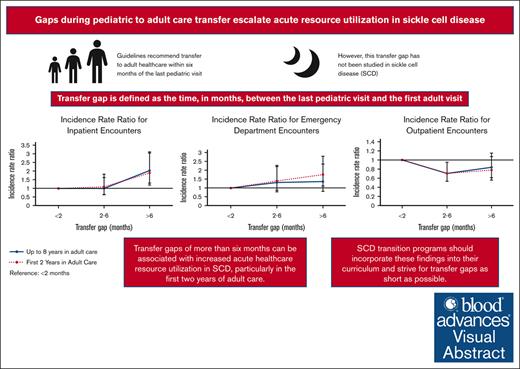
Visual Abstract
Guidelines recommend transfer to adult health care within 6 months of completing pediatric care; however, this has not been studied in sickle cell disease (SCD). We hypothesized that longer transfer gaps are associated with increased resource utilization. Transfer gaps were defined as the time between the last pediatric and first adult visits. We estimated the association between varying transfer gaps and the rates of inpatient, emergency department (ED), and outpatient visits, using negative binomial regression. Health care utilization was evaluated in a mid-south comprehensive program for a follow-up period of up to 8 years (2012-2020) and was restricted to the first 2 years of adult health care. In total, 183 young adults (YAs) with SCD (51% male, 67% HbSS/HbSβ0-thalassemia) were transferred to adult health care between 2012 and 2018. YAs with transfer gaps ≥6 months compared with <2 months had 2.01 (95% confidence interval [CI], 1.31-3.11) times the rate of hospitalizations in the 8-year follow-up and 1.89 (95% CI, 1.17-3.04) when restricted to the first 2 years of adult health care. In the first 2 years of adult care, those with transfer gaps ≥6 months compared with <2 months, had 1.75 (95% CI, 1.10-2.80) times the rate of ED encounters. Those with gaps ≥2 to <6 months compared with <2 months had 0.71 (95 % CI, 0.53-0.95) times the rate of outpatient visits. Among YAs with SCD, a longer transfer gap was associated with increased inpatient and decreased outpatient encounters in adult health care and more ED encounters in the first 2 years of adult health care. Strategies to reduce the transfer gaps are needed.
Introduction
Sickle cell disease (SCD) is a genetic blood disorder that causes complex acute and chronic complications throughout the life span, including vaso-occlusive pain episodes, stroke, and progressive organ damage. Young adults (YAs) with SCD are at risk of a marked increase in disease severity, frequency of acute health care utilization, acute complications, and mortality.1-7 The increase in the risk for morbidity and mortality coincides with the age of transfer from pediatric to adult health care,8 further complicating the health care needs of these YAs and underscoring the importance of uninterrupted comprehensive SCD health care throughout their lifetime. Health care transition aims to provide a structured approach to prepare, transfer, and integrate YAs into adult care.9,10 Thus, the transfer from pediatric to adult care is central to the complex and multifaceted process of health care transition. The entire process of health care transition targets many levels (ie, patient, provider, and health system) and spans over several years, including the period of care transfer, a component of health care transition.11
Barriers to health care transfer and the overall transition in SCD include systems of power (eg, institutional and practitioner bias) and inequity that impact patients’ lives and medical care, disease complexity, patient-perceived lack of knowledge of the transition process, challenges in care coordination across providers, and limited access to health insurance coverage in adulthood.12,13 Facilitators of adult care transfer include being treated at the same hospital for both pediatric and adult programs, having the genotype HbSS, and/or receiving SCD-modifying therapy.14 Understanding these barriers has informed new interventions and has challenged adult providers to improve relationships between pediatric and adult providers, as well as prompted adult providers to increase their self-efficacy in caring for conditions once considered childhood diseases.15
Despite the recommendations of different professional societies and health care experts that YAs with chronic health conditions should transfer to adult-centered care within 6 months of leaving pediatric care,16-19 YAs may experience transfer gaps (defined as the time from the last pediatric-focused visit to the first adult-focused visit) of >12 months.20 Transfer gaps might contribute to poor health outcomes among YAs with SCD, but there are no data investigating the effects of prolonged adult care transfer gaps in SCD. Delays in establishing adult health care among YAs with SCD may place patients at risk for poor health outcomes and are yet to be studied. When YAs with SCD do not promptly transition to a comprehensive SCD program, they may have limited access to evidence-based specialized SCD care.21 Thus, patients with prolonged pediatric to adult care gaps may be forced to rely on emergency department (ED) care, potentially resulting in increased acute health care utilization.22
It has been previously shown that, compared with adolescents, YAs experience increased organ dysfunction and acute visits.23 A timely, well-coordinated transfer from pediatric to adult health care is critical to increase access to high-quality, comprehensive SCD care and improve health outcomes for YA with SCD.17,24 Given the complex health care needs of YAs with SCD, it remains unclear whether the recommended 6-month transfer period is optimal for SCD.17 This study investigated the association between varying transfer gaps between the last pediatric visit and the first adult visit and health care resource utilization for YA with SCD. We hypothesized that transfer gaps of ≥6 months from pediatric to adult-centered health care would be associated with higher frequencies of acute health care resource utilization and lower frequencies of outpatient visits in adult care.
Methods
Participant selection
This study included patients diagnosed with SCD who were followed up by a pediatric program at a comprehensive sickle cell center in the Mid-South United States and who participated in a transition to an adult health care program that has been previously described.8 In summary, the program begins transition preparation and planning at the age of 12 years, including transition readiness and neurobehavioral assessments. At the age of 17 years, patients are introduced to adult medical facilities through a Transition Tour Program.8 During the last pediatric visit, the first adult visit is scheduled for a maximum of 30 days after the last pediatric visit. Patients transfer to adult health care at the age of 18 years, and the program uses a colocated care delivery model for adult health care integration between the ages of 18 and 25 years.25 In the colocated model, patients are seen by both pediatric (physicians, psychologists, and nurse educators) and adult providers (physicians, social workers, and advance practice practitioners), who comanage their care in the adult care setting. When patients do not complete adult care transfer (ie, fulfill the first visit in adult care), pediatric providers will attempt to reschedule the adult appointment for up to 1 year and then completely discontinue pediatric care. This transition program was established in 2007 for children only and expanded to include YAs in 2012.
Participants were included in the analysis if they completed care at a pediatric institution during the years 2012 to 2018 and fulfilled their first adult visit to a partner adult facility. Participants were retrospectively followed up from their first adult visit through 31 December 2020, for a minimum of 2 years of follow-up and a maximum of 8 years of follow-up. Those who completed care at the pediatric institution during the years 2012 to 2018 but did not fulfill an adult visit were classified as either lost to follow-up, abandoned care during adolescence, relocated during adolescence, or death during adolescence. All study activities were approved by the institutional review board.
Variable specification
As the exposure of interest, the gap in health care during transfer, or transfer gap, was defined as the time, in months, between the last pediatric visit and the first fulfilled adult visit. The dates of the last pediatric visit and the first adult visit were extracted from the transition database and reviewed. The transfer gap was evaluated as a 3-ordinal variable (<2 months, ≥2 months to <6 months, and ≥6 months) to evaluate whether health care utilization increased as the transfer gap in SCD-specific care increased. The primary interest in this analysis was to examine the 6-month time point given current recommendations to complete the transfer of patients to adult health care within 6 months of their last pediatric visit.18,19
As the outcomes of interest, all adult routine outpatient visits, inpatient hospitalizations (i.e., hospital admissions), and ED records were abstracted from the medical records and reviewed. Visits were evaluated by type (outpatient, inpatient, or ED) over the 8-year follow-up period. Inpatient visits were classified as a hospital stay lasting ≥24 hours. Infusion center visits were grouped with ED visits, as both were <24 hours in duration and for similar reasons. The median frequency of each visit type per year of follow-up in adulthood was determined for each participant. As a subanalysis, the adult visits were limited to only the first 2 years of adult care to evaluate the short-term effect of transition gaps on health care resource utilization. Additionally, as a sensitivity analysis, the consistency of health care utilization was examined. That is, participants with >2-year gaps in their adult health care utilization records were considered outliers and were removed for the sensitivity analysis.
As covariates of interest, demographic information included sex, SCD genotype (HbSS/HbSβ0-thalassemia or HbSC/HbSβ+-thalassemia), hydroxyurea utilization (ever vs never), chronic blood transfusions (ever vs never), primary insurance at the time of transfer (public vs private), and year and age at transfer (ie, last pediatric visit). Year of transfer was divided into 2 categories (2012-2015 and 2016-2018) to account for the maturity of the transition program. Additionally, the participants’ pediatric inpatient, ED, and outpatient history were summarized as the number of visits for SCD in the last 2 years of pediatric health care.
Statistical analysis
Descriptive statistics (median and interquartile range [IQR], frequencies, and percentages) were used to describe the sample. χ2 and Wilcoxon rank-sum tests were used to compare the characteristics between those who were included in the study and those who were ineligible to be included in this study, and between those who transferred within 6 months and those who transferred in >6 months. The associations between varying transfer gaps and adult health care visits per year were evaluated using generalized linear models using the negative binomial distribution. Multivariable models were fit to assess the rate of health care utilization visits as predicted by the transfer gap duration period between pediatric and adult health care, with log patient years as a model offset. Patient years were defined as the number of years of recorded visits in adult health care. The presence of confounding by covariates was indicated if the main effect differed by >10%. If a covariate was identified as a confounder, it was included in the adjusted model. As a sensitivity analysis, similar analyses were performed on the sample restricted to the first 2 years of care. The type 1 error rate for all analyses was set at 0.05 and all analyses were conducted using SAS version 9.4 (Cary, NC).
This study was approved by the institutional review board of St. Jude Children's Research Hospital.
Results
There were 356 patients with SCD who ended pediatric care at our institution between 2012 and 2018. Approximately 48% (n = 173) were not eligible for inclusion in this study due to transferring elsewhere (n = 80), lost to follow-up (n = 91), or death during adolescence (n = 2). Of those who completed the transfer, 183 YAs (51% male, 67% HbSS/HbSβ0-thalassemia) attended 1 of 2 regional, partner adult comprehensive SCD institutions and were included in this study (Table 1). There was a statistically significant difference in genotype (P = .001), year at transfer (P < .0001), and age at transfer (P < .0001) when comparing eligible participants with ineligible (supplemental Table 1).
Approximately 88% of the included participants were transferred to adult health care within the recommended 6 months (Table 1). The median transfer gap was 1.4 months (IQR, 1.0-2.2). Those who transferred to adult care within 6 months attended more outpatient visits in pediatric and adult care (supplemental Table 2). There were no other significant differences between the 6-month transfer gap statuses. The participants were followed up in adult care for a median of 5.0 years (IQR, 3.0-7.0). Females had more frequent ED visits (supplemental Table 3). Those with HbSS/HbSβ0-thalassemia, those who had used hydroxyurea, and those who had chronic transfusions had more frequent inpatient, ED, and outpatient encounter visits. Those with public insurance had more frequent inpatient and ED visits than those who were uninsured.
YAs with transfer gaps of 6 months or longer had 2.01 (95% confidence interval [CI], 1.31-3.11) times the adjusted incidence rate of inpatient visits compared with those with gaps of <2 months (Table 2). After restricting the analysis to the first 2 years of adult care, YAs with transfer gaps of 6 months or longer had 1.89 (95% CI, 1.17-3.04) times the adjusted incidence rate of inpatient visits compared with those with a transfer gap of <2 months. There was no significant increase in the rate of inpatient encounters for those who transferred to adult care 2 to 6 months after leaving pediatric care compared with those who transferred in <2 months. Transfer gap length was not significantly associated with ED encounters during the 8-year follow-up (incidence rate ratio (IRR), 1.37; 95% CI, 0.80-2.33). However, after restricting the first 2 years of adult care, YAs with transfer gaps ≥6 months had 1.75 (95% CI, 1.10-2.80) times the adjusted incidence rate of ED encounters compared with those with <2 months transfer gaps (Table 2). Transfer gaps between 2 and 6 months compared with <2 months were associated with fewer outpatient encounters in adult care (IRR, 0.71; 95% CI, 0.53-0.96; Table 2). The association was similar after restricting the analysis to the first 2 years of adult care (IRR, 0.71; 95% CI, 0.53-0.95; Table 2).
Sensitivity analysis
There were 14 participants who had large gaps (>2 years) in the captured adult care utilization data. Compared with the 169 participants with consistent adult care utilization data, those with large gaps in data capture were less likely to have a severe SCD genotype and less likely to have used hydroxyurea (supplemental Table 4). These 14 participants also contributed less adult patient time (median 2.5 years [IQR, 2.0-5.0] compared with 5.0 years [IQR, 4.0-7.0]) and attended fewer outpatient visits in adult care (median 1.0 years [IQR, 0.8-1.9] compared with 5.3 years [IQR, 3.0-9.0]).
When repeating the analysis with only those with consistent health care utilization data (n = 169), the results did not change. Individuals with >6 months transfer gap had 2.24 (95% CI, 1.44-3.47) times the adjusted incidence rate of inpatient encounters compared with those with <2 months transfer gap (Table 2). When evaluating the ordinal transfer gap and its association with ED encounters, there was not a significant association for the complete follow-up. However, similar to the full sample, after restricting to the first 2 years of adult care, those with >6 months transfer gap had 1.80 (95% CI, 1.11-2.92) times the adjusted incidence rate of ED encounters compared with those with <2 months transfer gap. The association between ordinal transfer gap and outpatient encounters was similar to the complete sample (IRR, 0.69; 95% CI, 0.51-0.93).
Discussion
Because delays in establishing adult care during health care transition may result in the exacerbation of chronic diseases, we aimed to investigate the effect of varying lengths of transfer gaps from pediatric to adult-centered care on health care utilization among YAs with SCD.1,2,4 We confirmed our hypothesis that longer delays in establishing adult health care after pediatric care are associated with greater acute health care resource utilization and fewer health care maintenance (ie, outpatient) SCD visits. These findings emphasize the importance of swift transfer from pediatric to adult care among YAs with SCD.
Our findings are consistent with the literature on other chronic diseases. Among youth with HIV, those who successfully transferred to adult care within 3 months of leaving pediatric care were 76% more likely to have suppressed viral load in adult care compared with youth who did not transfer within 3 months.26 It has also been shown that among patients with type 1 diabetes, individuals who are noncompliant with transfer are more likely to have diabetes-related hospitalizations and fewer clinic appointments in the year before transfer.27 As with other chronic diseases, our results demonstrated that a shortened transfer gap between pediatric and adult care could represent a clinically meaningful quality indicator of a successful transition, and our data now support this indicator of health care transition for the SCD population.
Studies have demonstrated an increase in acute health care utilization surrounding the transition to adult care.5-7 An increase in acute health care utilization after a large transfer gap likely reflects increased morbidity and mortality imparted by temporary health care discontinuation. Our findings support the current recommendations to engage and coordinate patients with chronic conditions into adult health care within 6 months from transferring out of pediatric care.17 However, our findings also denote that delaying establishing adult care after completion of pediatric care has both short- and long-term effects on higher adult acute health care utilization for YAs with SCD. We also found that an intermediate transfer gap length (2-6 months) was associated with lower frequencies of health maintenance (ie, outpatient) visits in adult care. Outpatient visits are critical to addressing health needs and preventing adverse outcomes. It has been previously demonstrated that outpatient follow-ups are associated with fewer rehospitalizations.28
Interventions to prevent gaps in health care between pediatric and adult care should be developed and implemented in transition programs. It has been previously shown that adolescents and YAs with type 1 diabetes are significantly less likely to report a gap in care if they feel prepared for transition.29 Programs with transition navigators have been shown to improve transition readiness, reduce loss to follow-up, and improve medication adherence.30,31 The primary barrier to transition is comfortability with the adult providers and facilities.13 Transition programs with early introduction to adult care,32 health literacy preparation,25, and promotion of patient self-efficacy19,33,34 may improve continuity of care throughout the health care transition period. Efforts to address neurocognitive deficits should also be considered, as these deficits might have a negative impact on engaging in adult care and are associated with low health literacy.35-37
Limitations
This study only included patients who were transferred within the health care system and, therefore, excluded those who were transferred to adult care facilities outside of this health care system because their records were not available. Additionally, it is possible that YAs were seen at adult health care facilities outside the program network, and these visits may not have been captured in our data. However, data ascertainment concerning health care resource utilization for those utilizing 1 of the 2 adult partner institutions was high in our program, reducing the risk of outcome misclassification. A sensitivity analysis removing those with >2 years of missing adult care utilization was performed in an effort to alleviate this limitation, and similar results, if not stronger, were found. This study also excluded all individuals who failed to transfer to adult care; therefore, conclusions cannot be drawn about this population. Moreover, the present sample represents a cohort that spans over 3 institutions, 1 pediatric and 2 adult programs, with a resource-rich transition program8 that may have reduced generalizability to other programs that lack partner institutions. Future studies would benefit from a multicenter evaluation to improve the generalizability of these findings. Lastly, low-income children may be removed from Medicaid at the age of 19, and loss or change of insurance was not measured in this analysis and may present unmeasured confounding.
Conclusion
Health care transition is a complex process spanning over many years.15 Current health care guidelines and expert consensus recommend that patients should engage in adult care within 6 months of leaving pediatric health care.18,19 Although we recognize that ensuring short transition gaps is important to reduce health deterioration among YAs with SCD, we do acknowledge that other factors beyond prolonged transfer gaps may also affect the optimal transition process and must be addressed (eg, institutional racism, poor care that adults receive in EDs).38 Notwithstanding, this study demonstrated that transfer gaps of >6 months can be associated with increased acute health care resource utilization in SCD, particularly in the first 2 years of adult care. SCD transition programs should incorporate these findings into their curriculum and strive for transfer gaps as short as possible (ideally shorter than 2 months) and no longer than 6 months. Future studies should continue to investigate the association between the duration of transfer gaps from pediatric to adult care for even longer-term clinical effects and invest in interventions and strategies to reduce the transfer gap in the SCD population.
Acknowledgments
The authors thank Courtney Mays and Gail Fortner for their support with regulatory matters, and Anjelica Saulsberry and Pradeep Podila for their support with data collection.
J.S.H received funding from U1EMC19331 from American Lebanese Syrian Associated Charities and the Health Resources and Services Administration, U01HL133996 from the National Heart, Lung, and Blood Institute and NU58DD000019 from the National Center on Birth Defects and Developmental Disabilities during the conduct of this study. J.S.P. was supported by K01HL125495 from the National Heart, Lung, and Blood Institute at the time of this project.
Authorship
Contribution: K.E.H. collected the data, conceptualized and designed the study, carried out the statistical analysis, drafted the initial manuscript, and reviewed and revised the manuscript; M.K. conceptualized and designed the study, drafted the initial manuscript, and reviewed and edited the manuscript; J.S.H. collected the data, conceptualized and designed the study, coordinated and supervised the data collection, and reviewed and edited the manuscript; M.P.S., V.G.N., and N.S. conceptualized and designed the study and reviewed and edited the manuscript; J.G.M. and J.S.P. critically reviewed the manuscript for important intellectual content; M.N. and S.A. coordinated data collection and edited the manuscript; and all authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Kristen E. Howell, Department of Epidemiology and Biostatistics, Texas A&M School of Public Health, 212 Adriance Lab Rd, College Station, TX 77843; email: khowell1@tamu.edu.
References
Author notes
Raw data were generated at St. Jude Children's Research Hospital. Derived data supporting the findings of this study are available on request from the corresponding author, Kristen E. Howell (khowell1@tamu.edu).
The full-text version of this article contains a data supplement.