Key Points
CAST regimen is safe and effective in reducing acute GVHD after haploidentical peripheral blood transplantation.
Our outcomes provide an impetus to further examine this novel combination in GVHD prevention.
Abstract
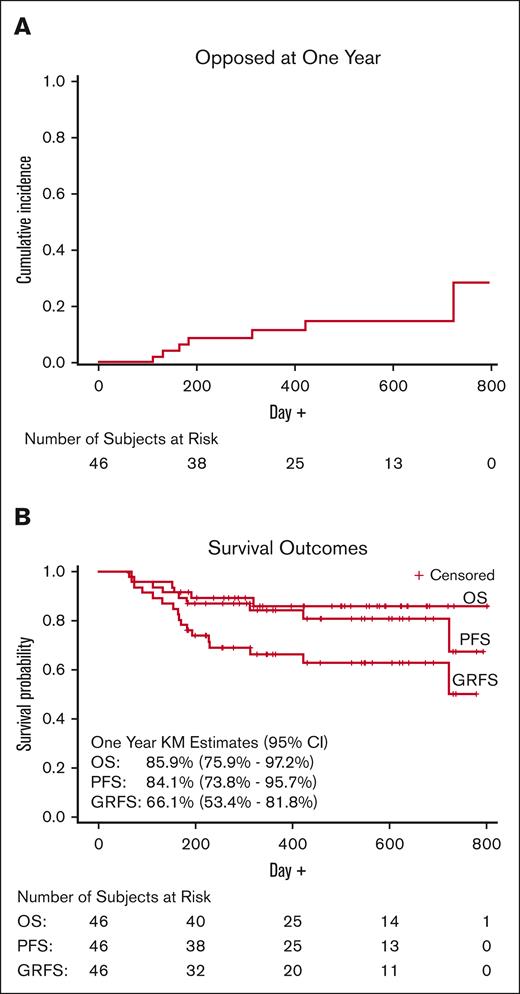
Reducing the incidence of graft-versus-host disease (GVHD) after haploidentical hematopoietic stem cell transplantation (HSCT) is warranted. Posttransplant cyclophosphamide (PTCy) is the main agent used for GVHD prevention in this setting. It remains unknown whether costimulation blockade can be safely combined with PTCy and enhance its efficacy. We performed a phase 1b-2 clinical trial to examine the combination of PTCy, abatacept, and a short course of tacrolimus (CAST) after peripheral blood haploidentical HSCT. The primary end point was the incidence of grades 2-4 acute GVHD by day +120. The study enrolled 46 patients with a median age of 60 years (range, 18-74 years). The cumulative incidences of grades 2-4 and 3 or 4 acute GVHD were 17.4% (95% confidence interval [CI], 9.2-32.9) and 4.4% (95% CI, 1.1-17.1), respectively. With a median follow-up of 15.3 months, the cumulative incidence of 1-year treatment-related mortality was 4.4% (95% CI, 1.1-17.1). The estimated 1-year moderate-to-severe chronic GVHD rate, relapse rate, progression-free survival, overall survival, and GVHD- and relapse-free survival were 15.9% (95% CI, 8-31.7), 11.7% (95% CI, 5-27.2), 84.1% (95% CI, 73.8-95.7), 85.9% (95% CI, 75.9-97.2), and 66.1% (95% CI, 53.4-81.8), respectively. Toxicities were similar to those expected in patients receiving haploidentical HSCT. This clinical trial showed that the CAST regimen is safe and effective in reducing the rate of grades 2-4 acute GVHD after haploidentical peripheral blood HSCT. This trial was registered at www.clinicaltrials.gov as #NCT04503616.
Introduction
Since the introduction of posttransplant cyclophosphamide (PTCy) to circumvent ex vivo T-cell depletion for the prevention of graft-versus-host disease (GVHD) after haploidentical hematopoietic stem cell transplantation (HSCT), the use of haploidentical donors has increased significantly. This strategy has addressed an important issue of health care disparity in the field of blood and marrow transplantation by expanding donor options for patients from racial and ethnic minorities, who otherwise lack suitable donors.1 However, a recent retrospective registry study demonstrated inferior outcomes after haploidentical transplantation compared with matched unrelated donor (MUD) transplantation in patients with myeloid neoplasms receiving the same PTCy-based GVHD prevention regimen.2 Patients experienced a higher incidence of grade 3 or 4 acute GVHD after haploidentical transplantation. The incidence of chronic GVHD was also increased among patients receiving myeloablative conditioning (MAC). Among those receiving reduced-intensity conditioning (RIC), there was higher treatment-related mortality (TRM) and lower overall survival (OS) after haploidentical transplantation than among those receiving MUD transplantation. This provided us with the impetus to develop a more effective GVHD prevention regimen for haploidentical transplantation, aiming to “level the playing field” for patients receiving a transplantation from alternative donors.
We designed a regimen consisting of PTCy, abatacept, and a short course of tacrolimus (CAST). PTCy reduces and impairs the functionality of alloreactive effector cells while promoting the preferential recovery of regulatory T cells.3 Multiple studies have demonstrated the efficacy of PTCy in preventing chronic GVHD after haploidentical transplantation.4 However, the incidence of acute GVHD has remained less favorable, particularly after peripheral blood grafts, with an adjusted cumulative incidence of grades 2-4 and 3 or 4 acute GVHD in the range of 42% and 10%, respectively.5 Abatacept is a soluble fusion protein of the Fc region of immunoglobulin G1 and the extracellular domain of cytotoxic T-lymphocyte–associated antigen 4. Abatacept blocks the interaction of CD80/CD86 with CD28 and impairs T-lymphocyte costimulation. In a study that combined abatacept with tacrolimus and methotrexate for the prevention of GVHD after MUD and mismatched unrelated donor (MMUD) HSCT, abatacept decreased the incidence of acute but not chronic GVHD when compared with the control group, leading to its US Food and Drug Administration approval for prevention of acute GVHD in this setting.6 We hypothesized that the combination of PTCy and abatacept would be safe and effective in GVHD prevention and would allow us to shorten the duration of calcineurin inhibition after haploidentical peripheral blood transplantation.
Methods
Trial design and oversight
This was an investigator-initiated, single-institution, phase 1b-2 clinical study evaluating the safety and efficacy of the CAST regimen for prevention of GVHD after peripheral blood haploidentical HSCT. An investigational new drug application was approved by the US Food and Drug Administration (IND 149936). The study was approved by the New York University Grossman School of Medicine institutional review board and was conducted in accordance with the Declaration of Helsinki and the International Council for Harmonisation guidelines for Good Clinical Practice. All patients provided a written informed consent before initiation of study procedures. The trial procedures were monitored by the Clinical Trial Office of the Perlmutter Cancer Center at New York University Langone Health, a National Institutes of Health–designated comprehensive cancer center. The Perlmutter Cancer Center Data and Safety Monitoring Committee provided monitoring of patient safety per the National Cancer Institute–approved data safety monitoring plan.
Patients
Candidate patients were those undergoing haploidentical HSCT from a related donor for hematological malignancies. Patients with donor-specific antibodies or positive crossmatches were excluded. Eligible patients were aged ≥18 years and had a Karnofsky performance status ≥70, no evidence of progressive infectious process, adequate organ function with creatinine clearance >50 mL/min per 1.72 m2, total bilirubin and alanine aminotransferase and aspartate aminotransferase of <2× the upper limit of normal (except for those with Gilbert syndrome), alkaline phosphatase levels ≤250 IU/L, adjusted carbon monoxide diffusion capacity >60%, and left ventricular ejection fraction >45%. Patients with active ischemic heart disease or myocardial infarction within 6 months or New York Heart Association congestive heart failure class 3 or 4 were excluded. Patients were required to have negative HIV test. Women of childbearing age had negative pregnancy test results.
Treatment
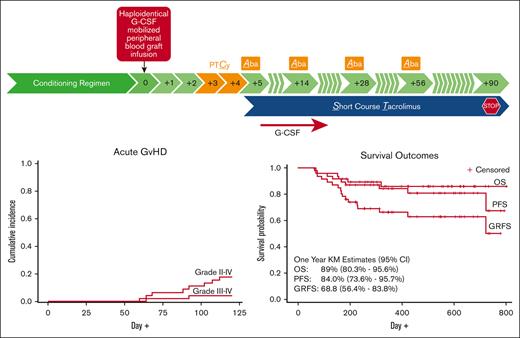
Figure 1 represents the treatment scheme. Patients received nonmyeloablative (NMA) conditioning, RIC, or MAC at the discretion of the treating physician. The decision was based on the patient’s age, performance status, hematopoietic cell transplantation–specific comorbidity index (HCT-CI),7 and disease type and status. Myeloablative total body radiation (TBI)-based conditioning regimens were reserved for patients with acute lymphoblastic leukemia. Conditioning regimens are summarized in supplemental Table 1. All patients received granulocyte colony-stimulating factor–mobilized peripheral blood hematopoietic stem cell grafts on day 0. GVHD prophylaxis consisted of PTCy 50 mg/kg IV daily on days +3 and +4; abatacept 10 mg/kg IV over 30 minutes on days +5, +14, and +28; and tacrolimus starting at 0.02 mg/kg per day continuous IV infusion initiated on day +5 and adjusted to maintain a therapeutic drug level thereafter. Tacrolimus was switched from oral route as tolerated and tapered starting on day +60 to complete on day +90 in the absence of GVHD. Based on the timing of the observed acute GVHD and abatacept half-life, the protocol was amended, and the last 18 patients enrolled received a fourth dose of abatacept on day +56. All patients received granulocyte colony-stimulating factor support. All supportive care was provided following institutional practices.
End point measurements
The primary end point was the incidence of grades 2-4 acute GVHD by day +120. Acute GVHD was graded based on the modified Glucksberg criteria, with increasing severity from grade 1 to 4.8 Secondary end points included the incidence of chronic GVHD scored per the National Institute of Health Consensus Development Project,9 TRM, relapse rate (RR), OS, and GVHD- and relapse-free survival (GRFS), defined as absence of grades 3 and 4 acute GVHD, chronic GVHD requiring systemic steroids, relapse, and death.
Statistical considerations
Based on a 2-stage optimal Simon design, we could detect a reduction in the incidence of grade 2-4 acute GVHD from 50% with the standard of care1 to 30% with the experimental regimen, with α = 0.05 and a power of 82%, at the conclusion of the study with 46 patients. At the end of the first stage, the trial would be stopped for futility if ≥9 of 22 patients developed grade 2-4 acute GVHD. The incidence of grade 2-4 acute GVHD would be estimated at the end of the trial with exact 95% Clopper Pearson confidence intervals (CIs). If the observed incidence was 30%, the exact CI would range from 17.4% to 45.3% with 46 patients (calculations from PASS 2019, NCSS, J. Hintze, Kaysville, UT). Additional monitoring included predefined stopping rules for excessive TRM, toxicity, and primary graft failure, each with 3 interim and a final evaluation. For acute and chronic GVHD, cumulative incidence is estimated with death as a competing risk. For RR, the cumulative incidence was estimated with TRM as a competing risk. For TRM, cumulative incidence was reported with relapse as a competing risk. GRFS and OS rates were estimated using Kaplan-Meier methods.
Results
Patients
From September 2020 to August 2022, of the 61 patients receiving haploidentical HSCT at NYU Langone Health, 46 patients were enrolled in the study. Supplemental Figure 1 depicts the exclusion rationale. The trial did not meet its stopping criteria for futility after the first 22 patients were enrolled. Other safety stopping criteria rules were also not triggered. Consequently, enrollment continued until all prespecified 46 patients were enrolled. All patients received the planned treatment. Tacrolimus was stopped by day +90 in all but 9 patients, 2 cases were due to protocol violations. With a data cutoff date of 6 February 2023, the median length of follow-up was 15.3 months (range, 6.2-28.9 months). Table 1 summarizes the patient and transplantation characteristics. Notably, 41.3% of patients enrolled were from minority groups.
Engraftment
All study patients achieved neutrophil engraftment at a median of 18 days (range, 13-30 days). One patient died before achieving platelet engraftment. All remaining patients (n = 45) achieved platelet engraftment at a median of 30 days (range, 16-125 days; Figure 2). Whole-blood donor chimerism was ≥97% in all patients by day +48. The patient who achieved neutrophil engraftment on day +30 met the protocol-defined criteria of primary graft failure. However, the patient had full donor chimerism by day +30. One patient developed secondary graft failure with endogenous reconstitution of hematopoiesis. Another patient developed stable mixed chimerism. Both these patients had no evidence of disease relapse. All other patients maintained donor chimerism ≥97% in the absence of disease relapse.
Engraftment. Cumulative incidence of neutrophil engraftment on day +30 and platelet engraftment on day +100.
Engraftment. Cumulative incidence of neutrophil engraftment on day +30 and platelet engraftment on day +100.
Acute and chronic GVHD
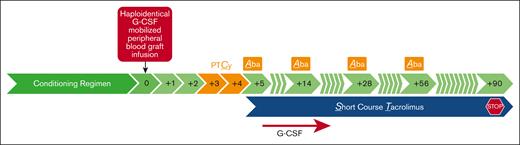
The day +120 cumulative incidence of grade 2-4 acute GVHD with death as a competing risk was 17.4% (95% CI, 9.2-32.9). Grade 3 acute GVHD occurred in 2 patients (4.4%; 95% CI, 1.1-17.1; Figure 3A). No patient developed grade 4 acute GVHD. Of the 18 patients who received 4 doses of abatacept, 3 (16.6%) developed grade 2 acute GVHD; none of these patients developed grade 3 or 4 acute GVHD. The median onset of acute GVHD was 90 days (range, 60-112 days). There were no cases of acute GVHD of the liver or steroid-refractory acute GVHD. Chronic GVHD occurred in 7 patients including 1 patient with overlap syndrome. The 1-year cumulative incidence of moderate-to-severe chronic GVHD was 15.9% (95% CI, 8-31.7; Figure 3B). The median time of onset of chronic GVHD was 171 days (range, 113-230 days). There was no death attributable to GVHD.
Cumulative incidence of acute and chronic GVHD. Cumulative incidence of GVHD with death as a competing risk. (A) Acute GVHD grade 2-4 and (B) chronic GVHD, moderate-to-severe.
Cumulative incidence of acute and chronic GVHD. Cumulative incidence of GVHD with death as a competing risk. (A) Acute GVHD grade 2-4 and (B) chronic GVHD, moderate-to-severe.
Toxicity and infectious complications
One patient presented with thrombotic microangiopathy secondary to tacrolimus on day +41. This resolved after decreasing the tacrolimus dose. There were 2 cases of sinusoidal obstructive syndrome; both cases resolved, with 1 requiring therapy with defibrotide. Cytomegalovirus reactivation occurred in 45.7% of patients and required preemptive antiviral therapy. Epstein-Barr virus reactivation occurred in 2 patients requiring treatment with rituximab. BK cystitis was observed in 32.6% of the patients; only 1 patient required specific therapy with cidofovir. Bacterial infections included Clostridium difficile colitis (8.5%), Yersinia entercolitica colitis, and astrovirus colitis (2%), bacteremia (17%), osteomyelitis (2%), Toxoplasma gondii pneumonia (2%), and cellulitis (2%). Other ≥3 grade toxicities included cardiac arrhythmia (n = 3), pericardial effusion (n = 2), and papilledema (n = 1). Two deaths were attributed to treatment: 1 due to idiopathic interstitial pneumonia syndrome and 1 to cytomegalovirus and Toxoplasma gondii reactivation. The 1-year cumulative incidence of TRM was 4.4% (95% CI, 1.1-17.1).
Relapse, survival, and GRFS
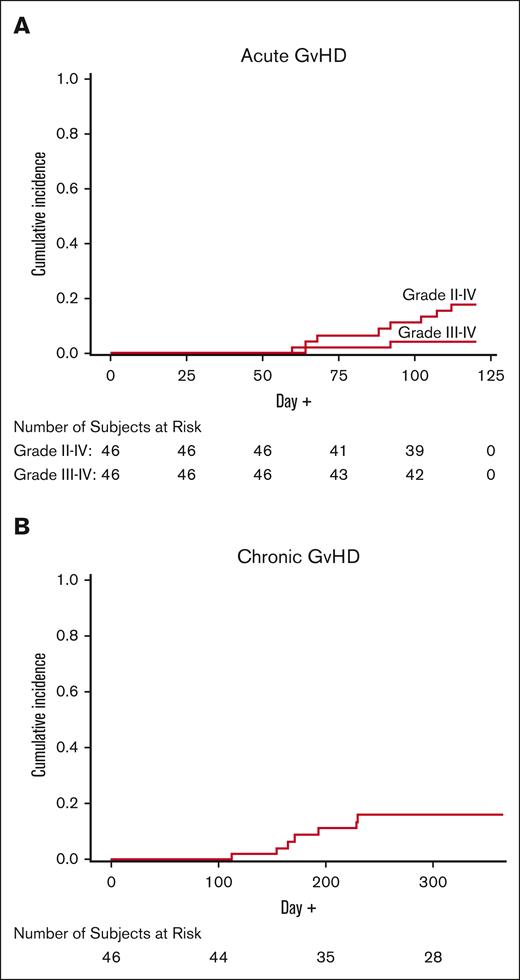
Seven patients relapsed after transplantation; median of 184 days (range, 112-723 days). Relapses included 3 patients with B-cell acute lymphoblastic leukemia, 2 patients with acute myelogenous leukemia, 1 patient with HTLV-1–associated adult T-cell lymphoma, and 1 patient with blastic plasmacytoid dendritic cell neoplasm leukemia. One-year cumulative incidence of relapse was 11.7% (95% CI, 5-27.2; Figure 4A). Although it was not a protocol-specified end point, the Kaplan-Meier 1-year estimated progression-free survival rate was 84.1% (95% CI, 73.8-95.7). One-year OS and GRFS rates were 85.9% (95% CI, 75.9-97.2) and 66.1% (95% CI, 53.4-81.8), respectively (Figure 4B).
Outcomes. (A) One-year cumulative incidence of relapse. (B) Kaplan-Meier survival curves.
Outcomes. (A) One-year cumulative incidence of relapse. (B) Kaplan-Meier survival curves.
Immune reconstitution
Enumeration of T-cell subsets, including CD4+, CD8+, CD19+, and natural killer (CD56+CD16+) T cells, is summarized in Figure 5. The median counts of CD4+, CD8+, CD19+, and natural killer (CD56+CD16+) T cells on day +180 were 161 (range, 26-795), 346 (range 9-263), 237 (range 0-1217), and 262 (range 12-1682) cell per μL, respectively.
Immune reconstitution. Violin plot constructed using https://www.bioinformatics.com.cn/en.
Immune reconstitution. Violin plot constructed using https://www.bioinformatics.com.cn/en.
Discussion
This phase 1b-2 trial demonstrates the safety and efficacy of CAST combination, a novel GVHD prevention regimen after peripheral blood haploidentical HSCT. In this study, the CAST regimen was associated with excellent rates of GVHD, NRM, RR, OS, and GRFS in comparison with that presented in historical data.5
The underrepresentation of minorities in blood and marrow donor registries continues to pose a challenge for patients from certain racial and ethnic groups. Meanwhile, haploidentical family members represent an immediately available option in nearly all cases when suitable MUDs are not available.1,10 We believe that the CAST regimen is a step toward closing this health care disparity gap by reducing the incidence of GVHD and equalizing the outcomes of haploidentical in comparison with those of MUD transplantations.
Our results also compare favorably with those of other alternative donor sources, such as MMUDs and umbilical cord blood (UCB). In a National Marrow Donor Program–sponsored multicenter phase 2 trial, patients received allogeneic HSCT from MMUDs with PTCy, tacrolimus, and mycophenolate mofetil (MMF). Although the source of graft in this study was bone marrow as opposed to peripheral blood, the rates of grades 2-4 and 3 or 4 acute GVHD and chronic GVHD were 43%, 18%, and 36% for patients who received MAC, and 33%, 0%, and 18% after RIC, respectively.11 One-year GRFS rates were 38% and 55% in the MAC and RIC cohorts, respectively. In a smaller single center study using peripheral blood grafts, the rates of grades 2-4 and 3 or 4 acute GVHD were 50% and 18%, respectively; the rate of chronic GVHD was 48%; 1-year GRFS rate was 68%.12 In the ABA2 study, the MMUD stratum enrolled 43 pediatric and adult patients. Patients received peripheral blood or bone marrow grafts after MAC or RIC. The GVHD prophylaxis consisted of abatacept (on days −1, +5, +14, and +28) with tacrolimus and methotrexate. The rates of grades 2-4 and 3 or 4 acute GVHD were 41.9% and 2.3%, respectively. However, the rate of moderate-to-severe chronic GVHD was excessively high, at 57.9%.6 A follow-up study (ABA3) is examining whether 8 doses of abatacept will decrease the incidence of chronic GVHD (NCT0430740). When UCB transplantations were compared with haploidentical bone marrow transplantation after RIC in 2 parallel phase 2 trials, the incidences of acute (grades 2-4, 37% and 28%, and grades 3 or 4, 9% and 7%, respectively) and chronic GVHD and progression-free survival were similar between the 2 groups. However, TRM was lower in the group receiving haploidentical transplantation than in the group receiving UCB transplantations. This translated into improved 2-year survival.13 The GVHD prevention regimen for patients receiving haploidentical transplantations in these trials consisted of PTCy, tacrolimus, and MMF. A registry study comparing UCB with haploidentical transplantation after MAC showed lower incidence of acute GVHD, chronic GVHD, and TRM. The rates of grades 2-4 acute GVHD was 63% and 48% among patients receiving ≤5 of 8 and ≥6 of 8 HLA-matched cord blood units. The 3-year OS was similar.14
While reducing the incidence of GVHD, it is critical that the chosen regimen does not result in excessive immunosuppression with increased rates of infectious complications or impairment of graft-versus-disease effect leading to higher TRM or RR. The CAST regimen did not seem to negatively affect either. In this trial, tacrolimus was planned to be stopped by day +90. Previous reports have demonstrated the feasibility of shortened course of tacrolimus in 64% of patients receiving peripheral blood MUD or haploidentical transplants after NMA conditioning and PTCy, tacrolimus, and MMF for GVHD prophylaxis with acceptable safety profile.15 In our trial, the majority of patients (80%) were able to stop tacrolimus by day +90. This approach might have contributed to the prompt immune reconstitution. In fact, the recovery of T cells in our study compares favorably with what was observed in other studies using PTCy-based GVHD prevention regimens.12,16
The optimal duration of abatacept for GVHD prevention is yet to be determined. The terminal half-life of abatacept is 19.5 days. When patients received 4 doses during the first 30 days after transplantation, the mean peak serum level was 258 ± 9.3 μg/mL, whereas the maximum trough level dropped to 8.9 μg/mL by day +100.17 Because of the delayed median time to onset of acute GVHD in the first 28 patients receiving 3 doses of abatacept, the protocol was amended, adding a fourth dose on day +56 for the remaining 18 patients. Of these patients, none experienced grade 3-4 acute GVHD. The ongoing ABA3 trial should shed light on this question.
Moreover, the optimal dose of PTCy warrants further examination. Early data suggest that the daily dose of PTCy can be decreased to 25 mg/kg with reduced toxicity and accelerated engraftment without higher incidence of acute GVHD in patients receiving bone marrow grafts and PTCy in combination with sirolimus and MMF.18 A confirmatory trial is ongoing (NCT05436418). We have initiated a trial using the CAST combination and a reduction in the dose of PTCy (Re-CAST) after peripheral blood grafts (NCT05621759).
Limitations of our trial include its single-institution, nonrandomized design. Heterogeneity of the conditioning regimens and underlying malignancies limits the applicability of direct comparisons with similar trials.
Our study has met its primary end point in terms of reducing the incidence of grades 2-4 acute GVHD after haploidentical peripheral blood hematopoietic stem transplantation with excellent outcomes and therefore provides an impetus to compare CAST regimen with the standard approaches in a large, multi-institutional, randomized study, including in other settings such as in MMUD transplantations.
Acknowledgments
The study was supported, in part, by a grant from the Lisa Dean Moseley Foundation. J.D.G. and B.A.L. receive partial support from Cancer Center grant CA016087. The trial was not supported by any commercial entity.
Authorship
Contribution: A.S.A-H., K.C., and F.C. conceived the trial; J.D.G. and B.A.L. were the statisticians of the trial and performed the statistical analysis; all other authors contributed to the review of the data and writing of the manuscript and have responsibility of its content; and all authors had full access to the data and vouch the accuracy and completeness of the data and for the fidelity of the trial to the protocol.
Conflict-of-interest disclosure: A.S.A.-H. has received an educational grant from Bristol Myers Squibb and served as scientific advisory board member for Incyte. M.A.-H. has served as consultant for Jazz; a scientific advisory board member for Kite, Daiichi, Rigel, and Incyte; and speaker for Jazz, Takeda, and Servier. The remaining authors declare no competing financial interests.
Correspondence: A. Samer Al-Homsi, New York University Grossman School of Medicine, Transplant and Cellular Therapy, New York University Langone Health, 610 2nd Ave, New York, NY 10016; e-mail: samer.al-homsi@NYULangone.org.
References
Author notes
Partial results of this trial were presented in abstract form at the 62nd (Atlanta, 2021) and 63rd (New Orleans, 2022) annual meetings of the American Society of Hematology and the annual meeting of the American Society of Transplantation and Cellular Therapy (Orlando, 2023).
Deidentified participants data from the final research data set used in the manuscript will be shared upon reasonable request beginning from 9 months and ending at 36 months after publication, or as required by a condition of awards and agreements supporting the research, provided the investigators who proposes the use of the data executes a data use agreement with NYU Langone Health.
Data are available on request from the corresponding author, A. Samer Al-Homsi (samer.al-homsi@nyulangone.org).
The full-text version of this article contains a data supplement.