Key Points
IgD myeloma was historically associated with worse outcomes, but we now report a standard cytogenetic risk profile and survival outcomes.
Improved IgD myeloma survival is due to earlier diagnosis, improved supportive care, and response to novel antimyeloma therapies.
Abstract
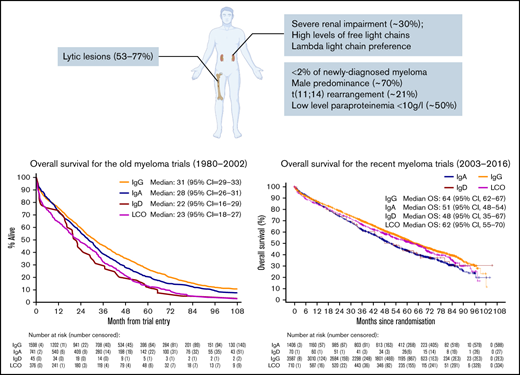
Immunoglobulin D (IgD) myeloma is a subtype often considered to have adverse features and inferior survival, but there is a paucity of data from large clinical studies. We compare the clinical characteristics and outcomes of patients with IgD myeloma from UK phase 3 myeloma trials analyzed in 2 groups: old (1980-2002) and recent (2002-2016) clinical trials, based on the time of adoption of novel myeloma therapies. Patients with IgD myeloma comprised 44 of 2789 (1.6%) and 70 of 5773 (1.2%) of the old and recent trials, respectively. Overall, IgD myeloma was associated with male predominance, low-level paraproteinemia (<10g/L), and λ light chain preference. The frequency of ultra-high-risk cytogenetics was similar in IgD myeloma compared with other subtypes (4.3% vs 5.3%, P > .99). Despite the old trial series being a younger group (median age: 59 vs 63 years, P = .015), there was a higher frequency of bone lesions, advanced stage at diagnosis, worse performance status, and severe renal impairment compared with the recent trials. Furthermore, the early mortality rate was significantly higher for the old trial series (20% vs 4%, P = .01). The overall response rate following induction therapy was significantly higher in the recent trials (89% vs 43%, P < .0001), and this was consistent with improved median overall survival (48 months; 95% confidence interval [CI] 35-67 months vs 22 months; 95% CI, 16-29 months). Survival outcomes for IgD myeloma have significantly improved and are now comparable to other myeloma types because of earlier diagnosis, novel therapies, and improved supportive care. This trial was registered at clinicaltrials.gov as # NCT01554852.
Introduction
Multiple myeloma, one of the leading causes of hematologic cancer–related morbidity and mortality, is characterized by an accumulation of monoclonal plasma cells in the bone marrow and usually a detectable monoclonal immunoglobulin (paraprotein or M-protein) in the serum.1,2 In contrast to the more common immunoglobulin G (IgG), IgA, and light chain only (LCO) myeloma subtypes, the paraprotein secreted is IgD in less than 2% of cases.3,4 IgD myeloma is biologically distinct from the common types of myeloma as it arises in a B cell before immunoglobulin class switching and as such may have a different clinical behavior. IgD myeloma has been described to be associated with a relatively young age at presentation, higher incidence of extramedullary involvement, osteolytic lesions, λ light chain predilection, renal failure, and advanced disease at diagnosis.5,6 Prior to the development of more sensitive diagnostic techniques such as immunofixation electrophoresis and the serum free light chain assay,7 the diagnosis of IgD myeloma was more likely to be missed because of the subtle M protein spike on conventional serum electrophoresis.8 Historically, IgD myeloma has been thought to be associated with a poor prognosis, but some recent studies have suggested comparable survival rates with other subtypes.9,10 As IgD myeloma is rare, the evidence base has been mostly limited to few small case series or other retrospective studies.
Over the last 2 decades, the management of myeloma has been transformed by the introduction of high-dose therapy with stem cell rescue, novel agents such as proteasome inhibitors, immunomodulatory agents (IMiDs), and monoclonal antibody therapies resulting in improved survival.11 Furthermore, improvements in supportive care may have also contributed to better outcomes.
The aims of this study were to identify the unique features of IgD myeloma in a large series of patients with myeloma and to compare outcomes between UK Medical Research Council (MRC) and National Cancer Research Institute (NCRI) myeloma clinical trials conducted before and after the introduction of novel therapies to determine their impact on IgD myeloma survival.
Patients and methods
Patient data
Patients with myeloma enrolled in the MRC UK myelomatosis IV, V, VI, VIII, IX, and XI clinical trials were considered for this study. For the purpose of this comparative analysis, 2 series were established: an “old trials” series comprising patients recruited in Myeloma IV, V, VI, and VIII trials, before the introduction of novel myeloma therapies, and the “recent trials” series, which included patients from Myeloma IX and XI. The Myeloma VII trial was not included because patients were randomized to receive intensive chemotherapy and stem cell rescue.12,13
In the old trials conducted between 1980 and 2002, patients were randomly assigned to receive either standard dose melphalan-based chemotherapy or melphalan-based conventional dose combination chemotherapy as exemplified by doxorubicin, carmustine, cyclophosphamide, and melphalan (ABCM). Details of these trials have previously been published.12,13
The two most recent trials, Myeloma IX and XI, accrued trial participants from 2003 to 2016. Myeloma IX was a multicenter, randomized, open-label, phase 3, and factorial design clinical trial conducted in the United Kingdom (International Standard Randomized Controlled Trial 68454111). The trial protocol details for Myeloma IX have been published previously.14,15 In summary, newly diagnosed patients aged 18 years or older with symptomatic multiple myeloma were allocated to either an intensive or nonintensive pathway. Details of the randomization strategy and treatment arms are summarized in supplemental Figure 1a-b. For the intensive pathway, oral cyclophosphamide, thalidomide, and dexamethasone was compared with infusional cyclophosphamide, vincristine, doxorubicin, and dexamethasone in patients with newly diagnosed multiple myeloma. For the nonintensive pathway, patients were randomized to either melphalan plus prednisolone or oral cyclophosphamide, thalidomide, and dexamethasone with a reduced dose of dexamethasone and lower starting dose of thalidomide. The exclusion criteria included pregnancy, asymptomatic myeloma, solitary bone or extramedullary plasmacytoma, previous or concurrent active malignancies, and presence of severe acute kidney injury unresponsive to up to 72 hours of rehydration, characterized by a serum or plasma creatinine > 500 μmol/L, a urine output less than 400 mL/day, or a requirement for dialysis.
The Myeloma XI trial (International Standard Randomized Controlled Trial 49407852) was a phase 3, randomized, multicenter, parallel group design, open-label trial comparing thalidomide, lenalidomide, carfilzomib, and bortezomib combinations and of lenalidomide (±vorinostat) as maintenance treatment in newly diagnosed patients with symptomatic myeloma 18 years and older.16,17 A summary of the randomization and treatment arms are shown in supplemental Figure 2a-b. The exclusion criteria were similar to those for the Myeloma IX trial.
Baseline clinical and biochemical characteristics were recorded for all patients at enrollment. Serum creatinine, β-2 microglobulin, paraprotein type and levels, and urine creatinine and light chain levels were measured by a central laboratory in Birmingham, UK. Participating centers provided clinical details, information on skeletal disease–related events, full blood count, serum albumin and urea, and plasma cell infiltration of bone marrow. Translocations t(4;14), t(14;16), and t(14;20) together with the copy number abnormalities del(17p), gain/amp(1q) have all been associated with adverse outcomes, and the presence of more than 1 adverse lesion is associated with even worse prognosis.18-20 Three cytogenetic risk groups were defined based on the number of adverse cytogenetic abnormalities identified at recruitment: ultra high risk (2 or more), high risk (1), and standard risk (0). Disease response and progression were defined according to trial protocol criteria, and a final report to ascertain the cause of death and a summary of the clinical course was recorded in the event of a death.
All trial protocols were approved by a multicenter research ethics committee and the relevant local ethics committees and institutional review boards. All patients gave written informed consent in accordance with the Declaration of Helsinki.
Differences in patient characteristics by paraprotein group were investigated using Pearson’s χ2 or Fisher’s exact tests. Overall survival (OS) was defined as the time between date of entry to either date of death or date last seen. Survival curves were constructed using the Kaplan-Meier method, and the log-rank test was used to assess differences between paraprotein class groups. Progression-free interval was calculated from date of recruitment to either the date of progression or censored at the date of death in patients who died progression free or censored at the date last seen for patients alive without progression. The date of data cutoff was 26 November 2021. Statistical analyses of the MRC trials were performed using SAS statistical software (SAS Institute, SAS Circle, Cary, NC).
Results
Baseline patient characteristics
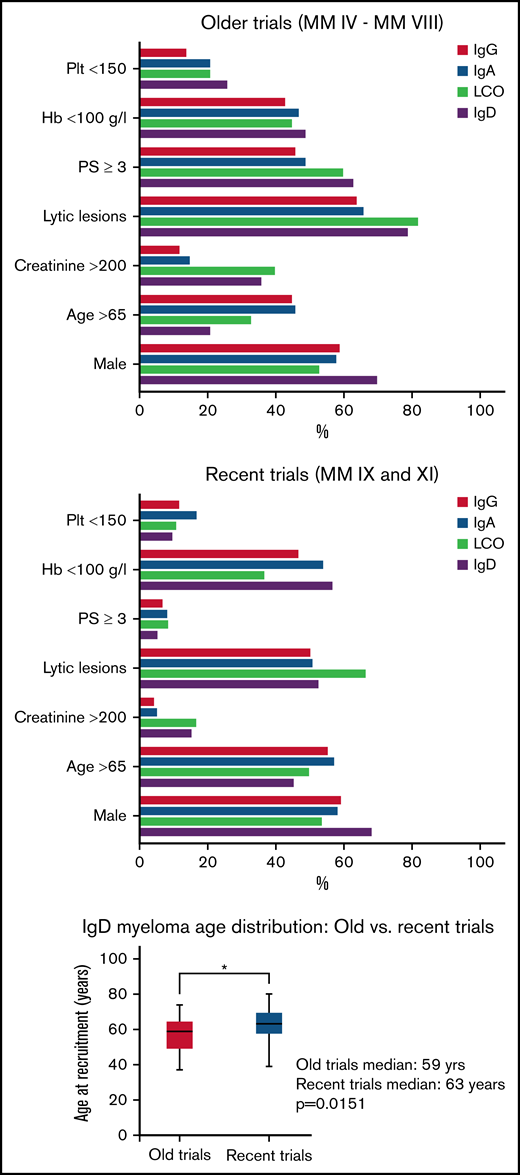
Forty-four patients with IgD myeloma were identified from the older Myeloma trials, accounting for approximately 2% of the 2789 total myeloma cases with an identifiable paraprotein (supplemental Table 1.1). The most common paraprotein type was IgG (56%), followed by IgA (26%) and LCO (12%). The median age of patients with IgD myeloma was 59 years (Figure 1), and 20% were 65 years or older at the time of diagnosis (Table 1). In this series, most patients with IgD myeloma (61%) had a performance status of 3 or more, and this was comparable to light chain only myeloma (60%). IgD and LCO myeloma were also similar in rates of elevated serum β2-microglobulin levels. Significant renal impairment, as indicated by elevated serum creatinine and urea, were highest in LCO and IgD myeloma but more marked for the former (supplemental Table 1.2). Severe anemia (<7.5 g/dL) was most frequently observed in patients with IgD myeloma, perhaps reflecting higher bone marrow involvement as half of these patients had bone marrow plasma cells greater than 50%. Hypercalcemia was more common in IgA myeloma (45%). There were, however, fewer lytic bone lesions in IgA myeloma compared with IgD and LCO myeloma, which had the highest rates (supplemental Table 1.2). There was no significant difference in bone pain and fractures across all groups.
Comparison of baseline patient characteristics for the myeloma subsets across UK MRC/NCRI clinical trials. Plt, platelet count; Hb, hemoglobin concentration; PS, performance status; LCO, light chain only myeloma. The box and whisker plot compares the ages of patients with IgD myeloma in the respective trials. Box indicates median and interquartile range; whiskers indicate range.
Comparison of baseline patient characteristics for the myeloma subsets across UK MRC/NCRI clinical trials. Plt, platelet count; Hb, hemoglobin concentration; PS, performance status; LCO, light chain only myeloma. The box and whisker plot compares the ages of patients with IgD myeloma in the respective trials. Box indicates median and interquartile range; whiskers indicate range.
Seventy patients with IgD myeloma were recruited into the recent trials accounting for 1.2% of the 5773 total. As observed in the old trials, rates of severe renal impairment were higher in IgD and LCO myeloma subgroups in the recent trials (Figure 1; supplemental Tables 1.2 and 1.3), but this was considerably less compared with the old trials. Both IgD myeloma series were similar in λ light chain preference, higher male prevalence, and low-level paraproteinemia, but the old trials series had significantly worse performance status, advanced International Staging System (ISS) stage, higher serum β2-microglobulin levels, severe renal impairment, and more frequent lytic lesions at diagnosis despite the recent trial series being older (median age, 59 vs 63 years; P = .015; Table 1; Figure 1). In the recent trials, 73% of patients with IgD myeloma were allocated to the intensive arms.
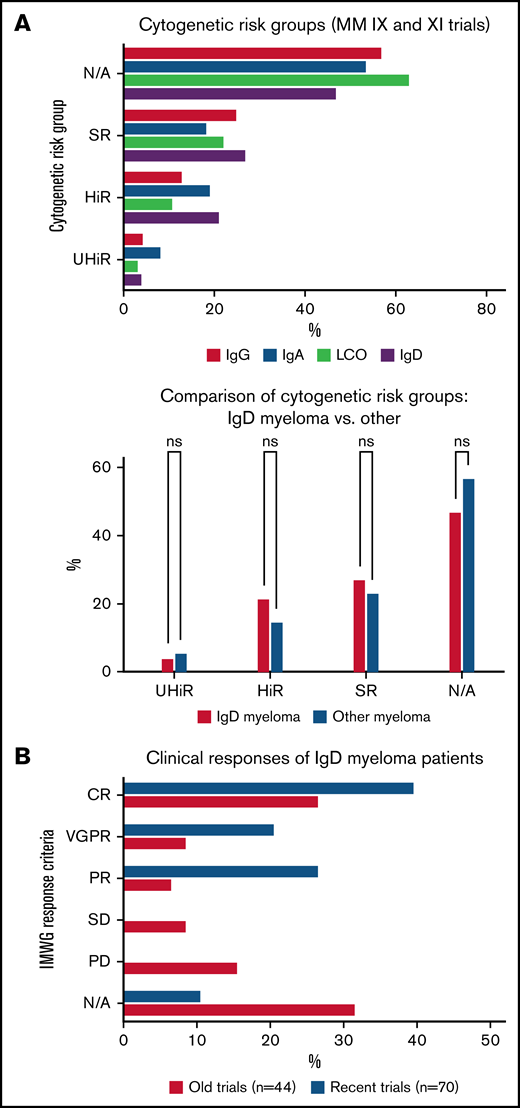
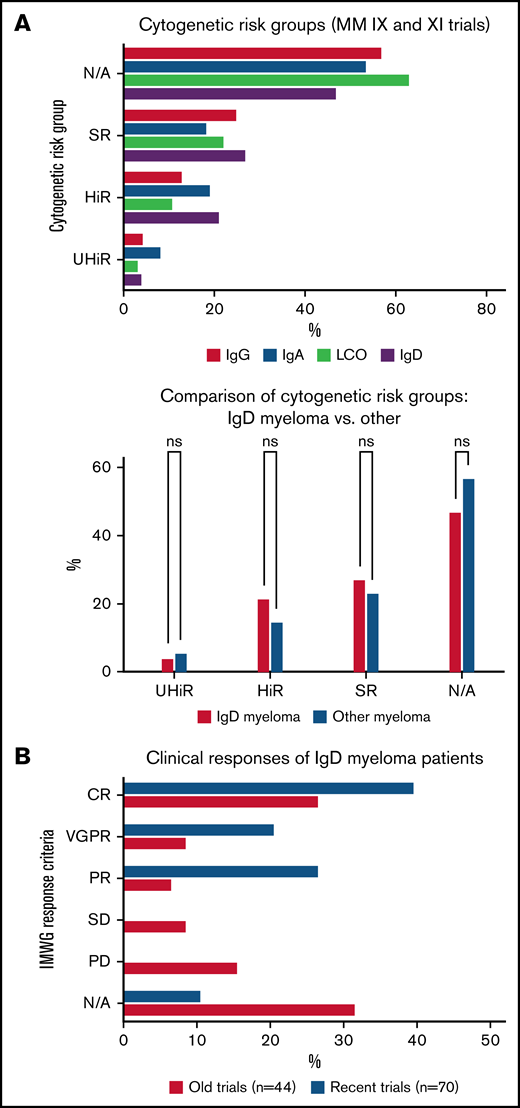
Patients with IgD myeloma in the recent trials had a similar distribution of the cytogenetic risk groups compared with other myeloma subtypes (Figure 2A), with 3 (4.3%) of these patients identified as ultra-high risk at diagnosis. There was an overrepresentation of ultra-high risk cytogenetics in the IgA myeloma group compared with the other subtypes (8.4% vs 5.3%, P < .0001; supplemental Table 2). The t11,14 chromosomal rearrangement was assessed at diagnosis in 28 patients with IgD myeloma, and this cytogenetic abnormality was present in 6 (21%) compared with 95 (11%) of 838 patients with IgG and 207 (15%) of 1339 patients with non-IgD myeloma (supplemental Tables 5 and 6).
Frequency of cytogenetic risk groups and clinical responses for IgD myeloma. (Ai) Cytogenetic risk stratification of participants in the recent UK myeloma clinical trials (Myeloma IX and XI). Graph shows the percentage of the cytogenetic risk groups for the various myeloma subtypes. (Aii) Comparison proportions of the cytogenetic risk groups for IgD myeloma vs other myeloma subtypes. UHiR, ultra high risk; HiR, high risk; SR, standard risk; N/A, not available. (B) Clinical responses following induction therapy based on the IMWG response criteria. CR, complete response; VGPR, very good partial response; PR, partial response; SD; stable disease; PD, persistent disease; N/A, not available.
Frequency of cytogenetic risk groups and clinical responses for IgD myeloma. (Ai) Cytogenetic risk stratification of participants in the recent UK myeloma clinical trials (Myeloma IX and XI). Graph shows the percentage of the cytogenetic risk groups for the various myeloma subtypes. (Aii) Comparison proportions of the cytogenetic risk groups for IgD myeloma vs other myeloma subtypes. UHiR, ultra high risk; HiR, high risk; SR, standard risk; N/A, not available. (B) Clinical responses following induction therapy based on the IMWG response criteria. CR, complete response; VGPR, very good partial response; PR, partial response; SD; stable disease; PD, persistent disease; N/A, not available.
Clinical responses after induction therapy
Comparison of induction response rates among patients with IgD myeloma between the old and recent clinical trial series showed significant improvements in overall response rates (43% vs 89%, P < .0001; Figure 2B). There was a similar trend toward deeper remissions in the participants with IgD myeloma in the recent trials: complete response rate was 40% vs 27% (P = .23; supplemental Table 4).
Survival outcomes
In the old trials, patients with IgD myeloma had the shortest median OS of 22 months (95% confidence interval [CI]: 16-29 months), and this was similar for LCO myeloma (median, 23 months; 95% CI: 18-27 months; Figure 3A). The longest median OS was observed in patients with IgG myeloma (median: 31 months; 95% CI: 29-33 months), whereas that for IgA myeloma was 28 months (95% CI: 26-31 months). Similarly, the median progression-free survival (PFS) was longest for IgG myeloma (21 months; 95% CI: 20-22) and shortest for IgD myeloma (16 months; 95% CI, 13-20; P < .0001; Figure 3B). A significantly higher early death rate, within 100 days of trial entry, was observed for patients with IgD myeloma compared with IgG/IgA (20% vs 14%, respectively; P < .001).
Old myeloma trials. (A) Overall survival of patients with myeloma stratified by paraprotein type. (B) Progression-free survival of patients with myeloma stratified by paraprotein type.
Old myeloma trials. (A) Overall survival of patients with myeloma stratified by paraprotein type. (B) Progression-free survival of patients with myeloma stratified by paraprotein type.
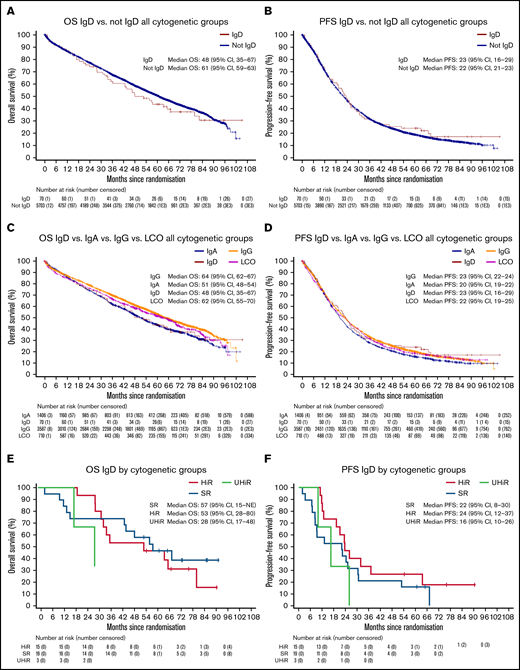
In the pooled analysis of the recent trials, the median OS for IgD myeloma was 48 months (95% CI: 35-67 months) compared with 61 months (95% CI: 59-63 months) for the other subtypes combined (Figure 4A). This difference was not statistically significant (P = .466; hazard ratio [HR], 0.89; 95% CI: 0.66-1.21). There was also no significant difference in median PFS between IgD myeloma and other subtypes; 23 vs 22 months, respectively (P = .522; HR, 1.09; 95% CI: 0.84-1.42; Figure 4B). Direct comparison of OS between specific myeloma subtypes showed that IgG and LCO myeloma had the longest median OS (Figure 4C) at 64 (95% CI: 62-67 months) and 62 months (95% CI: 55-70 months), respectively. The median OS for IgA myeloma was 51 months (95% CI, 48-54 months). PFS was similar for all patients, irrespective of paraprotein type (Figure 4D).
Recent myeloma trials. (A) Kaplan-Meier plot comparing overall survival between IgD myeloma and other subtypes. (B) Kaplan-Meier plot comparing progression-free survival between IgD myeloma and other subtypes. (C) Kaplan-Meier plot of overall survival stratified by paraprotein class. (D) Kaplan-Meier plot of progression-free survival stratified by paraprotein class. (E) Overall survival of patients with IgD myeloma stratified by cytogenetic risk group. (F) Progression-free survival of patients with IgD myeloma stratified by cytogenetic risk group.
Recent myeloma trials. (A) Kaplan-Meier plot comparing overall survival between IgD myeloma and other subtypes. (B) Kaplan-Meier plot comparing progression-free survival between IgD myeloma and other subtypes. (C) Kaplan-Meier plot of overall survival stratified by paraprotein class. (D) Kaplan-Meier plot of progression-free survival stratified by paraprotein class. (E) Overall survival of patients with IgD myeloma stratified by cytogenetic risk group. (F) Progression-free survival of patients with IgD myeloma stratified by cytogenetic risk group.
To evaluate the influence of cytogenetics on survival, a stratified analysis was performed for the recent trial series. The frequency of standard, high, and ultra high risk cytogenetics groups were similar between IgD and IgG myeloma, but the frequency of ultra-high risk cytogenetics was higher for IgA myeloma compared with IgG (8.4% vs 4.5%, P < .0001; supplemental Table 2). The median OS and PFS for IgD myeloma was comparable with those of other subtypes within each of the 3 cytogenetic risk groups (supplemental Figure 3a-b). The median OS values for IgD myeloma subcategories were 57 months (95% CI: 15-not evaluable), 53 months (95% CI: 28-80), and 28 months (95% CI: 17-48), respectively, for standard, high, and ultra-high cytogenetic risk groups (Figure 4E). The median PFS was shortest in the ultra-high-risk group (16 months; 95% CI: 10-26) and longest in the high-risk group (24 months; 95% CI: 12-37; Figure 4F).
Mortality data
At the time of data cutoff, 44 and 43 deaths had been recorded among patients with IgD myeloma in the old and recent trial, respectively (Table 2), with disease progression being the main cause of mortality in both groups. A significantly higher rate of early mortality, within 100 days of trial entry, was observed in the old trials IgD myeloma group (20% vs 4%, P = .01). Similar rates of deaths caused by renal failure and cardiorespiratory disease were observed between the 2 groups. Interestingly, infection was more commonly recorded as the cause of death in the recent trial series (2% vs 19%, P = .01).
Discussion
Given the rarity of IgD myeloma, there are only few published studies on the clinical characteristics and outcomes of the disease. This study reports the largest set of patients with IgD myeloma from randomized clinical trials. Most previously published IgD myeloma studies have been retrospective case series, registry data, or single-center reports, and some of these are summarized in Table 3. One of the strengths of this study is the fact that the diagnostic and follow-up laboratory samples were analyzed in a central laboratory, thus permitting direct comparability between the patient groups in our study.
Previous studies have reported associations of IgD myeloma with male sex, younger age at diagnosis, hypercalcaemia, higher serum β2-microglobulin and creatinine, λ light chain predilection, amyloidosis, and a greater degree of bone involvement.21-24 Some associations such as higher frequency of male patients, younger median age, and λ light chain predilection were also observed in this study. However, despite being an older group, patients with IgD myeloma in the recent trials had less renal impairment and hypercalcemia, better performance status, and earlier ISS stage at diagnosis compared with the old trials group. The most plausible explanation for this observation would be earlier diagnosis permitted by the introduction of sensitive diagnostic techniques such as the serum free light chain assay. Interestingly, we also found striking similarities in baseline characteristics between IgD and LCO myeloma, possibly reflecting the diagnostic challenge posed by the lack of a characteristic monoclonal protein spike on conventional electrophoresis for both myeloma subtypes. Possibly because of the difficulty with establishing the diagnosis of IgD myeloma before the introduction of more sensitive diagnostic methods such as the serum-free light chain assay, patients were at an advanced stage with a higher disease burden as observed in the old trials. Consequently, the lesser degree of severe renal impairment observed in the recent trials compared with the older trials may also reflect the improved management of renal complications. The most striking evidence for this can be seen in the marked improvement in the median overall survival of LCO myeloma between the 2 series (23 vs 62 months). A recently published analysis of outcomes of patients from the Myeloma XI trial by baseline renal function showed that severe renal impairment was associated with inferior survival and recovery of renal function postinduction treatment was associated with younger age (<70 years), a higher baseline free light chain level > 1000 mg/L, and/or a free light chain response of >90%.17 Therefore, the improved renal profiles of the recent trials group would have made a significant contribution to the improvements in survival outcomes of patients with IgD myeloma.
Despite the patients with IgD in the old trial series being younger, this group had a worse baseline performance status and ISS stage, correlating with inferior survival outcomes for this group. Comparison of OS for IgD myeloma across the trials indicates a significant improvement in median survival from 22 months (95% CI: 16-29 months) for the old trials series to 48 months (95% CI: 35-67 months) in the recent trials. A similar improvement in progression-free survival was observed (16 months; 95% CI: 13-20 vs 23 months, 95% CI: 16-29). As the recent trials were conducted in the era of IMiDs and proteasome inhibitors, it is likely that the improvement in outcomes, particularly the PFS, is attributable to these novel therapies. Interestingly, of all the myeloma subtypes, IgD myeloma has seen the largest improvement in PFS between the 2 series. A similar improvement in IgD myeloma survival has been reported by the Greek Myeloma Study Group for patients treated from 2000 to 2012 compared with those treated before 2000 (44 vs 51.5 months, P = .018), the time point when the first IMiD became available.9 Furthermore, a consistent improvement in median OS is apparent from published IgD myeloma studies over the years (Table 3). One of the earliest case series of IgD myeloma in Japanese patients published in 1991,25 well before the introduction of novel antimyeloma agents, reported a median OS of 12 months in contrast to a recently published multicentre retrospective Asian Myeloma Network (AMN) study involving patients with IgD myeloma from China, Korea, and Singapore that reported a median OS of 36.5 months for the entire IgD myeloma cohort.26 There was an unusually high prevalence of IgD myeloma (2%-8.8%) in the study population with a higher frequency of t11,14 chromosomal rearrangement in the IgD myeloma cohort compared with other myeloma subtypes (24.7% of IgD MM vs 13.5% of non-IgD MM). Similarly in our recent trials series, the frequency of t11,14 in IgD myeloma was approximately twice that of the IgG subtype. This increased frequency of t11,14 in IgD myeloma warrants further study because of the therapeutic potential of BCL-2 inhibitors in this group of patients.
Furthermore, IgD myeloma was not associated with a higher rate of adverse cytogenetics compared with other subtypes; however, we observed an increased frequency of the ultra-high risk cytogenetic profile in IgA myeloma, correlating with a relatively shorter OS compared with IgG myeloma (Figure 4C). Other studies have similarly reported higher frequencies of adverse risk cytogenetics such as t4,14 in patients with IgA myeloma with resulting poorer outcomes compared with IgG myeloma.27-29 Furthermore, the significant difference in median OS between IgG and IgA myeloma in our study is not seen within the ultra-high risk cytogenetics subgroup that has a uniformly inferior outcome (IgA, 33 months, 95% CI: 26-40 vs IgG, 29 months, 95% CI: 22-36; supplemental Figure 4). These observations support the use of cytogenetic risk stratification rather than paraprotein type in assigning prognostic categories in myeloma.
The impact of novel therapies on the outcomes of IgD myeloma could also be deduced from the clinical response rates between the old and recent trial series as the overall response rate was significantly higher in the recent trials (89% vs 43%, P < .0001) with a trend toward deeper remissions (CR and VGPR). In a study conducted in the prenovel therapy era, Morris et al previously reported significantly higher complete response rate in patients with IgD myeloma compared with the more common myelomas (43.8% vs 23.2%) but an inferior OS (43.5 vs 63.2 months, P < .0001) suggesting a high relapse rate in this patient group.22 Similar findings were reported in a smaller study of 77 patients with myeloma undergoing autologous stem cell transplant in Korea; despite significantly higher complete response rates after autologous stem cell transplant (75% vs 58%), patients with IgD myeloma had much worse event-free (6.9 vs 11.5 months, P = .01) and OS (12 vs 55.5 months, P < .01) compared with other myeloma subtypes.30 It is noteworthy that the majority of patients in this study received conventional chemotherapy regimens as opposed to novel agents. Given the improvements in IgD PFS in our recent trial series, it is possible to conclude that novel agents have improved both the depth and duration of clinical responses in patients with IgD myeloma.
In the current study, the most frequent cause of death for both IgD myeloma series was disease progression, with a significantly higher rate of early mortality in the old trials, which is likely because of a combination of factors notably severe renal impairment and advanced disease stage. An explanation for the higher rate of infections reported as a cause of death in the recent trials series is likely a result of longer survival and the impact of multiple lines of therapy.
One of the limitations of this study has been the relatively limited number of patients with IgD myeloma that made comparison with the other more common myeloma subtypes statistically challenging. Furthermore, cytogenetics results were not available for the old trials for comparison with the available data from the recent trials. The exclusion of patients with end-stage renal impairment from the clinical trials limits the extrapolation of the findings to this population, but as the comparison of outcomes was between 2 clinical trial series with similar inclusion and exclusion criteria, apart from the age limit of 75 years for the older trials, the observed differences in outcomes are not likely to be attributable to selection bias. Furthermore, the central analysis of the OPTIMAL and MERIT trials of patients with newly diagnosed myeloma in the United Kingdom presenting with severe renal impairment reported comparable proportions of IgD myeloma, indicating that significant patients with IgD myeloma were not being missed by exclusion of patients with end-stage renal failure from the clinical trials analyzed in this publication.31
To our knowledge, this is the first study specifically reporting the characteristics and outcomes of IgD myeloma from large phase 3 randomized clinical trials. Our data suggest that with improved diagnostic tests permitting earlier diagnosis and the introduction of novel antimyeloma agents, OS and PFS of IgD myeloma is now comparable to other myeloma subtypes. We argue that the historical association of IgD myeloma with a dismal prognosis was largely because of renal impairment and advanced stage, possibly linked to delays in establishing the diagnosis. Our data also underline the importance of cytogenetic risk stratification as patients with adverse cytogenetic profiles had poorer outcomes irrespective of the myeloma subtype and that IgD myeloma was not associated with a higher rate of adverse cytogenetics. Therefore, in the era of novel myeloma therapies, cytogenetic risk stratification is of greater prognostic value than paraprotein type.
Acknowledgments
The authors appreciate all the clinical trial investigators across the participating hospitals in the United Kingdom and particularly the trial participants.
Authorship
Contribution: C.A. prepared the original draft, created methodology, and performed data curation and analysis; G.I. reviewed and edited the manuscript, and performed data curation for the old trials series, analysis, and validation; D.C. performed data curation for the recent trials and reviewed and edited the manuscript; T.M. reviewed and edited the manuscript and performed data curation, analysis, and validation of the recent trials; J.D., W.G., M.K., R.O., C.P., J.A.C., F.D., G.J.M., and G.H.J. reviewed and edited the manuscript; and M.T.D. and S.B. supervised the study, participated in conceptualization, created methodology, performed data validation, and reviewed and edited the manuscript.
Conflict-of-interest disclosure: D.C., T.M., and W.G. received research funding from Celgene Corporation, Amgen, Merck Sharp, and Dohme. M.K. has consulted for Abbvie, consulted for and received honoraria from Amgen, consulted for and received honoraria, research support, and travel support from BMS/Celgene, consulted for and received honoraria and travel support from Janssen, consulted for GSK, consulted for Karyopharm, consulted for Pfizer, consulted for Seattle Genetics, and consulted for and received honoraria and travel support from Takeda. C.P. received consulting fees, honoraria, and travel support from Amgen, Celgene Corporation, Janssen, Sanofi, and Takeda Oncology. G.J.M. received consultancy fees, honoraria, and travel support from Amgen, Celgene Corporation, Janssen, Sanofi, and Takeda Oncology. G.H.J. received research funding from Takeda and Celgene/BMS and honoraria for speaking from Takeda, Celgene/BMS, Amgen, Janssen, Sanofi, and Oncopeptides. M.T.D. owns stock in Abbingdon Health. S.B. is on the ad board for Sanofi, Pfizer, and Bristol Myers Squibb. The remaining authors declare no competing financial interests.
Correspondence: Charles Agbuduwe, UCL Cancer Institute, 72 Huntley St, London, WC1E 6DD and UCL Great Ormond Street Institute of Child Health, University College London, London, United Kingdom; e-mail: c.agbuduwe@ucl.ac.uk.
References
Author notes
Contact the corresponding author for data sharing at c.agbuduwe@ucl.ac.uk.
The full-text version of this article contains a data supplement.