Key Points
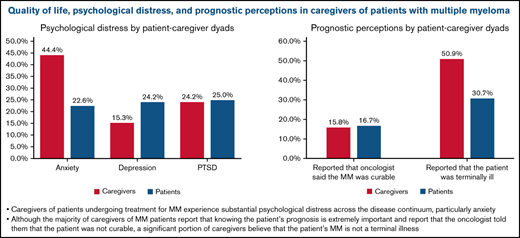
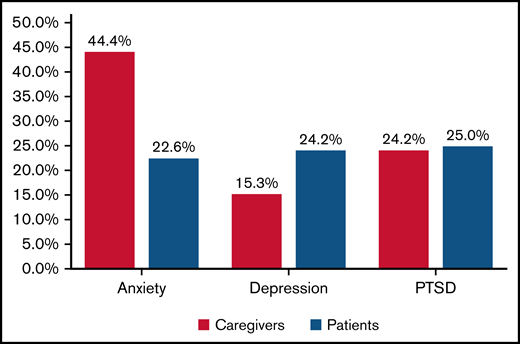
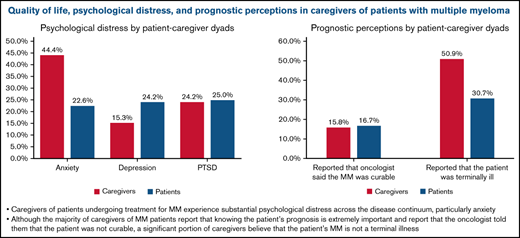
Caregivers of patients treated for MM experience substantial psychological distress across the disease continuum, particularly anxiety.
The majority of caregivers report the oncologist told them the patient’s MM was incurable, yet a large portion believe the patient curable.
Abstract
Although caregivers of patients with multiple myeloma (MM) play a critical role in supporting their loved ones throughout the illness course, studies examining caregiver quality of life (QOL), psychological distress, and prognostic awareness are lacking. We conducted a cross-sectional, multisite study of patients undergoing treatment with MM and their caregivers. Eligible caregivers were enrolled to 1 of 3 cohorts based on lines of therapy. Caregivers completed validated questionnaires to assess their QOL, psychological distress, and perceptions of prognosis. We enrolled 127 caregivers of patients with MM (newly diagnosed [n = 43], 2-3 lines of therapy [n = 40], and ≥4 lines of therapy [n = 44]). Caregiver QOL and psychological distress did not differ by line of therapy. The rate of clinically significant anxiety, depression, and posttraumatic stress disorder symptoms were 44.1% (56/127), 15.8% (20/127), and 24.4% (31/127), respectively. When examined in dyads, caregivers reported higher rates of clinically significant anxiety (44.4% [55/124] vs 22.5% [28/124]) compared with patients with MM. Most caregivers (84.2%, 101/120) reported that the oncologist had informed them that the patient’s cancer was incurable; however, only 50.9% (58/114) and 53.6% (59/110) of caregivers acknowledged the patient’s cancer was terminal and incurable, respectively. Caregivers of patients undergoing treatment for MM experience substantial psychological distress across the disease continuum, particularly anxiety. The majority of caregivers of patients with MM report that knowing the patient’s prognosis is extremely important and report that the oncologist told them that the patient was incurable. Nevertheless, a significant portion of caregivers believe that the patient’s MM is curable.
Introduction
Multiple myeloma (MM) is the second most common hematologic malignancy affecting primarily older adults with a median age of 70 years.1 Advances over the past 15 years have contributed to the availability of effective therapies that have modified the treatment paradigm for MM such that patients are now treated continuously for their disease. Notably, these medications have led to significant improvements in patients’ overall survival; the 5-year relative survival is 55.6%.2 Despite the remarkable therapeutic advances, little is known about the quality of life (QOL) and lived experiences of patients with MM and their caregivers throughout the illness continuum. Due to the long-term nature of MM therapy, patients and caregivers often dedicate a significant proportion of their time to management of the disease,3 which may impact QOL and psychological well-being. Long-term therapy may also have downstream effects, including caregiver burden. Caregivers assume their role as the primary caretaker of patients with limited preparation and often are not provided consistent support throughout the duration of treatment.4
Recognizing the profound impact that cancer therapy may have on caregivers, several studies have reported that caregivers often experience higher levels of psychological distress and greater impairments in QOL than patients themselves.5,6 In a cross-sectional survey assessing the unmet needs and QOL of patients with MM and their partners, over one-fourth (26.5%) of patients reported at least 1 unmet need.7 Notably, caregivers of patients with MM reported several unmet needs that are distinct from the needs of patients, including information on the management of side effects experienced by patients and the availability of local healthcare services. These studies reinforce the demand for supportive care interventions tailored to both patients with MM and their caregivers. However, data assessing the effect of MM therapy on caregivers remain limited. To our knowledge, no published studies have measured caregiver QOL and psychological distress over the course of MM therapy. There exists an important gap in our understanding of caregiver QOL and burden during MM therapy.
Deficits in patients’ and caregivers’ prognostic perceptions may have important implications for informed decision making, especially when it comes to their end-of-life care. Previous studies have reported that patients with incurable cancers and their families desire timely and realistic prognostic information.8,9 When caregivers have an accurate understanding about prognosis, they are better positioned to help patients cope with their prognosis, participate in conversations related to goals of care, advocate for patients’ best interests, anticipate the outcome of terminal illness, and make informed decisions.10-14 Thus, understanding caregiver prognostic perceptions may play an important role in informed decision making across the disease continuum, and particularly during end-of-life care in MM. Yet, little is actually known about caregivers’ prognostic perceptions in MM.
In this study, we first describe the QOL and psychological distress of caregivers of patients with MM by lines of therapy to better appreciate the experience of the caregivers across the MM disease trajectory. We also examine caregivers’ preferences for prognostic information and their prognostic perceptions. Understanding the lived experience of caregivers of patients with MM will help identify opportunities for intervention that may improve the overall QOL and care of this population.
Methods
Participants
We conducted a prospective, cross-sectional, multisite study within the Dana-Farber/Harvard Cancer Center network between June 2020 and January 2021. We included 180 patients receiving treatment for MM and 127 of their caregivers. Data on patients is currently in press.15 This manuscript focuses on caregiver outcomes. Caregivers enrolled in the study were English-speaking adults. To capture the full spectrum of the experience of caregivers of patients with MM, we recruited up to 60 consecutive caregivers to 1 of 3 cohorts based on line of therapy. Specifically, we enrolled caregivers of patients in the following cohorts: newly diagnosed receiving first-line therapy (prior to autologous stem cell transplant), receiving 2 to 3 lines of therapy, and receiving ≥4 lines of therapy. The 3 cohorts were chosen based on conventions around study populations in clinical trials of MM therapies and were used for the patient study. Caregivers included either a relative or friend whom the patient identified as living with them or having in-person contact with him or her at least twice per week.
Study design and procedures
This study was approved by the DF/HCC Institutional Review Board. We identified eligible patients and their caregivers by screening weekly MM clinic schedules. Patients were asked to identify a caregiver who may be interested in participating. Informed consent was obtained from caregivers either in-person at the patient’s scheduled clinic visit or over the telephone through verbal consent. Caregivers completed baseline self-report assessments within 1 week of obtaining informed consent.
Study measures
Demographic and clinical factors.
Caregivers completed a demographic questionnaire at the time of baseline data collection detailing their age, sex, race, ethnicity, religion, relationship status with the patient, education level, annual household income, and living situation.
QoL.
To measure QOL, we used the CareGiver Oncology QOL questionnaire. The CareGiver Oncology QOL questionnaire is a 29-item instrument to measure QOL in multiple domains and has been previously validated for caregivers of patients with cancer, including hematologic malignancies.16,17 Higher total scores indicate better QOL.
Psychological distress.
We used the Hospital Anxiety and Depression Scale to assess symptoms of anxiety and depression in caregivers.18,19 The Hospital Anxiety and Depression Scale is a 14-item questionnaire that contains 2 7-item subscales assessing depression and anxiety symptoms during the past week. Scores on each subscale range from 0 to 21, with a cutoff of ≥8 denoting clinically significant anxiety or depression. To assess symptoms of posttraumatic stress disorder (PTSD), we used the Posttraumatic Stress Disorder Checklist (PCL), a 17-item self-reported measure that evaluates symptoms of posttraumatic stress, with higher scores indicating worse PTSD symptoms.20 A cutoff of ≥33 denoting clinically significant PTSD.
Perceptions of prognosis.
We used the Perception of Treatment and Prognosis questionnaire (PTPQ) to assess caregivers’ perceptions of their prognosis. The PTPQ was used to assess (1) preferences for information about treatment and goals of therapy, (2) the importance of knowing about prognosis, and (3) likelihood of cure.13,21
To assess caregivers’ perception of prognosis, we used 3 items from the PTPQ. We asked caregivers to rate the likelihood that their loved ones will be cured of their cancer on a 7-point scale. We dichotomized responses into a low likelihood of cure (defined as “no chance—0% chance of cure” and “very unlikely—less than 10% chance of cure”) vs all other responses (including unlikely cure [10%-24% chance of cure] and likely cure [25% to >90% chance of cure]) as done in prior studies.13,22 We then asked caregivers if the oncologists has said that their loved ones’ cancer was curable (“yes” vs “no”). Finally, we asked participants to rate their loved ones’ current medical status with regard to current health and terminal illness using a validated 4-item scale that has been used extensively in prior studies.13,23 We dichotomized the responses as either “terminally ill” or “not terminally ill.”
Statistical analysis
We used descriptive statistics to characterize caregiver demographics, QOL, symptom burden, psychological distress, and perceptions of prognosis overall and by line of therapy. To assess the association between lines of therapy with caregiver-reported QOL, psychological distress, and perception of prognosis, we used unadjusted linear and logistic regression models for continuous and dichotomous outcomes, respectively, and examined lines of therapy as a predictor of these outcomes. We then used multivariate regression models adjusting for age, sex, race, and education when examining the relationship between lines of therapy and these outcomes. To describe the rates of clinically significant mood symptoms, we dichotomized scores on these instruments using their standard cutoffs with categories reflecting the presence of absence of clinically meaningful mood symptoms.
We then explored the relationship between caregivers’ perception of their patients’ prognosis with their QOL and psychological distress using linear regression models. Specifically, we examined whether caregivers report that their oncologist told them their patient’s cancer was incurable, and caregiver acknowledgment of their patient’s terminal illness was associated with caregiver-reported QOL and psychological distress. Given the potential for collinearity between QOL and psychological distress, we modeled these outcomes separately.
Psychological distress and perception of prognosis between patient-caregiver dyads were descriptively compared given the limited sample size. We used correlation coefficients to explore the concordance between patient and caregiver psychological distress.
Results
Participant characteristics
We identified a total of 156 potential caregivers to achieve a sample size of 127 caregivers (enrollment rate, 81.4%) (Figure 1). We enrolled 127 caregivers to the following groups: newly diagnosed (n = 43), 2 to 3 lines of therapy (n = 40), and ≥4 lines of therapy (n = 44) from 3 sites between June 2020 and January 2021. None of the newly diagnosed patients had undergone transplant, and 43.3% (26/60) of patients receiving 2 to 3 lines of therapy and 61.7% (37/60) of patients receiving ≥4 lines of therapy had undergone an autologous stem cell transplant. The median caregiver age was 61.8 years (range, 24.0-81.9), and 71.7% (91/127) were female. The majority (68.5% [87/127]) of caregivers were spouses/partners, and 18.9% (24/127) identified as the child of the patient (Table 1).
Flow diagram of caregiver recruitment. MGH, Massachusetts General Hospital.
Caregiver QOL and psychological distress
Caregiver QOL did not differ by line of therapy: QOL 74.5 (standard deviation [SD], 12.7) vs 73.2 (SD, 13.3) and 71.7 (SD, 14.7).
Caregiver psychological distress also did not differ by line of therapy. In multivariate regression models controlling for age, sex, and education, line of therapy was not associated with caregiver QOL or psychological distress. The rates of clinically significant anxiety, depression, and PTSD symptoms were 44.1% (56/127), 15.7% (20/127), and 24.4% (31/127), respectively.
In unadjusted analyses, caregiver sex, employment, education level, or patient’s receipt of transplantation were not associated with caregiver QOL or psychological distress. Older caregiver age was associated with better caregiver QOL (B = 0.24; 95% CI, 0.05, 0.43; P = .014) but not their psychological distress.
Information preferences
Overall, 89.6% (112/125) of caregivers reported that it is “extremely” or “very” important to know about the patient’s prognosis, and 55.6% (70/126) stated that they had received adequate information regarding the patient’s prognosis. Caregivers reported that prognostic information was “extremely” or “very” helpful in making decisions about treatment (94.0%, 109/116), preparing for the future (88.6%, 101/114), and coping with the disease (85.2%, 98/115) (Table 2).
Prognostic understanding and treatment goals
Most caregivers (84.2%, 101/120) reported that the oncologist had told them the patient’s cancer was incurable. However, only 50.9% (58/114) of caregivers acknowledged that the patient was terminally ill, and 53.6% (59/110) reported that they thought the patient’s cancer was incurable.
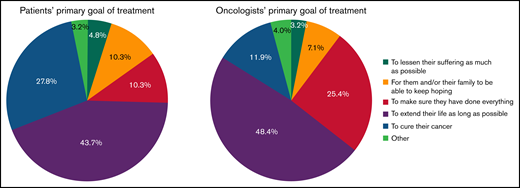
With regard to treatment goals, nearly 27.8% (35/126) of all caregivers reported that their primary goal of therapy was cure, and 11.9% (15/126) reported that their oncologist’s primary goal was cure (Figure 2). There were no differences in caregiver report that the cancer was incurable by line of therapy.
Caregiver perceptions of patient’s goals of treatment and oncologist’s goals of treatment.
Caregiver perceptions of patient’s goals of treatment and oncologist’s goals of treatment.
Association of caregivers’ perception of prognosis with their QOL and psychological distress
Caregiver report that the oncologist said that the patient was incurable was not associated with worse QOL (B = 0.545, P = .876), anxiety (B = −0.590, P = .567), depression (B = −0.473, P = .42), or PTSD symptoms (B = −3.74, P = .169). Caregiver acknowledgment of terminal illness was not associated with worse QOL (B = −3.76, P = .146), depression (B = 0.325, P = .59), or PTSD symptoms (B = −0.839, P = .678). However, caregiver acknowledgment of terminal illness was associated with higher anxiety (B = 1.51, P = .046).
Patient-caregiver dyads.
Psychological distress and prognostic perceptions were then evaluated in patient-caregiver dyads descriptively. When examining dyads, caregivers reported higher rates of clinically significant anxiety symptoms (44.4% [55/124] vs 22.6% [28/124]) compared with patients with MM (Figure 3). Caregivers reported fewer clinically significant depression symptoms (15.3% [19/124] vs 24.2% [30/124]) and similar rates of PTSD symptoms (24.2% [30/124] vs 25.0% [31/124]). There was a small positive correlation between patient and caregiver psychological distress (anxiety, r = 0.26; depression, r = 0.17; PTSD, r = 0.13). Caregivers were more likely than patients to report that the patient was terminally ill (50.9% [58/114] vs 30.7% [35/114]). There was no difference in caregivers’ and patients’ report that the oncologist said MM was incurable (84.2% [101/120] vs 83.3% [100/120]) (Figure 4).
Discussion
We examined the QOL, psychological distress, and prognostic perceptions of caregivers of patients with MM by line of therapy. Caregivers of patients with MM undergoing treatment experience impaired QOL and elevated psychological distress across the disease continuum, irrespective of the line of therapy. Further, caregivers of patients with MM reported higher levels of anxiety than the patients themselves. Though there were no statistically significant differences in QOL and mood by line of therapy, the proportion of caregivers endorsing clinically significant impairments and distress was substantial and speaks to the long-term challenges for caregivers of patients with MM and the need for supportive interventions to improve their QOL and care.
The level of anxiety seen in caregiver of patients with MM is striking, but what distinguishes the psychological distress of caregivers of patients with MM is the uniquely sustained level of distress across a long disease continuum. Previous studies have shown elevated but comparatively lower rates of psychological distress in other caregiver population, including those with advanced solid tumors.24-27 Caregivers of patients with other hematologic malignancies and those undergoing hematopoietic stem cell transplant experience distress acutely at the time of transplant, which declines over a few months.28,29 In contrast, caregivers of patients with MM continue to struggle with high levels of psychological distress across the disease trajectory. This distress may be due to caregivers’ experience of worry about their loved ones and uncertainty regarding the future. However, treatment for MM requires frequent visits over many years, and the high prevalence of symptoms over the course of therapy may also contribute to caregiver burden and distress.30 Despite this heightened distress, only a minority of caregivers of patients with advanced cancer access mental health services.31 Unfortunately, supportive care interventions to address the psychological needs of caregivers of patients with MM are also lacking.32 These findings highlight the need to screen for psychological distress in caregivers of patients with MM and to develop and test innovative and potentially scalable interventions to mitigate distress throughout the illness course.
In our study, caregivers of patients with MM demonstrated a strong desire for detailed information about their loved ones’ treatment and prognosis. Despite some satisfaction with the amount of information received about the disease and prognosis, a large proportion of caregivers reported an inaccurate understanding of their loved ones’ prognosis or treatment goals. Although the majority of our caregivers reported that their oncologist had told them that the patient’s cancer was incurable, almost 46% reported that the patient’s cancer was likely curable, and more than a one-fourth of caregivers reported their primary treatment goal was cure. Interestingly, when examining patient-caregiver dyads, caregivers reported a more accurate understanding of the patients’ prognosis, similar to prior studies in patients with other incurable malignancies.33,34 It is also possible that patients and caregivers may not interpret the terms “curable” and “terminal” similarly to clinicians, and that may reflect the limitation of our capacity to measure prognostic perceptions in this population.35,36 The discrepancy between hearing the patients’ cancer is incurable and reporting that the patient’s disease is curable may also reflect cognitive dissonance and the internal conflict that caregivers experience as they process their loved ones’ prognosis but still hope for a possibility of a cure.35 Our current approach to evaluating prognostic perceptions does not take into account the potential role of cognitive dissonance in affecting caregivers’ survey responses. Further work is needed to develop a validated tool to measure illness and prognostic understanding in oncology that considers both the cognitive and the emotional aspects involved in answering questions about prognosis.35
For patients and caregivers to weigh the benefits and burdens of a cancer therapy, they must understand the goals of treatment. It remains unclear to what extent caregivers' prognostic awareness and acceptance of the patients' prognosis impact medical decision making in MM. It has been demonstrated that when caregivers have an accurate understanding about prognosis, they are better positioned to help patients cope with their prognosis, participate in conversations related to goals of care, advocate for patients' best interests, anticipate the outcome of terminal illness, and make informed decisions.10-14 Further studies are needed to elucidate further caregivers' prognostic awareness and its association with medical decision making, particularly at the end of life, in MM.31
We also found that caregivers’ acknowledgment that the oncologist said the cancer was incurable was not associated with their QOL or psychological distress. Other studies in caregivers of patients with hematologic malignancies have shown that caregivers’ prognostic awareness is not associated with their distress.33,34 Some oncologists may be concerned that having discussions focused on prognosis may take away hope or cause despair; however, our study findings do not support this notion. Importantly, most participants in this study wanted to know as many details as possible related to their diagnosis and treatment and valued knowing about their prognosis. Our data will hopefully provide reassurance to providers that they may communicate prognosis openly and honestly with caregivers. Our study did, however, demonstrate that acknowledgment of terminal illness was associated with higher levels of anxiety. Terminal illness acknowledgment often captures a particularly ill population near the end of life, which may have lower QOL and higher psychological distress. These factors may account for the differences seen in anxiety between caregivers who identify their loved one as having an incurable illness vs those who identify their loved one as terminally ill. Psychosocial interventions that promote adaptive coping strategies can play an important role in improving the psychological well-being of caregivers.37,38
Our study has several limitations. First, we conducted this study at an academic center with a relatively homogeneous, primarily White, population. These findings may not generalize to more diverse populations across different geographic areas. This study enrolled caregivers to 1 of 3 cohorts based on line of therapy rather than following individual caregivers over the entirety of their loved one’s MM course and therefore relies on comparison between caregivers of different patients with different disease characteristics. Further, this study did not survey caregivers of patients receiving maintenance therapy, which is typically a time where visit burden is lower and disease control is better, and, thus, caregivers may have higher QOL and less psychological distress. Though we also did not capture distress and its relationship to autologous stem cell transplant, which is typically a time of higher distress. We did not capture data on financial distress or income and thus are unable to explore this relationship. Another limitation is that we did not capture caregivers’ mental health history prior to the patient’s diagnosis.
In summary, we demonstrated that caregivers of patients with MM had impaired QOL across the disease course, with 44% of caregivers suffering from clinically significant anxiety and nearly one-fourth suffering from PTSD symptoms. These impairments persisted and remained consistent as the disease progressed through later lines of therapy. We also demonstrated that caregivers hold significant misperceptions regarding treatment goals and prognosis despite a strong desire for detailed information relating to their cancer. Future research should focus on the delivery of adequate psychosocial support throughout the disease course and on the optimal delivery of prognostic information. Interventions are needed to improve caregiver QOL, reduce their psychological distress, and cultivate adaptive coping strategies that may help improve the shared experience over the MM disease course.
Acknowledgments
The authors thank Mary Sanderson and her caregivers.
This work was supported by The Mary Sanderson Fund. A.S.S. was supported by funding from the National Institutes of Health National Cancer Institute (NCI) (K08CA252174).
Authorship
Contribution: E.K.O. contributed to the conception and design of work, data analysis and interpretation, drafting the article, and final approval of the version to be published; Y.N.S. contributed to data collection; B.Y.H. contributed to drafting the article; O.N., A.J.Y., J.P.L., A.R.B., K.C.A., C.C.M., N.C.M., I.M.G., A.S.S., E.A.A., J.N.B., C.C.H., P.G.R., and N.S.R. contributed to investigation and critical revision of the article; and A.E.-J. contributed to design of work, data analysis and interpretation, critical revision of the article, and final approval of the version to be published
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Elizabeth K. O’Donnell, Massachusetts General Hospital, 55 Fruit St, Boston, MA 02114; e-mail: ekodonnell@mgh.harvard.edu.
References
Author notes
For data sharing, please contact the corresponding author at ekodonnell@mgh.harvard.edu.