Key Points
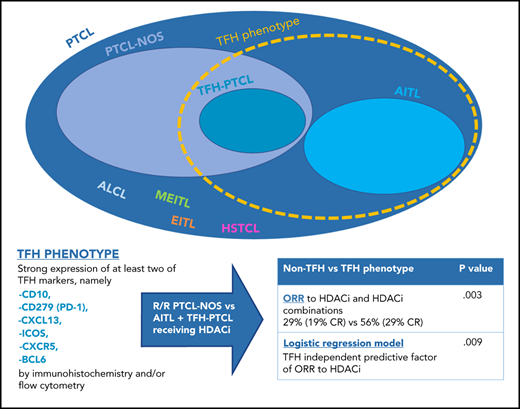
T follicular helper phenotype is an independent predictor of response to HDACi in peripheral T-cell lymphoma.
PFS showed a trend in favor of the TFH phenotype, and 18% of the TFH patients can use HDACi as a bridge to allogeneic transplantation.
Abstract
Histone deacetylase inhibitors (HDACi) are active agents for peripheral T-cell lymphoma (PTCL). Anecdotally angioimmunoblastic T-cell lymphoma (AITL) appears to respond better than PTCL–not otherwise specified (NOS) to HDACi. The new World Health Organization classification shows that a subgroup of PTCL carries similarities in phenotype and gene expression profiling to AITL, comparable to T follicular helper (TFH) cells. The disease might behave similarly to AITL when treated with HDACi. We analyzed 127 patients with AITL or PTCL-NOS treated with HDACi at relapse as a single agent or in combination. We re-reviewed the pathology of all PTCL-NOS to identify the TFH phenotype. Patients received HDACi at relapse as a single agent in 97 cases (76%, 59 TFH, 38 non-TFH) or in combination in 30 cases (24%, 18 TFH, 12 non-TFH) including duvelisib, lenalidomide, lenalidomide plus carfilzomib, and pralatrexate. Seven PTCL-NOS had TFH phenotype; 2 PTCL-NOS were reclassified as AITL. Overall response rate (ORR) was 56.5% (28.9% complete response [CR]) in TFH and 29.4% (19.6% CR) in non-TFH phenotype patients (P = .0035), with TFH phenotype being an independent predictor of ORR (P = .009). Sixteen patients sufficiently responded to HDACi or HDACi in combination with another agent to proceed directly to allogeneic transplantation; 1 of 16 responded to donor lymphocyte infusion (12 TFH, 4 non-TFH). Our results, although retrospective, support that HDACi, as a single agent or in combination, may have superior activity in TFH-PTCL compared with non-TFH PTCL. This differential efficacy could help inform subtype-specific therapy and guide interpretation of HDACi trials.
Introduction
Patients with relapsed or refractory peripheral T-cell lymphoma (PTCL) have poor prognosis, with a median survival of 6 to 10 months.1,2
Romidepsin and other histone deacetylase inhibitors (HDACi) are active agents for relapsed/refractory PTCL, achieving overall responses in around 25% of patients and median duration of response of 13 to 17 months in the studies leading to their US Food and Drug Administration approval.3-5 Histones are proteins that maintain DNA configuration and regulate access to genes by transcription factors via their acetylation or deacetylation. HDACi increase the histone acetylation, which is thought to reduce the expression of tumor suppressor genes and oncogenes.2
The recent World Health Organization (WHO) classification of lymphoid malignancies, refined the PTCL–not otherwise specified (NOS) category, introducing a subtype of PTCL defined as nodal PTCL with T follicular helper phenotype (TFH).6 TFH-PTCL is thought to share the same cell of origin as angioimmunoblastic T-cell lymphoma (AITL),7 because it carries a similar mutational pattern and gene expression profile that are believed to confer sensitivity to HDACi via epigenetic regulation and other different mechanism.8,9
Anecdotally, AITL appears to respond better than PTCL-NOS to romidepsin.3 This trend has been shown in some clinical trials of single-agent HDACi and combinations, but numbers have been too small to drive conclusions.4,5,10-14 However, the registration studies of these agents showed a tendency toward better overall response rate (ORR) in AITL with belinostat (ORR 45.5% for AITL vs 23.3% for PTCL-NOS)4 and superimposable results with romidepsin (ORR 30% for AITL vs 29% for PTCL-NOS).5 Of note, all the registration studies and most of the combination studies have been conducted prior to the publication of the new WHO classification where the TFH phenotype PTCL was defined.
Our hypothesis is that AITL and TFH-PTCL might respond better to treatment with HDACi than PTCL-NOS. To explore this question, we conducted a multicenter retrospective cohort study and evaluated the outcomes of patients with PTCL (AITL, TFH-PTCL, and PTCL-NOS) treated with HDACi, either in combination or as single agents, across 6 international sites.
Methods
After approval by the institutional review boards at 6 academic institutions, patients with relapsed/refractory PTCL who received HDACi at relapse, either in combination or as a single agent, in the context of a protocol or as commercial supply, were identified at each site. Criteria to include patients were slightly different at each site. At Memorial Sloan Kettering Cancer Center and Washington University in St. Louis, MO, all patients receiving HDACi were identified by the pharmacy database, and all patients treated in the setting of relapsed/refractory PTCL were selected. At Weill Cornell Medical College, Peter MacCallum Cancer Center, Concord Repatriation General Hospital, and Stanford University, patients were selected from institutional lymphoma databases. We included in the analysis all cases that were identifiable as AITL, PTCL-NOS, and TFH-PTCL according to the WHO classification of 2016.6 The majority of the cases classified as PTCL-NOS were re-reviewed at each institution to assess the TFH phenotype. When the physical re-review was not feasible, the phenotype was reassessed by looking at the markers’ expression on the pathology reports. This phenotype was defined as having strong expression by immunohistochemistry and/or flow cytometry of at least 2 TFH markers, among CD10, CD279 (PD1), CXCL13, ICOS, SAP, CCR5, and BCL6.2 Pathology review was performed locally at each institution. Cases of PTCL-NOS in which the tissue could not be reviewed and a minimum of at least 2 markers for TFH were not included in the report were excluded from this analysis.
Medical and pathology records were evaluated for clinical characteristics, pathologic and radiologic data, and treatment history at each institution. Treatment was considered to have occurred if at least 1 dose of the drug was administered. The investigators at each site reported responses based, whenever possible (121 of 127 patients), on the Lugano criteria applied retrospectively.15 In 6 cases, the patients did not receive a second positron emission tomography/computed tomography assessment. These patients had received >3 doses of HDACi and were coded as nonresponders.
Progression-free survival (PFS) was defined as time from the initiation of the first treatment until death or progression. Patients undergoing allogeneic transplant right after HDACi (bridge to transplant) were censored at the time of transplant, and transplant was not considered an event. PFS was defined as time from initiation of HDACi until investigator-assessed progression, death from any cause, or date of last follow-up if in remission. Time-to-event statistics were estimated using the Kaplan-Meier method; differences in survival were estimated with log-rank; and differences between groups were estimated with the Mann-Whitney U test, Fisher’s exact test, and the logistic regression model. Follow-up time was calculated by the reverse censoring method. Analyses and graphs were performed with the statistical programs R, STATA, GraphPad, and the cBioPortal.
Results
Patients
A total of 164 patients receiving HDACi between April 2005 and January 2019 were identified from 6 institutions.
A total of 127 patients met the inclusion criteria. Thirty-seven patients were excluded from the analysis for the following reasons: 13 patients with PTCL were not evaluable for the TFH phenotype; 5 patients had other forms of T-cell lymphoma (2 monomorphic epitheliotrophic intestinal T-cell lymphoma, 2 hepatosplenic T-cell lymphoma, 1 anaplastic large cell lymphoma); 7 received romidepsin as maintenance after autologous transplant on a clinical trial (NCT01908777); 11 patients were treated on a clinical trial combining romidepsin with gemcitabine and oxaliplatin (NCT02181218); and 1 patient died minutes after the infusion of HDACi from a sudden cardiac arrest and was not evaluable. All patients relapsed after frontline chemotherapy per the inclusion criteria of the study. Median follow up was 31.6 months (range, 0.3-126.5 months). Characteristics of the 127 patients at time of HDACi therapy are described in Table 1.
Ninety-seven patients were treated with single-agent romidepsin (n = 84) or belinostat (n = 13), 14 in the context of clinical trials and 83 as commercial supply. Thirty patients were treated with romidepsin combinations, 29 as part of a clinical trial (11 received romidepsin/duvelisib [NCT02783625],10 12 received romidepsin/carfilzomib/lenalidomide [NCT02341014],13 6 received romidepsin/lenalidomide [NCT01755975]12 ); 1 patient received romidepsin/pralatrexate16 as commercial supply. After pathology re-review of the PTCL-NOS cases, where it was feasible to add Immunohistochemistry for the TFH markers, 7 patients were classified as TFH-PTCL, and 2 patients were reclassified as AITL.
ORR
The ORR to HDACi as both single agent and in combination was 45.6% (32 of 127 patients, 25% complete response [CR]). When HDACi were used as single agents, ORR was 45.3% (23 of 97 patients [23.7% CR]) and 46.6% (9 of 30 patients [30% CR]) when used in combination. Table 2 summarizes the ORR for patients with TFH phenotype and non-TFH phenotype in our cohort, when treated with single agent or in combination.
To evaluate if the TFH phenotype might be an independent predictor of response, we performed a univariate analysis of 12 variables that might have impacted the ORR, and then a logistic regression model of the significant variables (Table 3).
All variables were calculated at the time of relapse before HDACi infusion, and included age, stage, extranodal involvement, performance status (ECOG), LDH, IPI stage, autologous transplantation as consolidation of first line therapy, response to first-line chemotherapy (CR and partial response vs stable disease [SD] and progressive disease [PD]), lines of treatment before HDACi, and combination vs single agent HDACi.
After univariate analysis, 2 variables were significantly associated to ORR: TFH phenotype and response to first-line chemotherapy (P = .003 and P = .010, respectively). Logistic regression demonstrated that the 2 variables have independent predictive value. P value for TFH phenotype was .009 (std, −1.02; error, 0.39).
PFS and bridge to allogeneic transplantation
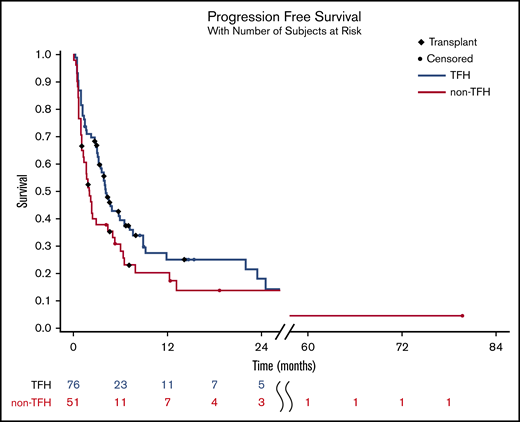
Median PFS after HDACi was 4.1 months for TFH phenotype patients and 2.1 months for non-TFH phenotype patients; log rank P = .18 (hazard ratio [HR] 0.5 for TFH; 95% confidence interval [95% CI], 0.33-0.75) (Figure 1).
PFS of relapsed/refractory TFH vs non-TFH phenotype PTCL after HDACi. PFS was 4.1 months for TFH phenotype patients and 2.1 months for non-TFH phenotype patients; log rank P = .18 (HR 0.5 for TFH; 95% CI, 0.33-0.75). For patients undergoing allogeneic stem cell transplantation, time on the curve was censored at the time of transplant.
PFS of relapsed/refractory TFH vs non-TFH phenotype PTCL after HDACi. PFS was 4.1 months for TFH phenotype patients and 2.1 months for non-TFH phenotype patients; log rank P = .18 (HR 0.5 for TFH; 95% CI, 0.33-0.75). For patients undergoing allogeneic stem cell transplantation, time on the curve was censored at the time of transplant.
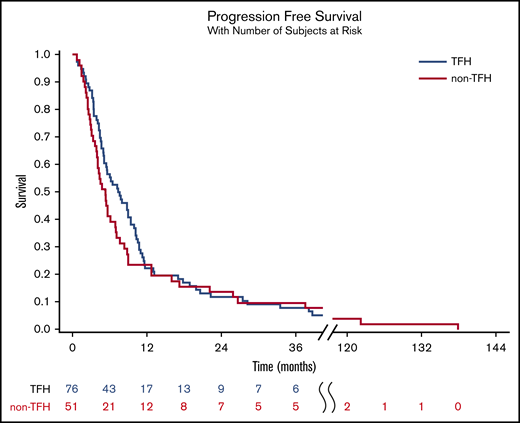
Median PFS after frontline had been 7.3 months for the TFH patients and 5.3 months for the non-TFH phenotype patients; log rank P = .65 (HR 1.39 for non-TFH; 95% CI, 0.98-1.99) (Figure 2).
PFS of relapsed/refractory TFH vs non-TFH phenotype PTCL after front-line chemotherapy, of which 25% underwent high-dose chemotherapy and autologous stem cell rescue. PFS was 7.3 months for the TFH patients and 5.3 months for the non-TFH phenotype patients; log rank P = .65 (HR 1.39 for non-TFH; 95% CI, 0.98-1.99).
PFS of relapsed/refractory TFH vs non-TFH phenotype PTCL after front-line chemotherapy, of which 25% underwent high-dose chemotherapy and autologous stem cell rescue. PFS was 7.3 months for the TFH patients and 5.3 months for the non-TFH phenotype patients; log rank P = .65 (HR 1.39 for non-TFH; 95% CI, 0.98-1.99).
For the 42 patients with TFH phenotype who responded to HDACi, median duration of response was 7 months (range, 0.2-45 months). The 15 patients with non-TFH PTCL who responded to HDACi had a median duration of response of 16 months (range, 0.9-77 months).
Twenty-nine patients (23%) in this cohort underwent allogeneic stem cell transplantation at some point after receiving HDACi, 10 (8%) with non-TFH phenotype and 19 (15%) with TFH phenotype PTCL. Fifteen patients (12%) proceeded directly to allogeneic transplantation after achieving a response to HDACi. One received HDACi as a bridge to donor lymphocyte infusion. Twelve (75%) of these patients using this bridging HDACi had a TFH phenotype PTCL, and 4 (25%) had non-TFH phenotype PTCL (Figure 1). Of these 16 patients, 10 are alive and 5 are also in remission at last follow-up.
Setting a cutoff for age (TFH phenotype are 8 years older than non-TFH, median 63 years [range, 29-83 years] vs 55 years [range, 30-81 years]; P = .003) and excluding patients older than 75 years at time of HDACi, a similar percentage of patients with TFH phenotype (19 of 65, 29%) and non-TFH phenotype (10 of 46, 22%) in our population received an allogeneic transplantation (P = .511). Considering only transplants with romidepsin as bridge, 12 of 65 (18%) TFH-phenotype patients reached allogeneic transplant and 4 of 46 (8.6%) non-TFH reached transplant (P = .178). Five patients died of transplant-related complications, 1 from Pneumocystis jirovecii pneumonia after relapsing after allogeneic transplantation. Median overall survival for this population was 12 months (range, 4-83 months)
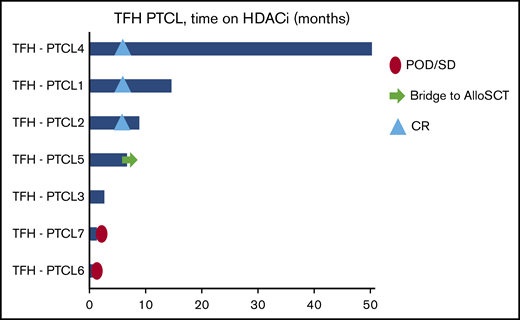
TFH patients
ORR in the TFH-PTCL group (n = 7) was 71% (3 CR, 2 partial response, 1 SD, and 1 PD) (Figure 3). Four patients were treated with romidepsin or belinostat as single agent (3 responded, 1 achieved SD); 3 patients were included in romidepsin combinations protocols (2 responded, 1 had PD). Patients with TFH-PTCL had higher ORR when compared with PTCL-NOS (71% vs 29%, P = .041), but had similar ORR when compared with those with AITL (71% vs 56%, P = .693) (Figure 3).
Swimmer’s plot detail of the patients with TFH PTCL. POD, progression of disease.
Swimmer’s plot detail of the patients with TFH PTCL. POD, progression of disease.
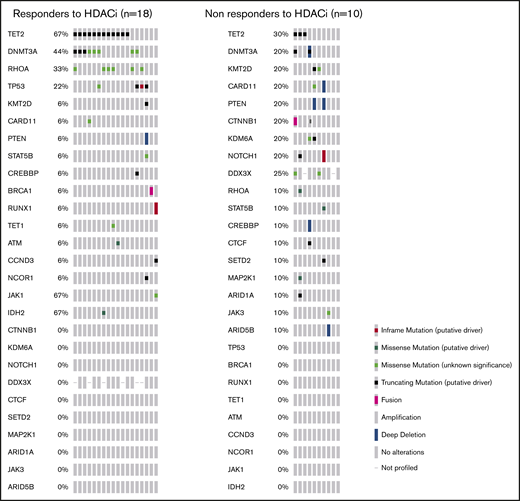
Mutational analysis
MSK IMPACT-heme 400-genes targeted sequencing17 was performed with modification of a previously published method to include genes specifically mutated in hematological malignancies. The analysis was performed with a paired normal DNA sample at the time of relapse/refractoriness in 28 patients, including 10 with non-TFH and 18 with TFH phenotype PTCL. Of the TFH phenotype PTCL, 14 responded to HDACi and 4 had SD or PD.
Among the non-TFH phenotype PTCL, 4 responded to HDACi and 6 had SD or PD. Figure 4 shows a detail of the targeted sequencing results, all performed at Memorial Sloan Kettering Cancer Center, with the genes ordered for frequency of mutations, divided among responders and nonresponders to HDACi using the cBioPortal.18 All 10 PTCL-NOS among these 28 cases were re-reviewed by pathology.
Detail of all more frequent mutations found on targeted sequence IMPACT heme panel performed at time of relapse/refractoriness in 28 patients receiving HDACi.
Detail of all more frequent mutations found on targeted sequence IMPACT heme panel performed at time of relapse/refractoriness in 28 patients receiving HDACi.
In this small group of patients, typical AITL mutations (TET2, and/or DNMT3A, and/or RHOA) were present in 15 of 18 of patients responding to HDACi (83%) and in 4 of 10 nonresponding to HDACi (40%) (P = .034). Responders to HDACi were AITL or TFH PTCL in 14 of 18 cases (77%) and 4 of 10 of the nonresponders (40%) (P = .097). Two patients with histopathological diagnosis of AITL did not have typical AITL mutations, and both had progression of disease despite HDACi. Two patients with PTCL-NOS had at least 1 typical AITL mutation (RHOA and DNMT3A), 1 achieved a CR, the other had SD.
Patients with mutations that are thought to confer resistance to chemotherapy, like DNMT3AR882X (n = 4; 3 AITL, 1 TFH-PTCL)19 and TP53 (4 patients) all responded to HDACi. In our cohort, 4 of 18 (22.2%) relapsed/refractory TFH-PTCL and AITL patients had DNMT3AR882X mutation. One of the 4 patients with DNMT3AR882X had previously responded to chemotherapy consolidated with autologous stem cell transplantation but was found to have relapsed at restaging post-AutoSCT. Additional details of this population are present in the supplemental Data.
Discussion
In this large retrospective study, we support the clinical observation that treatment with HDACi appears to achieve higher responses in patients with TFH phenotype lymphoma (AITL and TFH-PTCL) than PTCL-NOS.
Both patients receiving HDACi as single agent and, less prominently, those receiving HDACi combinations, showed higher percentages of response when compared with PTCL-NOS. In our series, patients with TFH-PTCL and AITL have similar responses and duration of response to HDACi-based therapy.9
In the linear regression model, the TFH phenotype demonstrated to be 1 of the only 2 variables at time of relapse that could independently predict ORR to HDACi in our cohort. Of interest, the characteristics of performance status, stage, LDH and the comprehensive IPI score did not seem to influence the response to HDACi. The second variable found to independently predict response to HDACi was the response to frontline chemotherapy, with patients not achieving response (with PD or SD) to chemotherapy less frequently responding to HDACi.
Although the PFS with HDACi appears similar between TFH and non-TFH phenotype patients, 12 (18%) patients in the TFH subgroup vs 4 (8%) in the non-TFH phenotype group subsequently underwent allogeneic transplantation using HDACi as a bridge therapy, and these patients were censored at the time of transplant. Median time from start of HDACi to allogeneic transplant was 4 months (range, 2-14 months).
The retrospective nature of our study presents several limitations. The most evident is that the ORR and CR rate to HDACi is higher than seen in the registration studies of romidepsin and belinostat. This may be because of nonhomogeneous patient selection among different academic centers, leading to enrichment of responding patients in the dataset. Nevertheless, this kind of bias should equally affect the AITL and PTCL subgroups. We also included patients receiving combinations of HDACi with other drugs. Patients enrolled in these trials are equally distributed between TFH and non-TFH phenotype; however, this is another factor in the higher-than-expected ORR. Moreover, this is a cohort treated at big academic sites, and the results might not be representative of the general patient population.
Our limited data on targeted sequencing seem to suggest that mutations typically found in TFH phenotype might predict responsiveness to HDACi in addition to the pathologic diagnosis itself. These are very preliminary data on a small group of patients. The data will require confirmation in larger cohorts.
In a prospective study of patients with AITL receiving first line chemotherapy and lenalidomide, Lemonnier et al.19 have found that the DNMT3AR882X mutations were associated with resistance to chemotherapy in all 6 mutated and 64 nonmutated (9.4%) patients. Resistance to anthracycline had similarly been reported in DNMT3AR882X-mutated AML.20
In our cohort of relapsed/refractory patients receiving HDACi, 4 of 18 (22.2%) AITL patients were found to have the DNMT3AR882X mutation. Three of the 4 patients in this series with DNMT3AR882X did not respond to initial chemotherapy and 1 progressed shortly after autologous transplantation. All 4 patients with DNMT3AR882X subsequently responded to HDACi.
In conclusion, these data suggest that using HDACi in combination therapies for AITL and TFH PTCL might be a particularly promising strategy. Likewise, when designing a trial including HDACi, the proportion of patients with TFH-phenotype PTCL may influence the overall response to that treatment.
For the original deidentified data, proposal for access should be e-mailed to the corresponding author, Paola Ghione (paola.ghione@roswellpark.org). Individual participant data will not be shared.
Acknowledgments
The authors gratefully acknowledge the members of the Molecular Diagnostics Service in the Department of Pathology at Memorial Sloan Kettering Cancer Center.
This work was funded in part by the Marie-Josée and Henry R. Kravis Center for Molecular Oncology and National Institutes of Health, National Cancer Institute Cancer Center Core Grant No. P30-CA008748 and MSK Lymphoma SPORE P50 CA192937 (A.D.).
The funders were not involved in the study design, data collection, data analysis, manuscript preparation, or publication decisions.
Authorship
Contribution: S.H. and P.G. idealized the project; P.G. and S.H. wrote the manuscript; P.G., P.F., N.M.-S., S.B., J.Y., M.A.S., M.L., N. Galasso, N. Ganesan, and C.v.d.W. collected and interpreted the patients’ information from medical records; N.O., G.I., and A.D. reviewed and supervised the pathology review; V.S. and P.G. analyzed the patients’ data; and N.M.-S., M.L., A.M., C.v.d.W., J.R., H.M.P., J.T., R.A., and S.H. treated and followed the patients.
Conflict-of-interest disclosure: S.H. had a consulting or advisory role with Celgene, Millennium Pharmaceuticals, Kyowa Hakko Kirin, Seattle Genetics, ADC Therapeuticals, Corvus Pharmaceuticals, Innate Pharma, miRagen, Portola Pharmaceuticals, Verastem, and Takeda Pharmaceuticals and received research funding from Celgene, Seattle Genetics, Takeda Pharmaceuticals, Kyowa Hakko Kirin, Aileron Therapeutics, ADC Therapeutics, Verastem, and Forty Seven. A.M. received honoraria from Seattle Genetics; had a consulting or advisory role for Seattle Genetics, Kyowa Hakko Kirin Pharma, Miragen Therapeutics, Takeda Pharmaceuticals, ADC Therapeutics, Cell Medica, Bristol-Myers Squibb, and Erytech PharmaResearch; and received funding through her institution from Incyte, Seattle Genetics, Merck, and Bristol-Myers Squibb. M.L. had a consulting or advisory role with TG Therapeutics, Celgene, Gilead Sciences, Juno Therapeutics, Seattle Genetics, AbbVie, Pharmacyclics, Janssen Oncology, Verastem, Kite Pharma, Novartis, Spectrum Pharmaceuticals, and Bristol-Myers Squibb and received research funding through his institution from Celgene, Curis, Juno Therapeutics, Janssen Oncology, TG Therapeutics, TG Therapeutics, and miRagen. R.A. had a consulting or advisory role with Seattle Genetics and Takeda and received research funds from Seattle Genetics, Merck, and Millenium. J.T. received research funding from Beigene, Genentech, Pharmacyclics, Janssen-Cilag, Takeda Pharmaceuticals, and Celgene. N.M.-S. received institutional research funding from Bristol-Myers Squibb, Celgene, Verastem Pharmaceuticals, Innate Pharmaceuticals, Corvus Pharmaceuticals, and Genentech/Roche and was a consultant for Kyowa Hakka Kirin, and C4 Therapeutics. H.M.P. received research funding from Celgene and was on the advisory boards of Celgene and Bristol-Myers Squibb. J.R. received research funding from Celgene, Pharmacyclics, AstraZeneca, and Seattle Genetics. A.D. received personal consultancy fees from Roche, Corvus Pharmaceuticals, Physicians' Education Resource, Seattle Genetics, Takeda, EUSA Pharma, and AbbVie; research grants from National Cancer Institute and Roche; and consulted/was on an advisory board for Celgene, Pharmacyclics, AstraZeneca, Juno, Kite Pharma, and Cellectar. The remaining authors declare no competing financial interests.
Correspondence: Paola Ghione, Roswell Park Comprehensive Cancer Center, Elm and Carlton Streets, Buffalo, NY 14263; e-mail: paola.ghione@roswellpark.org.
References
Author notes
The full-text version of this article contains a data supplement.