Lymphoma experts in the United States have changed the way Hodgkin lymphoma (HL) is managed in the curative setting; this has implications on treatment of the heavily pretreated patient. This is highly relevant in a few important circumstances: the lack of enthusiasm for any radiotherapy (RT) in early-stage disease for patients without bulky disease, and the use of brentuximab vedotin (BV) in the salvage setting despite limited evidence of a survival advantage compared with chemotherapy-only salvage regimens. Last, the fate of upfront therapy for advanced stage HL will be dependent on the results of the phase 3 Frontline Therapy Trial in Patients With Advanced Classical Hodgkin Lymphoma, which compared doxorubicin, bleomycin, vinblastine, and dacarbazine to BV–adriamycin, vinblastine, and dacarbazine. Preliminary data suggest a 6% improvement in the experimental arm at 2 years; whether this leads to a new standard of care is debatable.
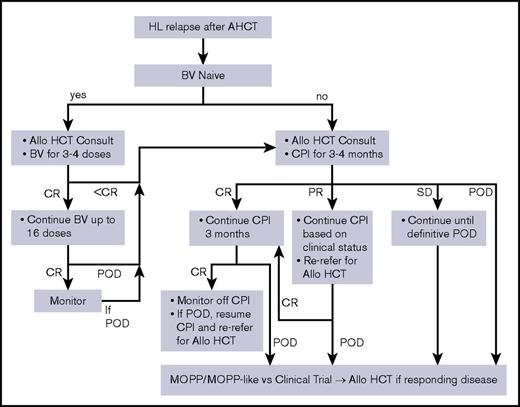
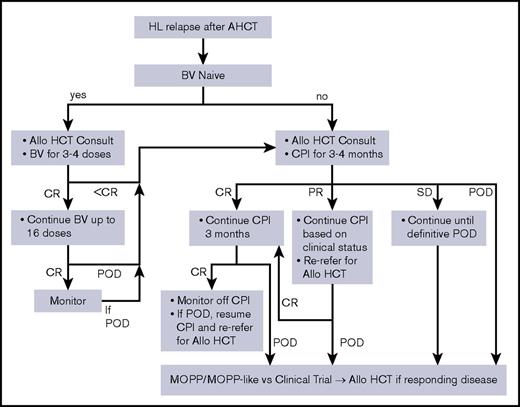
Schema for relapse of HL after ASCT. MOPP, nitrogen mustard, vincristine, procarbazine, prednisone; POD, progression of disease; SD, stable disease.
Schema for relapse of HL after ASCT. MOPP, nitrogen mustard, vincristine, procarbazine, prednisone; POD, progression of disease; SD, stable disease.
For patients in which high-dose therapy and autologous stem cell transplantation (ASCT) has failed, treatment options for these healthy young patients was some type of bridging therapy to a potentially curative nonmyeloablative allogeneic transplant (NMT) provided this bridging therapy shrinks the HL to a minimal disease state. If achieved, reports in the literature suggest that 30% to 60% of patients achieve long-term event-free survival. However, in 2017, we have an array of treatment options for these patients and the kneejerk response is questionable.1-3
Early-stage disease and the need for RT
The rationale for administering RT in the relapsed setting is that heavily pretreated patients frequently progress at sites of previous nodal disease. There are multiple studies supporting the incorporation of RT as a part of salvage treatment; however, because there is a lack of phase 3 data, medical oncologists continue to not use this modality for fear of long-term side effects.4-7 In second and later lines of therapy, this rationale is naïve because these patients die of HL as opposed to treatment-related side effects. ln fact, this is increasingly relevant because current treatment approaches for early-stage HL is positron imaging tomography (PET)–adapted, with 3 to 4 cycles of doxorubicin, bleomycin, vinblastine, and dacarbazine alone as standard of care, provided the result on PET imaging is favorable.8-9 Therefore the majority of patients receive primary and salvage therapy followed by high-dose therapy/ASCT without receiving any RT. I firmly believe that RT is the single most effective modality of therapy for HL and should be administered in patients in which ASCT fails, provided the disease can be encompassed into reasonable radiation field. One could argue that this field can be as large as a mantle or inverted Y. In this post-ASCT failure setting, if a complete response (CR) is achieved after RT, no further therapy is necessary and the patient can be monitored.
The majority of patients have widespread disease post-ASCT; therefore, the use of RT for advanced-stage HL makes little sense other than for palliation. Before the development of BV and the checkpoint inhibitors (CPIs), the median survival for this subset of HL patients was 2 years.
BV
BV was initially developed in this post-ASCT palliative setting and US Food and Drug Administration–approved in 2011.10-11 There is now long-term follow-up on the early studies. The majority of patients have clinical benefit from therapy, but the CR rate is <40%. Only one-third of CR patients are event-free at 4 years.12 We have also learned 3 important lessons with BV therapy in the post-ASCT setting: (1) it is extremely rare for a partial response (PR) to BV to convert to a CR with additional BV cycles; (2) nearly all CR patients achieve this end point at the first restaging; and (3) in 2017, BV was commonly administered before the post-ASCT failure setting and retreat with this agent needs to be based upon prior response to BV.
In the United States, BV can be used pre-ASCT as part of salvage treatment,13 but more commonly is used as maintenance therapy post-ASCT based upon the results of the Phase 3 Study of Brentuximab Vedotin (SGN-35) in Patients at High Risk of Residual Hodgkin Lymphoma Following Stem Cell Transplant trial. Updated results show a 4-year progression-free survival rate of 61% for the BV arm vs 43% placebo with a hazard ratio of 0.58 (95% confidence interval, 0.41-0.82).14 Patients in this study did not have BV before ASCT, and there are limited data for maintenance BV for those with pre-ASCT exposure; however, it is still administered for patients with poor risk disease. Therefore most patients will not be BV naïve if an ASCT fails.
For the few patients that have never received BV, I administer this agent as the first treatment after a failed ASCT because a CR nearly always happens at the time of first restaging. I recommend administering 3 to 4 doses followed by repeat PET imaging; if negative, another 4 to 6 doses are given. If the CR is durable, I monitor the patient off therapy. If a PR is achieved, one needs to consider changing therapy to a CPI or referring for an NMT. For patients that are not BV naïve at the time of post-ASCT failure, unless they had a CR to pre-ASCT therapy, the use of BV with curative intent is unclear and I would treat with a CPI first.
CPI
The use of CPI in the post-ASCT palliative setting will change the way relapse and refractory HL is managed. The CPI are so active that it is now unclear what the median survival of patients is when ASCT fails leading to the development of a potential new HL pathway, “chronic HL.” Two PD1 blocking drugs are now US Food and Drug Administration–approved: nivolumab and pembrolizumab.15-18 In solid tumors, we know that PD-1 ligand expression is predictive of response, antitumor immunity is mediated by CD8+ effector T cells, response is enhanced by increased tumor mutation burden, and the process requires major histocompatibility complex-I (MHC-I).19-22 The Reed-Sternberg cell is nearly always positive for PDL1 expression through 9p24.1 amplification, so this disease should be primed to respond to a PD1 blocking agent.23 However CD8+ T cells are not prevalent in the HL microenvironment; there is frequent loss of both MHC-I and MHC-2 and the mutational burden is not high. How these agents work in HL is being actively investigated, but it is clear that the response rate is higher than with any other malignancy.
To summarize the phase 1/2 experience with nivolumab and pembrolizumab: (1) >500 patients were treated; phase 1B and 2 studies were undertaken; (2) response rate is 65% to 70% and clinical benefit is >90%; (3) CR rate is 22% by investigator; (4) median duration of response is unclear but >1 year; and (5) major side effect-“itis” occurs and it is usually endocrine or inflammatory.24-25 In HL as well as many solid tumors, both of these agents are approved and I see little difference between nivolumab and pembrolizumab; the choice to use 1 over another is unclear.
Combinations of these agents with other novel or traditional chemotherapies are being studied in a multitude of ongoing trials.26 Recently, Herrara et al reported a 62% CR rate with the combination of BV and nivolumab when given with a pre-ASCT salvage regimen. A phase 3 study is under way comparing the combination to BV alone in the palliative setting. Histone deacetylase inhibitors have significant single agent activity in HL and there are ongoing studies combining these drugs with CPI; early results are encouraging.
As stated, the majority of patients with HL will have received BV before or directly after ASCT as part of salvage or maintenance programs; therefore, the CPI will be the treatment of choice for post-ASCT failures.
Considerations for allo-HCT
All lymphoma physicians are aware that a non-NMT can cure heavily pretreated HL patients, but with a high cost of graft-versus-host disease, infectious complications, and treatment failure. However, with the availability of BV and CPI, I see the role for NMT evolving. In 2018, an NMT will not be offered unless both BV and a CPI are administered. Historical data regarding outcomes after allo–hematopoietic cell transplantation (HCT) for HL may no longer be relevant.
There are now a few reports suggesting that NMT can be administered fairly safely after CPI therapy with similar graft-versus-host disease, infectious, and failure data.27-29
My recommendation for a patient that has heavily pretreated HL and that has received BV is as follows (see Figure 1):
If disease is nodal only and stage I/Il, and patient is RT naïve: RT with curative intent
Advanced stage:
○ HLA typing and refer for an allogeneic stem cell transplantation consult
○ Start CPI:
■ If CR is achieved, continue for another 3 months; if CR is maintained, stop therapy and monitor; restart if HL progression and now refer back for NMT consideration
■ If a PR is achieved, continue therapy based upon clinical situation (PR can convert to CR); however, refer back to transplant physician for repeat evaluation and further discussions
■ If stable disease is achieved, a CR will not happen; continue therapy until definitive disease progression and then start either alkykator or gemcitabine-based chemotherapy vs clinical trial, and refer back for allogenic consideration if a PR is achieved
Conclusion
I believe that when ASCT fails, there is now a variety of treatment options and the use of NMT is no longer standard or even a goal. However, all patients with advanced-stage or early-stage disease that cannot be radiated should be referred for an allogeneic stem cell transplant consult. It is important to remember that some patients can be cured with RT alone, BV alone, and likely with CPI in the post-ASCT setting; one should be cautious before recommending an NMT immediately after a failed autologous transplant.
Acknowledgments
This research was supported in part by grants from the National Institutes of Health, National Cancer Institute (P01 CA23766 and P30 CA008748).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Authorship
Contribution: C.H.M. wrote the paper.
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: Craig H. Moskowitz, Department of Medicine, Memorial Sloan Kettering Cancer Center, Weill Cornell Medical College, 885 2nd Ave, 9th Floor, Box 350, New York, NY 10065; e-mail: moskowic@mskcc.org.