Key Points
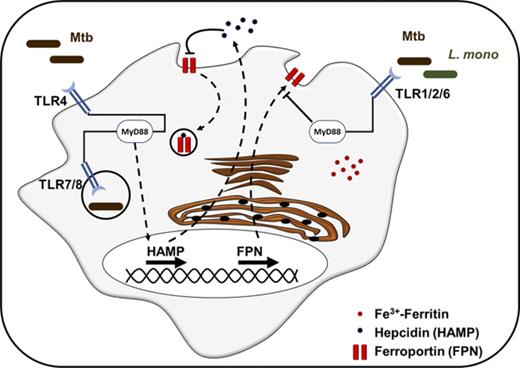
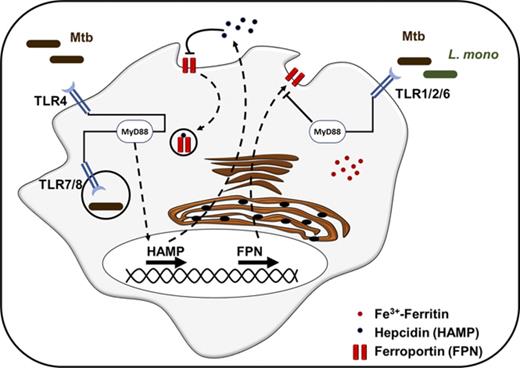
TLR signaling induces intracellular iron sequestration in macrophages through 2 redundant mechanisms.
TLR2 signaling downregulates ferroportin transcriptional expression, whereas TLR4 induces hepcidin secretion.
Abstract
Upon infection, pathogen and host compete for the same iron pool, because this trace metal is a crucial micronutrient for all living cells. Iron dysregulation in the host is strongly associated with poor outcomes in several infectious diseases, including tuberculosis, AIDS, and malaria, and inefficient iron scavenging by pathogens severely affects their virulence. Hepcidin is the master regulator of iron homeostasis in vertebrates, responsible for diminishing iron export from macrophages during iron overload or infection. Hepcidin regulation in hepatocytes is well characterized and mostly dependent on interleukin-6 signaling during inflammation, although in myeloid cells, hepcidin induction and the mechanisms leading to intracellular iron regulation remain elusive. Here we show that activation of different Toll-like receptors (TLRs) by their respective ligands leads to increased iron sequestration in macrophages. By measuring the transcriptional levels of iron-related proteins (eg, hepcidin, ferroportin, and ferritin), we observed that TLR signaling can induce intracellular iron sequestration in macrophages through 2 independent but redundant mechanisms. Interestingly, TLR2 ligands or infection with Listeria monocytogenes lead to direct ferroportin transcriptional downregulation, whereas TLR4 ligands, such as lipopolysaccharide, induce hepcidin expression. Infection with Mycobacterium bovis Bacillus Calmette-Guerin promotes intracellular iron sequestration through both hepcidin upregulation and ferroportin downregulation. This is the first study in which TLR1-9–mediated iron homeostasis in human macrophages was evaluated, and the outcome of this study elucidates the mechanism of iron dysregulation in macrophages during infection.
Introduction
Iron is an essential trace element for the survival of virtually all organisms. This metal is required as a component of molecule sensing, transporting, and storing of oxygen, as well as enzymes involved in oxidation and reduction of substrates during energy production, intermediate metabolism, and generation of reactive oxygen or nitrogen species for host defense. During infections, prokaryotic, eukaryotic, and viral pathogens use multiple complex mechanisms to acquire iron from their hosts, while hosts attempt to sequester it from pathogens, thereby starving them of iron and slowing their multiplication within the host.1,2 Iron consequently represents a point of conflict between host and pathogen, and altered iron balance is associated with poor outcomes in several infectious diseases, including tuberculosis,3 AIDS,4 and malaria.5
Hepcidin, a 25–amino acid peptide hormone, is the master regulator of iron homeostasis in vertebrates.6,7 It is well known that diminished iron export from macrophages that recycle iron from senescent red cells rapidly induces hypoferremia because of the high iron demand of erythropoiesis. Excess levels of hepcidin have been recognized as the main cause of anemia in chronic disease.8-10 Mechanistically, a decrease in iron efflux occurs when hepcidin binds with the iron exporter protein ferroportin. Once bound, the complex is internalized and degraded, culminating in decreased iron release from iron-exporting cells such as macrophages, hepatocytes, and duodenal enterocytes. Recently, Peyssonnaux et al11 demonstrated endogenous expression of hepcidin by mouse myeloid cells, specifically macrophages, in vitro and in vivo. These myeloid cell types produced hepcidin in response to bacterial pathogens in a Toll-like receptor 4 (TLR4)–dependent fashion. Conversely, bacterial stimulation of macrophages triggered a TLR4-dependent reduction in the iron exporter ferroportin.11
TLRs are key sensors of the innate immune system.12 TLRs recognize pathogen-associated molecular patterns (PAMPs) and control the hypoferremic host response. Lipopolysaccharide (LPS) is a cell-wall component of gram-negative bacteria recognized by TLR4. LPS injected into mice causes the release of proinflammatory cytokines and triggers a well-characterized acute phase response, including induction of hepcidin by interleukin-6 (IL-6).13-17 Recently, it was shown that stimulation of the TLR2/6 pathway by Pam3CSK4 or FSL-1 synthetic triacylated lipopeptides triggers a profound decrease in ferroportin gene and protein expression in mouse bone marrow–derived macrophages independent of hepcidin.18 Given the association of iron with infection outcomes, understanding how hepcidin itself is regulated during inflammation and infections is clearly important. However, most studies of hepcidin and its regulation during infection or inflammation have been conducted using hepatocytes. There is little information on how myeloid cells including macrophages regulate hepcidin expression and subsequently iron homeostasis when encountering pathogens or PAMPs.
In this study, we present a comprehensive evaluation of TLR mediation of iron homeostasis in THP-1 human monocytic cells. We determined that different TLRs regulate iron homeostasis in hepcidin-dependent and -independent manners. TLR2, TLR6, and TLR1/2 activation by Pam3CSK4, FSL-1, and Pam2CSK4, respectively, sequester iron by severely inhibiting the expression of ferroportin at the transcriptional level in human macrophages; interestingly, there was little change in hepcidin expression levels. Alternatively, TLR4 and TLR7/8 restrict iron levels inside the macrophage by induction of hepcidin at the transcriptional and translational levels without altering the expression of ferroportin. TLR3, TLR5, and TLR9 neither induce hepcidin nor reduce ferroportin expression in human macrophages. Collectively, this is the first study in which TLR1-9–mediated iron homeostasis in human macrophages was evaluated. The outcome of this study is useful in developing an understanding of the mechanism of iron dysregulation during infection and in inflammatory diseases and disorders.
Material and methods
Bacterial cultures
Mycobacterium bovis Bacillus Calmette-Guerin (BCG) Pasteur and Mycobacterium tuberculosis Erdman (generously provided by Jeff Cox [UC Berkeley, Berkeley, CA]) were cultured in 7H9 broth with 0.5% glycerol, 0.05% Tween 80, and 10% OADC at 37°C to optical density of ∼0.8, aliquoted, and stored at −80°C until used.19 Samples were thawed at 37°C and plated on 7H10 agar for viable colony forming unit (per milliliter) enumeration. Listeria monocytogenes was obtained from the American Type Culture Collection (15313), cultured in brain heart infusion (BHI) broth overnight at 37°C to optical density of ∼0.6, transferred to BHI/20% glycerol, aliquoted, and stored at −80°C until used.20 Samples were thawed at 37°C and plated on BHI agar for colony forming units per milliliter estimation.
Cells and cell culture
Human leukemia monocytic THP-1 cell line was obtained from the American Type Culture Collection (TIB-202) and maintained in RPMI with 2-mM l-glutamine and 10% fetal bovine serum (C-RPMI) at 3 to 8 × 105 cells/mL.21 Myeloid differentiation factor 88 (MyD88)–deficient THP-1 cells (ΔMyD88) were obtained from Invivogen (San Diego, CA) and cultured as the parental strain.
Human participants and human PBMC isolation
Deidentified healthy human volunteers were recruited at the University of Georgia to donate venous blood. The studies were performed according to the guidelines of the World Medical Association Declaration of Helsinki. Enrolled blood donors signed consent forms as described previously.22 The human blood protocol (UGA# 2012-10769) and the associated consent form were reviewed and approved by the institutional review board of the University of Georgia. Coagulation was prevented with heparin, and red blood cells were removed by dextran sedimentation (GE Healthcare). The leukocyte-rich supernatant was washed 2 times in sterile phosphate-buffered saline (PBS). Peripheral blood mononuclear cells (PBMCs) were isolated using a 5-step Percoll gradient centrifugation, collected from the 65% Percoll/PBS interphase, and washed twice with PBS subsequently. Cell viability was >98% as assessed by Trypan Blue dye exclusion assay.
Chemical reagents
Phorbol 12-myristate-13-acetate (PMA), synthetic diacylated (Pam2CSK4) and triacylated (Pam3CSK4) lipopeptides, polyinosinic-polycytidylic acid (poly I:C), Escherichia coli O111:B4 ultrapure LPS, Salmonella enterica serovar Typhimurium flagellin, synthetic lipoprotein FSL1, imidazoquinoline (R848), and class A CpG oligonucleotide (ODN2216) were purchased from Invivogen. Ammonium iron citrate (FeAC) was obtained from ChemCruz (Santa Cruz Biotech, Santa Cruz, CA).
Macrophage differentiation and TLR stimulation
For differentiation into a macrophage-like phenotype, parent and ΔMyD88 monocyte–like THP-1 cells were pelleted by centrifugation at 0.2g for 5 minutes, resuspended in C-RPMI with 50 nM of PMA at 1 × 106 cells/mL, and seeded in 48-well tissue culture plates (Costar, Corning, NY) for 24 hours at 37°C and 5% carbon dioxide. After differentiation, monolayers were washed twice with PBS to remove loosely adherent cells and rested overnight in C-RPMI 10% FBS supplemented with 100 µM of FeAC (unless otherwise stated) at 37°C and 5% carbon dioxide. After resting, macrophages were stimulated with different TLR ligands at concentrations described in supplemental Table 1.
For differentiation of primary human monocyte–derived macrophages (MDMs), we purified monocytes from human PBMCs by plastic adherence and differentiated them into macrophages with macrophage colony-stimulating factor for 5 days as previously described.23,24
Macrophage infection
Three hundred thousand monocyte-like THP-1 cells were differentiated in 48-well plates and rested, as described in “Macrophage differentiation and TLR stimulation,” in C-RPMI/FeAC overnight. The monolayers were then infected for 2 hours with BCG bacilli at a multiplicity of infection of 10 (10 bacteria per host cell) and for 1 hour with L monocytogenes bacilli at a multiplicity of infection of 5. The BCG-infected cells were incubated at 37°C for 72 hours and L monocytogenes–infected cells for 6 hours in C-RPMI/FeAC with 50 μg/mL of gentamicin. Fifty thousand human primary macrophages were infected as described in “Macrophage differentiation and TLR stimulation” in 96-well plates with M tuberculosis Erdman.
Isolation of messenger RNA and quantitative reverse transcription PCR
Total cellular RNA from 1 × 106 PMA-differentiated monocyte-like THP-1 cells was extracted with TRIzol (Invitrogen Thermo Fisher Scientific, Waltham, MA) using the manufacturer instructions and reverse transcribed into complementary DNA using the SuperscriptIII First-Strand cDNA Synthesis Kit (Invitrogen Thermo Fisher Scientific) using poly dT20 primers. Quantitative polymerase chain reaction (PCR) was performed using Bio-Rad IQ SYBR green supermix (Bio-Rad) in an iQ5 Real-Time PCR Detection System. All values were normalized against glyceraldehyde-3-phosphate dehydrogenase (GAPDH; ΔCT = CT [HAMP] − CT [GAPDH]). Fold change was calculated as 2−ΔΔCT, where ΔΔCT = ΔCT (test sample) − ΔCT (control). The primer sequences for the genes examined were as follows: human hepcidin (HAMP): forward, 5 = -GGATGCCCATGTTCCAGAG-3 =; reverse, 5 = -AGCACATCCCACACTTTGAT-3 =; human GAPDH: forward, 5 = -GCCCTCAACGACCACTTTGT-3 =; reverse, 5 = -TGGTGGTCCAGGGGTCTTAC-3 =; human ferroportin: forward, 5 = -CACAACCGCCAGAGAGGATG-3 =; reverse, 5 = -ACCAGAAACACAGACACCGC-3 =; human ferritin: forward, 5 = -AGAACTACCACCAGGACTCA-3 =; reverse, 5 = -TCATCGCGGTCAAAGTAGTAAG-3 =; human IL-6: forward, 5 = -CACAGACAGCCACTCACCTC-3 =; reverse, 5 = -AGCTCTGGCTTGTTCCTCAC-3 =; and human IL-8: forward, 5 = -TCTGCAGCTCTGTGTGAAGGTG-3 =; reverse, 5 = -AATTTCTGTGTTGGCGCAGTG-3 =.
Western blot
One million monocyte-like THP-1 cells were grown and differentiated in 6-well plates, washed twice with ice-cold PBS, and lysed with ice-cold immunoprecipitation lysis buffer for 30 minutes while placed on ice. Cell lysates were further disrupted manually by vigorous pipetting and vortexing. After centrifugation at 10 000g for 15 minutes at 4°C, supernatants were collected and stored at −20°C until analyzed.
Total protein concentration was determined by BCA protein quantification. Samples (20 μg) were mixed with Laemmli buffer (1× final concentration) and heated at 70°C for 10 minutes. Proteins were electrophoretically separated on a 15% sodium dodecyl sulfate polyacrylamide gel. Total protein was transferred to a PVDF membrane (Bio-Rad), which was then preincubated with blocking solution (5% nonfat dry milk in Tris-buffered saline containing 0.01% Tween 20; pH, 7.4) for 1 hour, followed by overnight incubation with 1 μg of antiferritin1 rabbit monoclonal antibody (Cell Signaling Tech, Danvers, MA) and 1 µg of anti-GAPDH rabbit monoclonal antibody (Cell Signaling Tech) at 4°C. After primary incubation, the membrane was washed 3 times with Tris-buffered saline containing 0.01% Tween 20 and incubated for 1 hour with secondary anti-rabbit HRP-conjugated antibody (Cell Signaling Tech).
All incubations and wash steps were performed at room temperature except when otherwise stated. Cross-reactivity was visualized by using enhanced chemiluminescence (SuperSignalWestPico; Pierce) and quantified using QuantityOne application software (Bio-Rad, Hercules, CA).
Prussian blue staining
Four hundred thousand monocyte-like THP-1 cells were grown and differentiated in 8-well chamber microscopy slides as described in “Western blot.” After stimulation with TLR ligands, cells were fixed with 4% formaldehyde in PBS for 10 minutes at room temperature, washed with PBS, and stained twice with a 1:1 solution of 4% hydrochloric acid and 4% potassium ferrocyanide for 25 minutes (Polysciences Prussian blue stain kit). After washing with PBS, cells were counterstained with filtered 1% Nuclear Fast Red solution for 5 to 10 minutes. After gentle washing with PBS and distilled water, slides were mounted and imaged with an Axiovert 40CFL microscope, and images were acquired with an Axiocam MRC5 color camera at magnifications of 200× and 400×.
Immunofluorescence microscopy
Antiferroportin antibodies for surface and total ferroportin detection were kindly provided by Tara Arvedson (Amgen Inc., Thousand Oaks, CA). Immunofluorescence staining was performed as previously described.25 Briefly, 2 × 105 THP-1 cells were seeded and differentiated in 8- or 16-chamber microscopy slides and treated with TLR ligands as described in “Prussian blue staining.” For ferroportin staining, cells were incubated with 2 μg/mL of mouse antibody diluted in C-RPMI. For detection, cells were incubated with 2 μg/mL of goat anti-mouse labeled with alexa-fluor-488 (Invitrogen Thermo Fisher Scientific). Incubation was performed at 4°C for 2 hours. Cells were gently washed 3 times, fixed with 4% formaldehyde in PBS for 10 minutes, permeabilized with 0.1% Triton X-100, and counterstained with 4′,6-diamidino-2-phenylindole. Slides were imaged on a Zeiss Axiovert 200M microscope at magnifications of 400× and 630×, and images were acquired with an Axiocam MRm grayscale camera.
Flow cytometry and intracellular staining
The mouse anti-human hepcidin antibody was kindly provided by Tara Arvedson (Amgen Inc.); its specificity has been previously validated.26 One million THP-1 monocytic cells were seeded and differentiated into 24-well plates, treated with TLR ligands as described in “Immunofluorescence microscopy” and with 1 µg/mL of Golgi plug (BD Fisher) for another 5 hours to arrest Golgi transport. Cells were trypsinized, fixed, and permeabilized with Fix&Perm buffer (BD Fisher, Grand Island, NY) according to manufacturer instructions. Intracellular hepcidin was stained with 3 µg of mouse anti-human hepcidin monoclonal primary antibody (mAb2.7) for 1 hour, detected with goat anti-mouse alexa-fluor-488 (Invitrogen, San Diego, CA), and analyzed on an LSRII flow cytometer (BD Biosciences, San Jose, CA). All dilutions were performed in permeabilization wash buffer (BD Fisher, Grand Island, NY). Data were analyzed with FlowJo fluorescence-activated cell sorting analysis software V7.6.5.
Intracellular labile iron pool quantification
The intracellular labile iron pool was measured using a calcein quenching assay as previously described27 and adapted for flow cytometry analysis. Briefly, 1 × 103 THP-1 monocytic cells were seeded and differentiated in 48-well plates and treated with LPS or Pam3Csk4 up to 48 hours in iron-supplemented medium. At each time point, cells were washed twice with warm PBS, stained with calcein-AM (Invitrogen Thermo Fisher Scientific) for 15 minutes at room temperature, washed again with warm PBS, trypsinized, resuspended in fluorescence-activated cell sorting buffer, and analyzed by flow cytometry before and after iron chelation with deferiprone (DFP). Quenched fluorescence was determined as percentage of mean fluorescence intensity (MFI) before iron chelation (xMFI) to 10 minutes after addition of DFP (xMFIDFP): (xMFI/xMFIDFP) × 100. Cells grown in non–iron-supplemented medium were used as negative controls.
Results
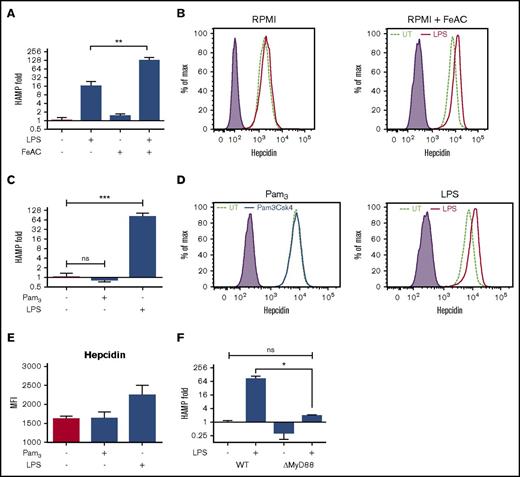
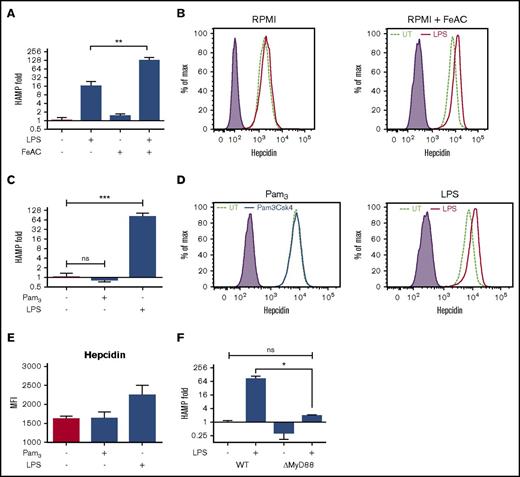
Iron increases LPS-mediated hepcidin induction
Hepcidin is regulated by 2 major pathways: iron metabolism and inflammation. To evaluate the interaction between these 2 pathways in human myeloid cells, specifically macrophages, THP-1 monocytic cells were differentiated into macrophage-like phenotype with PMA and stimulated with LPS for 24 hours in C-RPMI or in iron-containing medium (DMEM-F12). Hepcidin messenger RNA (mRNA) levels demonstrated a 16-fold induction after LPS stimulation in C-RPMI, but interestingly, this effect was further amplified up to 128-fold in DMEM-F12 when compared with the respective untreated control (supplemental Figure 1). To test if iron alone was responsible for this difference, we compared hepcidin basal mRNA levels in differentiated THP-1 cells in the presence or absence of iron supplementation and observed that iron alone had no significant impact on hepcidin expression levels in THP-1 cells (Figure 1A). These results led to the conclusion that LPS-mediated induction of hepcidin is more prominent in the presence of iron in cell culture medium, which more closely resembles the physiological conditions in mammalian serum. To confirm that these changes in mRNA levels translate into protein expression levels, we next assessed hepcidin concentrations in cells by intracellular staining. Our results indicated that LPS-mediated hepcidin synthesis was more prominent in the presence of iron (Figure 1B).
Iron increases TLR4-mediated hepcidin expression, whereas TLR2 activation does not induce hepcidin expression. (A) THP-1 human monocytic cells were differentiated with 50 nM of PMA and rested overnight in C-RPMI or C-RPMI supplemented with 100 μM of ferric ammonium citrate (FeAC) and then stimulated for 24 hours with 500 ng/mL of ultrapure LPS. (B) Differentiated THP-1 cells were treated as in panel A and stained for intracellular hepcidin using human antihepcidin antibody (mAb2.7) and analyzed by flow cytometry. (C) Differentiated THP-1 cells were treated with TLR2 ligand (Pam3CSK4) or TLR4 ligand (ultrapure LPS) for 24 hours, and hepcidin expression was quantified by quantitative reverse transcription PCR (qRT-PCR). (D-E) Macrophages treated as in panel C for 24 hours were stained for intracellular hepcidin using human antihepcidin antibody (mAb2.7) and analyzed by flow cytometry. Hepcidin expression was quantified by MFI. (E) Summary data from 3 independent experiments as represented in panel D. (F) Hepcidin expression in MyD88-deficient THP-1 (THP-1 ΔMyD88) cells treated with LPS as in panel A was measured by qRT-PCR. Hepcidin expression levels were analyzed by qRT-PCR, and GAPDH expression was used as a control. *P < .05, **P < .01, ***P < .001. All data were from 3 independent experiments. ns, not significant; UT, untreated; WT, wild type.
Iron increases TLR4-mediated hepcidin expression, whereas TLR2 activation does not induce hepcidin expression. (A) THP-1 human monocytic cells were differentiated with 50 nM of PMA and rested overnight in C-RPMI or C-RPMI supplemented with 100 μM of ferric ammonium citrate (FeAC) and then stimulated for 24 hours with 500 ng/mL of ultrapure LPS. (B) Differentiated THP-1 cells were treated as in panel A and stained for intracellular hepcidin using human antihepcidin antibody (mAb2.7) and analyzed by flow cytometry. (C) Differentiated THP-1 cells were treated with TLR2 ligand (Pam3CSK4) or TLR4 ligand (ultrapure LPS) for 24 hours, and hepcidin expression was quantified by quantitative reverse transcription PCR (qRT-PCR). (D-E) Macrophages treated as in panel C for 24 hours were stained for intracellular hepcidin using human antihepcidin antibody (mAb2.7) and analyzed by flow cytometry. Hepcidin expression was quantified by MFI. (E) Summary data from 3 independent experiments as represented in panel D. (F) Hepcidin expression in MyD88-deficient THP-1 (THP-1 ΔMyD88) cells treated with LPS as in panel A was measured by qRT-PCR. Hepcidin expression levels were analyzed by qRT-PCR, and GAPDH expression was used as a control. *P < .05, **P < .01, ***P < .001. All data were from 3 independent experiments. ns, not significant; UT, untreated; WT, wild type.
It has been demonstrated that TLR2 recognizes lipoteichoic acid, peptidoglycan, and lipoproteins of gram-positive bacteria.28 In addition, TLR2 is well known for recognition of mycobacterial lipoproteins. To evaluate whether TLR2 activation induces hepcidin expression in myeloid cells similar to TLR4 activation by LPS, we stimulated macrophages with Pam3CSK4 (synthetic TLR2 ligand) in iron-supplemented medium for 24 hours. Hepcidin mRNA levels showed that unlike LPS, Pam3CSK4 does not induce hepcidin expression in PMA-differentiated THP-1 monocytic cells (Figure 1C). Furthermore, intracellular hepcidin protein levels were similar between untreated and Pam3CSK4-treated cells (Figure 1D-E).
Activation of both TLR2 and TLR4 induces a signal through MyD88, and TLR4 can also signal intracellularly through TRIF3.29 Thus, we next assessed if LPS-mediated hepcidin induction is dependent on MyD88-mediated signaling. MyD88-deficient THP-1 cells were stimulated with LPS for 24 hours in iron-supplemented medium. As shown in Figure 1E, MyD88-deficient macrophages demonstrated a significantly decreased hepcidin induction (twofold compared with 64-fold in wild-type macrophages) against the respective untreated control. It is interesting to note that MyD88-deficient THP-1 cells already showed decreased hepcidin basal levels and that after LPS stimulation demonstrated similar hepcidin mRNA levels as wild-type untreated cells (Figure 1F).
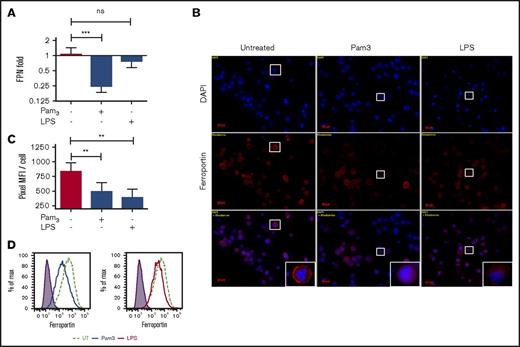
TLR2 downregulates ferroportin
Because hepcidin acts through ferroportin internalization and degradation, we next evaluated the impact of TLR2 and TLR4 signaling on ferroportin expression in macrophages. Our results showed that TLR4 ligand has no effect on ferroportin mRNA levels, whereas TLR2 activation by Pam3CSK4 significantly decreased ferroportin expression nearly threefold (Figure 2A). This downregulation corresponds to a significant decrease in surface ferroportin at protein levels similar to those resulting from LPS-mediated hepcidin expression (Figure 2B-C). Intracellular iron sequestration in macrophages is associated with decreased ferroportin levels in the cell membrane. To quantify the differences in total or surface ferroportin expression, differentiated THP-1 cells stimulated with Pam3CSK4 or LPS for 24 hours were surface stained and analyzed by flow cytometry. Consistent with our microscopic observations, regardless of its impact on hepcidin expression, TLR2 activation significantly decreases surface ferroportin levels similarly to LPS-treated cells (Figure 2D). Monocytic cell lines such as THP-1 may not always mimic the natural response of primary human macrophages. However, our data indicated that human primary MDMs respond similarly to PMA-treated THP-1 macrophage-like cells in regard to TLR4-mediated hepcidin induction (supplemental Figure 2A). Moreover, human MDMs significantly induce hepcidin production in response to M tuberculosis infection (supplemental Figure 2B). Future studies should expand the observations here reported with a human monocytic cell line to human primary myeloid cells and confirm the importance of hepcidin expression and intracellular iron sequestration in macrophages during infection with intracellular pathogens.
TLR2 ligand inhibits ferroportin expression. (A) THP-1 cells were stimulated with TLR2 or TLR4 ligand, and ferroportin expression was quantified by qRT-PCR. GAPDH expression was used as a control. (B) Surface ferroportin staining in THP-1 cells treated with TLR2 or TLR4 ligands was assessed by immunofluorescence microscopy (original magnification ×630). (C) MFI was assessed from 5 microscopic fields in panel B. (D) Surface ferroportin expression in THP-1 cells treated with TLR2 or TLR4 ligands compared with untreated cells was assessed by flow cytometry. All data were from 3 independent experiments. **P < .01, ***P < .001. DAPI, 4′,6-diamidino-2-phenylindole; FPN, ferroportin.
TLR2 ligand inhibits ferroportin expression. (A) THP-1 cells were stimulated with TLR2 or TLR4 ligand, and ferroportin expression was quantified by qRT-PCR. GAPDH expression was used as a control. (B) Surface ferroportin staining in THP-1 cells treated with TLR2 or TLR4 ligands was assessed by immunofluorescence microscopy (original magnification ×630). (C) MFI was assessed from 5 microscopic fields in panel B. (D) Surface ferroportin expression in THP-1 cells treated with TLR2 or TLR4 ligands compared with untreated cells was assessed by flow cytometry. All data were from 3 independent experiments. **P < .01, ***P < .001. DAPI, 4′,6-diamidino-2-phenylindole; FPN, ferroportin.
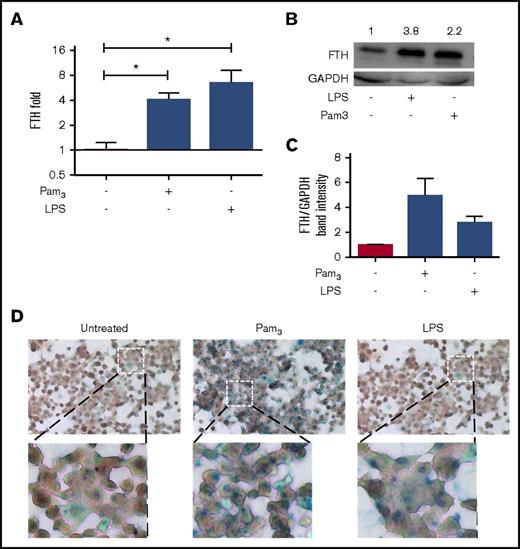
TLR2 signaling leads to increased intracellular iron sequestration
As discussed, hepcidin and ferroportin are key players in intracellular iron sequestration. Ferritin protein acts as a carrier for intracellular iron; thus, cytosolic ferritin is a good correlate of intracellular iron pool levels.30 Because TLR2/6 directly downregulate ferroportin, we hypothesized that addition of these ligands would also lead to intracellular iron sequestration and increased ferritin expression in macrophages. Differentiated THP-1 cells were stimulated with LPS or Pam3CSK4 for 24 hours, and ferritin gene expression was assessed by qRT-PCR. Our data showed that activation of TLR2 and TLR4 significantly upregulates (four- to eightfold) ferritin expression compared with untreated controls (Figure 3A). Furthermore, ferritin mRNA levels also correlated with intracellular ferritin protein levels (Figure 3B-C).
TLR2 induces intracellular iron sequestration through a hepcidin-independent mechanism. (A) Ferritin mRNA transcription levels from PMA-differentiated THP-1 cells treated with TLR2 or TLR4 ligands for 24 hours quantified by qRT-PCR and normalized against untreated controls. GAPDH expression was used as a relative control. (B) THP-1 cells treated as in panel A and cell lysates were subjected to immunoblotting with the antiferritin (anti-FTH) antibody. (C) Densitometry analysis from western blot in panel B. (D) Prussian blue staining of PMA-differentiated THP-1 cells treated as described in panel A. Low magnification field (×10) is shown above, with high magnification (×40) shown below. All data were from 3 independent experiments. *P < .05.
TLR2 induces intracellular iron sequestration through a hepcidin-independent mechanism. (A) Ferritin mRNA transcription levels from PMA-differentiated THP-1 cells treated with TLR2 or TLR4 ligands for 24 hours quantified by qRT-PCR and normalized against untreated controls. GAPDH expression was used as a relative control. (B) THP-1 cells treated as in panel A and cell lysates were subjected to immunoblotting with the antiferritin (anti-FTH) antibody. (C) Densitometry analysis from western blot in panel B. (D) Prussian blue staining of PMA-differentiated THP-1 cells treated as described in panel A. Low magnification field (×10) is shown above, with high magnification (×40) shown below. All data were from 3 independent experiments. *P < .05.
To confirm that increased ferritin expression correlates with increased intracellular iron sequestration, Prussian blue staining was performed to assess total cellular iron content. Our results demonstrated that both TLR2 and TLR4 activation lead to intracellular iron sequestration (Figure 3D). Our results also confirmed that TLR2 promotes intracellular iron sequestration by directly downregulating ferroportin gene transcription; however, the molecular mechanism of TLR2-mediated ferroportin downregulation is unknown and needs to be investigated.
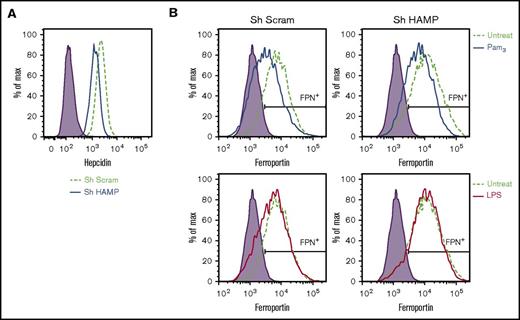
TLR2 inhibits ferroportin expression independent of hepcidin
To confirm that TLR2 activation mediates ferroportin downregulation through a hepcidin-independent mechanism, the hepcidin gene (HAMP) was silenced using a hepcidin-specific lentiviral short hairpin RNA (shRNA; Figure 4A). Nonspecific scramble lentiviral shRNA was used as a negative control. After achieving efficient lentiviral shRNA–mediated gene silencing in THP-1 monocytic cell line, cells were treated with LPS and Pam3CSK4 for 24 hours, and expression of ferroportin was evaluated by flow cytometry. Our results demonstrated that TLR2 activation equally downregulates ferroportin expression in both control and hepcidin-specific shRNA-silenced macrophages (Figure 4B). In contrast, TLR4 activation in hepcidin-specific shRNA-silenced macrophages has no impact on surface ferroportin levels compared with untreated controls (Figure 4B). These results further indicate that TLR2 activation dysregulates iron homeostasis mainly by downregulation of ferroportin gene expression in human macrophages.
TLR2 inhibits ferroportin expression independent of hepcidin. Hepcidin gene silencing in THP-1 cells was achieved by lentiviral-based shRNA transduction. Scramble shRNA (Sh Scram) was used as a negative control. (A) Hepcidin expression in Sh Scram and hepcidin-specific shRNA (Sh HAMP) silenced THP-1 cells. (B) Surface ferroportin expression in Sh Scram and Sh HAMP THP-1 cells after Pam3CSK4 or LPS treatment for 24 hours. All data were from 3 independent experiments.
TLR2 inhibits ferroportin expression independent of hepcidin. Hepcidin gene silencing in THP-1 cells was achieved by lentiviral-based shRNA transduction. Scramble shRNA (Sh Scram) was used as a negative control. (A) Hepcidin expression in Sh Scram and hepcidin-specific shRNA (Sh HAMP) silenced THP-1 cells. (B) Surface ferroportin expression in Sh Scram and Sh HAMP THP-1 cells after Pam3CSK4 or LPS treatment for 24 hours. All data were from 3 independent experiments.
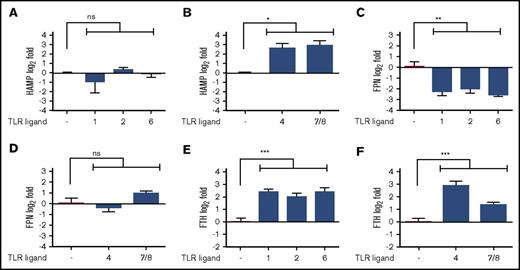
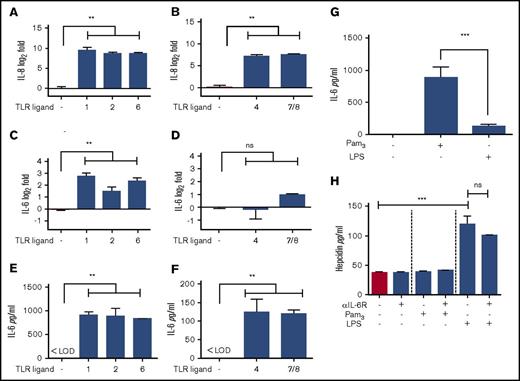
TLR signaling can induce hypoferremia through 2 independent pathways
To determine if the abovementioned iron sequestration mechanisms are restricted to TLR2 and TLR4 activation by Pam3CSK4 and LPS, respectively, or if these can be expanded to the activation of other TLRs, PMA-differentiated THP-1 cells were stimulated with each individual TLR ligand for 24 hours and hepcidin, ferroportin, and ferritin mRNA assessed by qRT-PCR. According to the gene expression profiles of hepcidin, ferroportin, and ferritin, the TLRs could be grouped into hepcidin inducers (TLR4, TLR7/8) and ferroportin downregulators (TLR1, TLR2, TLR6; Figure 5A-F). Activation by TLR3, TLR5, and TLR9 does not induce hepcidin or downregulate ferroportin and has no impact on ferritin expression; thus, these were considered noniron regulators (supplemental Figure 3). All TLR ligands except TLR3, TLR5, and TLR9 (poly I:C, flagellin, and ODN2216, respectively) induce ferritin expression up to threefold. Furthermore, differentiated THP-1 moncytic cells treated with either TLR3 or TLR5 ligand show no increase in total intracellular iron levels or in the intracellular labile iron pool, as observed by Prussian blue staining and the calcein quenching assay, respectively (data not shown). Nonetheless, despite having no impact alone, TLR3 activation can significantly downregulate ferroportin expression in combination with LPS, indicating that during infection, even noniron regulator TLRs (TLR3, TLR5, and TLR9) might play a role in intracellular iron sequestration (supplemental Figure 2).
TLR signaling induces hypoferremia through 2 independent pathways. (A-B) Hepcidin expression in THP-1 cells treated with different TLR ligands and organized to show hepcidin noninducers (A) and hepcidin inducers (B). (C-D) Ferroportin (FPN) expression in THP-1 cells treated with TLR ligands and organized as in panels A and B. (E-F) Ferritin (FTH) expression in THP-1 cells treated with different TLR ligands and organized as in panels A and B. All data were from 3 independent experiments. *P < .05, **P < .01, ***P < .001.
TLR signaling induces hypoferremia through 2 independent pathways. (A-B) Hepcidin expression in THP-1 cells treated with different TLR ligands and organized to show hepcidin noninducers (A) and hepcidin inducers (B). (C-D) Ferroportin (FPN) expression in THP-1 cells treated with TLR ligands and organized as in panels A and B. (E-F) Ferritin (FTH) expression in THP-1 cells treated with different TLR ligands and organized as in panels A and B. All data were from 3 independent experiments. *P < .05, **P < .01, ***P < .001.
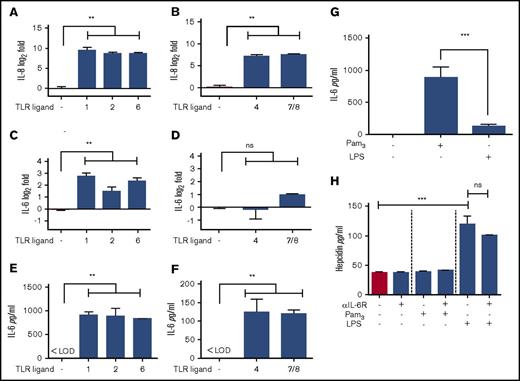
Hepcidin expression in macrophages is independent of IL-6 signaling
Hepcidin expression during infection is mostly IL-6 dependent in hepatocytes.13,31 Therefore, we speculate that after TLR stimulation, macrophages release proinflammatory cytokines such as IL-6 and IL-8, which could be involved in TLR activation–mediated hepcidin expression. To explore this hypothesis, macrophages were treated with different TLRs for 24 hours as stated in “TLR signaling can induce hypoferremia through 2 independent pathways,” and gene transcription of IL-6 and IL-8 was evaluated by RT-PCR. Surprisingly, TLR1, TLR2, and TLR6, which do not induce hepcidin, showed 16 times more IL-6 expression than the untreated control, whereas TLR4 and TLR7/8, which do induce hepcidin, did not generate any changes in IL-6 expression levels (Figure 6C-D). In addition, IL-6 secretion in culture supernatants of macrophages treated with TLRs was consistent with IL-6 gene expression profile (Figure 6E-G). To further demonstrate that hepcidin induction is indeed IL-6 independent in macrophages, THP-1 cells were stimulated with LPS and Pam3CSK4 in the presence of an IL-6 receptor–blocking antibody. As hypothesized, IL-6 blocking does not affect hepcidin expression in response to LPS, and Pam3CSK4 was unable to induce hepcidin expression in macrophages regardless of the presence of the IL-6 receptor–blocking antibody (Figure 6H).
TLR-mediated hepcidin induction is independent of IL-6 signaling. (A-B) IL-8 expression in TLR-treated macrophages and organized to show hepcidin noninducers (A) and hepcidin inducers (B). (C-D) IL-6 expression in TLR-treated macrophages and organized as in panels A and B. (E-F) IL-6 secretion in TLR-treated macrophages and organized as in panels A and B. (G) IL-6 secretion in macrophages treated with Pam3CSK4 or LPS for 24 hours. (H) Hepcidin secretion in macrophages treated with Pam3CSK4 or LPS for 24 hours in presence of 1 μg/mL of IL-6 receptor–blocking antibody. All data were from 3 independent experiments. **P < .01, ***P < .001. LOD, limit of detection.
TLR-mediated hepcidin induction is independent of IL-6 signaling. (A-B) IL-8 expression in TLR-treated macrophages and organized to show hepcidin noninducers (A) and hepcidin inducers (B). (C-D) IL-6 expression in TLR-treated macrophages and organized as in panels A and B. (E-F) IL-6 secretion in TLR-treated macrophages and organized as in panels A and B. (G) IL-6 secretion in macrophages treated with Pam3CSK4 or LPS for 24 hours. (H) Hepcidin secretion in macrophages treated with Pam3CSK4 or LPS for 24 hours in presence of 1 μg/mL of IL-6 receptor–blocking antibody. All data were from 3 independent experiments. **P < .01, ***P < .001. LOD, limit of detection.
The cytokine IL-8 is frequently associated with early response to bacterial infection32 and inflammatory hypoferremia,33 although a direct association between this cytokine and hepcidin has not been established. To determine if IL-8 is associated with TLR-mediated intracellular iron sequestration in macrophages, IL-8 mRNA levels were assessed by qRT-PCR in PMA-differentiated monocyte-like THP-1 cells stimulated with different TLR ligands. As expected, both LPS and Pam3CSK4 induced IL-8 to the same extent (approximately sevenfold induction), whereas poly I:C, which has no impact on intracellular iron sequestration, promoted no changes in IL-8 mRNA levels compared with untreated controls (data not shown). These results demonstrate that iron sequestration in macrophages can be directly modulated by TLR signaling, and the cytokines previously associated with hepcidin induction (IL-6 and IL-8) have a minimal impact.
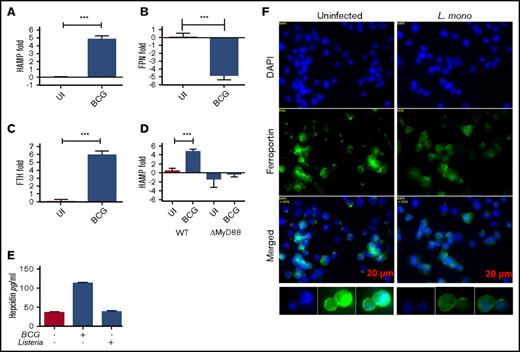
Redundant role of hepcidin during intracellular bacterial infection–mediated intracellular iron sequestration
To understand the biological relevance of the abovementioned mechanisms, the role of hepcidin in iron sequestaration during intracellular bacterial infection was determined. M bovis BCG infection induced intracellular iron sequestration as measured indirectly by ferritin level (Figure 7C). BCG activates both TLR2 and TLR4 signaling,34 and as with pure ligands, BCG infection induces hepcidin expression and inhibits ferroportin expression to promote intracellular iron sequestration in macrophages (Figure 7A-B). However, infection with L monocytogenes bacilli, gram-positive bacteria that prominently activate TLR2, does not induce hepcidin expression but downregulates ferroportin expression and subsequently promotes iron sequestration within the macrophages (Figure 7E-F). Furthermore, the role of MyD88 in hepcidin expression during BCG infection was assessed. As expected, when compared with the control parental strain, MyD88-deficient THP-1 cells had decreased hepcidin expression 24 hours after BCG infection (Figure 7D), confirming the role of TLR signaling in BCG-mediated hepcidin induction.
BCG induces iron sequestration through hepcidin induction and ferroportin downregulation. (A-C) Transcriptional changes of hepcidin (A), ferroportin (B), and ferritin (C) expression in BCG-infected THP-1 cells differentiated with 50 nM of PMA for 24 hours. (D) Hepcidin mRNA levels of BCG-infected WT and ΔMyD88 THP-1 cells. (E) Hepcidin secretion in BCG- or L monocytogenes (L mono)–infected THP-1 cells differentiated as in panel A. (F) Ferroportin expression in L mono–infected THP-1 cells. All data were from 3 independent experiments. ***P < .001.
BCG induces iron sequestration through hepcidin induction and ferroportin downregulation. (A-C) Transcriptional changes of hepcidin (A), ferroportin (B), and ferritin (C) expression in BCG-infected THP-1 cells differentiated with 50 nM of PMA for 24 hours. (D) Hepcidin mRNA levels of BCG-infected WT and ΔMyD88 THP-1 cells. (E) Hepcidin secretion in BCG- or L monocytogenes (L mono)–infected THP-1 cells differentiated as in panel A. (F) Ferroportin expression in L mono–infected THP-1 cells. All data were from 3 independent experiments. ***P < .001.
Discussion
In this study, we have shown that TLR activation with purified ligands leads to iron sequestration in human macrophages. Indeed, M bovis BCG and L monocytogenes PAMPs interact with TLRs and activate TLR-mediated signal transduction, leading to increased iron sequestration in macrophages. The potential role of TLRs in regulating macrophage iron status through ferroportin downregulation and hepcidin induction, 2 key regulators of iron homeostasis in humans, was explored.
This study presents for the first time a comprehensive evaluation of TLR mediation of iron homeostasis in differentiated THP-1 human monocytic cells. It has been shown that the macrophage iron modulatory response differs relative to the TLR stimulus provided. TLR1, TLR2, and TLR6 activation by their respective synthetic ligands generates intracellular iron sequestration by directly downregulating iron transporter ferroportin at the transcriptional level, whereas TLR4 and TLR7/8 activation increases hepcidin expression, resulting in internalization and degradation of ferroportin in the proteasome.35 Despite both mechanisms leading to increased intracellular iron levels and decreased extracellular iron availability, these constitute 2 independent yet redundant pathways activated during intracellular infection in macrophages.
Our results are in agreement with a previously published study by Guida et al,18 who demonstrated that TLR2/6 signaling induces hypoferrimia through a hepcidin-independent mechanism. In murine hepatocytes and macrophages, LPS treatment decreases intracellular iron sequestration both through hepcidin-dependent and -independent mechanisms18,36 ; however, chronic TLR4 stimulation also prominently activates NRF2,37 which can counteract TLR4-supressed ferroportin expression.38 Hepcidin controls the absorption of dietary iron as well as the distribution of iron between intracellular stores and extracellular fluids, including plasma.6 During extracellular infections, increased hepcidin concentrations and associated hypoferremia are thought to be host defense mechanisms that decrease the amount of iron available to extracellular microbial pathogens, thereby restricting their growth. Although hepcidin-induced hypoferremia may protect against extracellular infections, hepcidin activity and associated shifts in iron compartmentalization may differentially affect pathogens that use alternative niches, such as intracellular M tuberculosis and HIV. Kerkhoff et al32 conducted a cohort study and found that serum hepcidin concentrations increased with anemia severity and mycobacterial burden during coinfection with HIV and M tuberculosis. In this study, investigators generated multivariable Cox regression models, in which hepcidin was found to be an independent predictor of mortality in M tuberculosis–positive, HIV-infected patients.39 Therefore, one can speculate that hepcidin is intimately involved with the pathogenic processes occurring during HIV-associated tuberculosis; however, the cellular mechanism of hepcidin expression in coinfection with M tuberculosis and HIV has not been fully investigated.
Expression of hepcidin by hepatocytes is stimulated by IL-613,14,31 and bone morphogenetic protein (BMP)15,40 signaling pathways. Our data have shown that LPS-mediated hepcidin expression by human myeloid cells (macrophages) is not dependent on IL-6 or BMP/SMAD signaling pathways. Indeed, it has been reported that murine macrophages did not increase hepcidin expression in response to BMP stimulation alone.41 Our data are consistent with these earlier reports. Further investigation is needed to evaluate the cell regulatory pathways involved with hepcidin expression in human macrophages mediated by pathogens and PAMPs.
The full-text version of this article contains a data supplement.
Acknowledgments
The authors thank Tara Arvedson (Amgen Inc.) for providing hepcidin and ferroportin monoclonal antibodies. The authors also thank Shelly Helms for technical assistance in several parts of this project.
This work was supported in part by an endowment from the University of Georgia Athletic Association (F.Q.). R.A. is supported by Fulbright PhD scholarships 11/278.
Authorship
Contribution: R.A. designed research, performed research, analyzed data, and wrote the paper; F.Q. provided guidance and wrote the paper; and P.K.G. designed research, analyzed data, provided guidance, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Pramod K. Giri, Department of Infectious Diseases, College of Veterinary Medicine, University of Georgia, 501 D. W. Brooks Dr, Athens, GA 30602; e-mail: pgiri@uga.edu.