Introduction
Recent advances have realized the decades-old desire to harness the power of the immune system to eradicate malignant cells. It is now indisputable that immunotherapy can provide benefits for cancer patients that cannot be achieved with traditional cancer therapeutics. The potency of immunotherapy has been particularly notable in B-cell acute lymphoblastic leukemia (B-ALL), where chimeric antigen receptors (CARs) targeting CD19 and the CD3-CD19 bispecific T-cell engager blinatumomab both demonstrate impressive effects. Once a pipe dream, clinicians are now faced with a choice of immunotherapies to offer patients with relapsed or refractory B-ALL, presenting a new challenge: how to choose the best immunotherapy approach. Herein we provide a commentary on the relative merits and challenges of CD19-CAR T cells vs blinatumomab for relapsed/refractory B-ALL based on currently available data, focused on response rates, feasibility, toxicity, activity in extramedullary disease, and durability of effects. We acknowledge that other targets, including CD22, are promising for immunotherapy of B-ALL, with impressive remission rates recently reported with inotuzumab ozogomycin.1 However, because first-in-human studies of CD22-directed CAR T cells are ongoing and have not yet been published, our discussion on the relative merits of CAR therapeutics for B-ALL are necessarily limited to those targeting CD19.
Which CD19-directed therapy is more effective in inducing complete remission?
Randomized, controlled trials comparing the efficacy of CD19-CAR vs blinatumomab in relapsed/refractory B-ALL are not available, and may not be in the foreseeable future, precluding a definitive answer to this question. Several published studies clearly demonstrate that patients receiving CD19-CAR therapies have a high likelihood of being rendered into remission, with 4 separate groups reporting complete response (CR) rates of 70% to >90% following CAR T-cell therapy. Yet, caution should be used in interpreting this data because response rates to CAR T cells can be misleading if a sizable fraction of eligible patients do not actually receive the therapy as a result of inability to generate or administer a cellular product. Similar challenges have long plagued comparisons of stem cell transplant (SCT) and chemotherapy for treatment of relapsed/refractory leukemia and have been discussed at length in the literature.2 One intent-to-treat phase 1 study, which mitigates this problem to some extent, demonstrated a 70% CR rate (confidence interval [CI], 45.7% to 88.1%) in B-ALL.3 As summarized in Table 1, 2 phase 2 studies of blinatumomab have been reported, including a smaller exploratory study demonstrating a 69% (CI, 52% to 84%) CR rate and a larger study demonstrating a 43% (CI, 36% to 50%) CR rate.
In general, there has been substantial experience with CAR therapeutics in children and adults with B-ALL, and response rates have not varied with age. In contrast, literature regarding blinatumomab in the pediatric population is sparse, with a 31% CR rate reported in 1 pediatric phase 2 trial, which appears lower than CR rates reported from CAR-T trials in similar patient cohorts.4,5 Whether this heralds a lower response rate to blinatumomab in children vs adults with B-ALL remains unclear. Another caveat to interpreting response rates across studies is difficulty in assessing pretreatment disease burden; at least 3 CAR-T trials included patients with MRD-only disease while the fraction of patients with MRD-only disease is not available from all reported blinatumomab trials. Notably, 2 studies of blinatumomab that exclusively enrolled patients with MRD-only disease reported impressive response rates.6,7 Thus, both CD19-CAR and blinatumomab appear to be promising therapeutics for patients with low-burden or MRD only disease, but larger numbers of patients are needed to more definitively define the response rate using CD19-CAR in this setting. In summary, definitive comparisons of response rates between CD19-CAR-T and blinatumomab are not available, but CAR-based therapies have, on average, demonstrated higher remission rates than those reported with blinatumomab.
Are CAR T cells feasible for my patient?
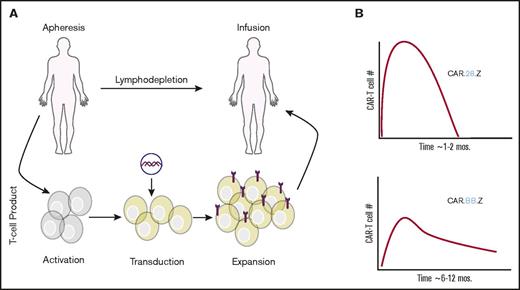
As illustrated in Figure 1A, CAR T-cell therapy is clearly more complex than administration of an off-the-shelf drug. Nonetheless, despite the fact that essentially all trials of CAR-T therapy for B-ALL have exclusively enrolled extensively pretreated relapsed or refractory patients, >90% success rates of product manufacturing have been reported by 2 groups3,8 suggesting that feasibility does not provide an absolute barrier to this therapy. In an ideal situation, autologous CAR-T products could be generated in as little as 10 days, and it is hoped that continued improvements to the manufacturing process will increase the likelihood that CAR T cells are available for every eligible patient. Development of allogenic, “off-the-shelf” CAR T cells is also being pursued, with a promising result in an infant with B-ALL, igniting the race to bring allogenic CAR T cells to market.9,10 Nonetheless, at the current time, CAR-T therapies are available only at a handful of academic centers, manufacturing capacity remains insufficient to meet demand, and CAR-T products are not currently approved by the US Food and Drug Administration; therefore, patients must be treated on a clinical trial. Thus, at the time of this writing, the limited availability of CAR T cells gives the edge to blinatumomab for feasibility and ease of administration.
Overview of administration and kinetics of CAR T cells. (A) Overview of CAR T-cell manufacturing and administration. (B) Impact of CAR T-cell costimulatory domain (CD28 or 4-1BB) on kinetics and duration of CAR T cells.
Overview of administration and kinetics of CAR T cells. (A) Overview of CAR T-cell manufacturing and administration. (B) Impact of CAR T-cell costimulatory domain (CD28 or 4-1BB) on kinetics and duration of CAR T cells.
How does toxicity of CAR T cells and blinatumomab compare?
Cytokine release syndrome (CRS) has been observed following both CAR T cells and blinatumomab, and the pathophysiology and approach to clinical management are similar.11,12 Although the incidence of sCRS appears lower following blinatumomab, sCRS is a marker of response and may occur less if response rates are lower (Table 1). Further, risk and severity of CRS is proportional to antigen burden, and if tumor burden is not comparable across studies, it is impossible to compare the propensity for one therapy vs another to induce severe CRS. Adverse neurologic events including seizures, encephalopathy, psychiatric disorders, and delirium have been reported with both agents at a comparable incidence (Table 1). Thus, both blinatumomab and CAR T cells may cause neurologic toxicity and CRS, and current data suggest that the incidence and severity of these toxicities are driven primarily by leukemic burden and potency of the antitumor effect rather than therapeutic modality per se.
Which therapy provides more durable antileukemia effects?
Increasing experience with CAR therapeutics has revealed insightful structure-function relationships that likely have substantial clinical impact. It is now clear that incorporation of costimulatory domains enhances CAR T-cell expansion; although T cells use a host of costimulatory receptors, most CAR-T constructs use either CD28 or 4-1BB (CD137) for coactivation signals.13-15 Both constructs enhance CAR T-cell expansion, but recent studies have illustrated significant distinctions in the biology of CD19.28.z-CAR vs CD19.BB.z-CAR.16,17 CD19.28.z-CAR-Ts show a faster and higher peak of in vivo proliferation but are prone to earlier exhaustion and disappearance, whereas CD19.BB.z-CAR T cells expand more slowly and reach a lower peak but demonstrate longer persistence (Figure 1B). Emerging reports have demonstrated persistent detectable CD19.BB.z-CAR T cells in a sizable fraction of patients >1 year following infusion. In contrast, blinatumomab has a short half-life (2.11 hours), requiring administration by continuous infusion over 28 days18 with no evidence for ongoing antileukemic immune responses following cessation of blinatumomab.7 Thus, a major distinction between blinatumomab and CD19.BB.z-CAR T cells is a difference in the duration of antileukemic effects.
The significance of the therapeutic durability of CAR-Ts is impacted by the clinical setting in which the therapy is rendered. For patients using CD19-based immunotherapy as a bridge to allogeneic SCT, transient but potent antileukemic effects of blinatumomab, CD19.28.z-CARs, or CD19.BB.z-CARs are likely equally effective. However, many patients undergoing CAR-T therapy have already relapsed following hematopoietic SCT or may not be candidates for hematopoietic SCT because of comorbidities, lack of a suitable donor, or other factors. For such patients, based on current understanding, treatment with a CD19.BB.z-CAR provides the best chance for persistent antileukemic effects and potentially cure.
What about extramedullary disease?
The central nervous system is a long-recognized reservoir wherein leukemia is able to elude systemic cytotoxic therapy. CAR T cells consistently demonstrate efficient penetration into the cerebrospinal fluid where they are capable of eradicating persistent leukemia.3,19,20 The testes are another potentially protected sanctuary for ALL cells. Presence of CAR T cells in the testes has not been discretely demonstrated, although patients with previous testicular disease have been reported to demonstrate testicular inflammation clinically following CAR-T treatment, suggesting their presence.3 To our knowledge, there are no data demonstrating blinatumomab is able to penetrate the central nervous system or testes for treatment of sanctuary sites of disease. As such, CAR T cells may prove more effective for treatment and surveillance of extramedullary disease sanctuaries in B-ALL patients.
Can I try blinatumomab first and then a CAR-T if there is no response?
It is not currently known if pretreatment with blinatumomab impacts subsequent response to CD19 CAR-T therapies, although CD19-CARs have induced remissions in patients after failure with blinatumomab.21 With every targeted therapy administered, the risk of antigen escape and subsequent relapse is likely to rise. Antigen escape associated with diminished expression of CD19 is being recognized with increasing frequency and represents a barrier to progress in immunotherapy for B-ALL.22-24 Thus, it is important to acknowledge that administration of blinatumomab prior to CD19-CAR therapy could increase the risk of CD19 loss immune escape and ultimately diminish cure rates.
Conclusion
CAR T cells are in clinical trials at institutions across the world25 and are likely to be increasingly available in the coming years. Given promising efficacy data in patients with relapsed or refractory B-ALL, these therapies appear poised to become a mainstay of therapy for B-cell malignancies going forward. Absent definitive data from randomized trials, we posit that CAR T cells have an edge over blinatumomab in their efficacy and potential for durable antileukemia effects, as well as their ability to address extramedullary disease. Yet, feasibility and availability of CAR therapies remain challenges for their wider implementation. Perhaps the greatest value of CD19-CAR therapy is its role in identifying the true power of adoptive T-cell therapy for cancer. It is likely that this platform will provide the basis for continued innovation and refinement of synthetic biology to improve the safety and efficacy of cell-based therapeutics for B-ALL and other malignant conditions.
Authorship
Contribution: K.L.D. and C.L.M. wrote the manuscript.
Conflict-of-interest disclosure: C.L.M. has patents/royalties from Juno Therapeutics. K.L.D. declares no competing financial interests.
Correspondence: Kara L. Davis, 1000 Welch Rd, Suite 300, Palo Alto, CA 94304; e-mail: kardavis@stanford.edu.
Acknowledgments
K.L.D. is supported by the NetApp St. Baldrick's Foundation Scholar award and is a CureSearch Young Investigator.