The protein Z–protein Z-dependent inhibitor complex is a factor Xa inhibitor. Protein Z deficiencies have recently been described in patients with ischemic stroke. As placenta infarction leads to poor pregnancy outcome, we studied protein Z plasma concentrations in nonthrombotic, nonthrombophilic consecutive patients with unexplained pregnancy wastage. A significant amount of protein Z deficiencies was only found in the early fetal loss group (< 1 mg/L; 44 of 200,P < 10−4) and mainly in the case of fetal demise between the beginning of the 10th and the end of the 15th week of gestation (odds ratio, 6.7 [3.1-14.8],P < 10−3). These deficiencies were not due to partial vitamin K1 deficiency, and at least some of them were constitutional ones. In women, protein Z deficiency may induce an enhanced risk of severe placental insufficiency soon after the connection of maternal and fetal circulations.
Introduction
Protein Z is a vitamin K–dependent plasma protein that serves as a cofactor for the control of the coagulation factor Xa by the protein Z–dependent protease inhibitor.1,2 Protein Z null mice have an apparently normal phenotype, but protein Z deficiency dramatically increases the thrombotic phenotype in mice carrying the factor VLeiden genotype.3 Studies to determine the role of protein Z in human thrombosis have, to date, led to the description of an association between prior ischemic stroke and protein Z deficiency.4
Ultrasonographic data indicate that the placenta replaces the yolk sac as the source of blood supply to the embryo from the beginning of the 8th to the end of the 9th week of gestation.5 From this crucial step, pregnancy outcome is dependent on sustained placental development; thrombosis in the maternal placenta may lead to fetal demise.
Here we describe the incidence of protein Z deficiency in women with unexplained pregnancy loss.
Study design
Patients
All the women we studied had given their informed consent for participation to our Abnormal Pregnancy Study Program, based on the recruitment of a vast cohort of patients from the South of France with at least one miscarriage/fetal loss, and of healthy parity- and age-matched control subjects (NOHA studies6-9). In this program, they were all investigated for classical prothrombotic factors as described (essential thrombocythemia; antiphospholipid/anticofactor antibodies; dysfibrinogenemia; deficiency in antithrombin, protein C, or protein S; factor V Leiden mutation; 20210A allele in the prothrombin gene; high plasminogen activator inhibitor 1 plasma levels; or hyperhomocysteinemia).
We studied 4 groups of consecutive women with negative thrombotic antecedents and prothrombotic factors: 200 patients with unexplained primary recurrent miscarriages before the 8th week of gestation (3 episodes; median age, 26.2 years), 200 patients with one unexplained primary episode of early fetal death from the 10th to the end of the 19th week (median age, 23.1 years), 50 patients with one unexplained primary episode of late fetal death from the beginning of the 20th week (median age, 22.8 years), and 200 healthy mothers of one child (median age, 23.0 years). Table 1 gives the characteristics of the initial population of consecutive women from which the final groups of patients and controls were obtained.
Characteristics of the initial population of consecutive women from which the studied final groups of childless patients and controls were obtained after exclusion of those with thrombotic antecedents and/or biologic prothrombotic factors
| . | N . | TA . | AT . | PC . | PS . | FVL . | FIIL . | aPLAb . | HCY . | PAI-1 . |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | ||||||||||
| N | 289 | 15 | 0 | 0 | 0 | 5 | 6 | 46 | 26 | 55 |
| % | 5.2 | 0 | 0 | 0 | 1.7 | 2.1 | 15.9 | 9 | 19 | |
| Group 2 | ||||||||||
| N | 312 | 27 | 0 | 1 | 12 | 20 | 13 | 51 | 23 | 27 |
| % | 8.7 | 0 | 0.3 | 3.9 | 6.4 | 4.2 | 16.4 | 7.4 | 8.7 | |
| Group 3 | ||||||||||
| N | 81 | 8 | 0 | 0 | 3 | 6 | 4 | 15 | 6 | 4 |
| % | 9.9 | 0 | 0 | 3.7 | 7.4 | 4.9 | 18.5 | 7.4 | 4.9 | |
| Control group | ||||||||||
| N | 217 | 1 | 0 | 0 | 0 | 4 | 5 | 2 | 2 | 3 |
| % | 0.4 | 0 | 0 | 0 | 1.8 | 2.3 | 0.9 | 0.9 | 1.4 |
| . | N . | TA . | AT . | PC . | PS . | FVL . | FIIL . | aPLAb . | HCY . | PAI-1 . |
|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | ||||||||||
| N | 289 | 15 | 0 | 0 | 0 | 5 | 6 | 46 | 26 | 55 |
| % | 5.2 | 0 | 0 | 0 | 1.7 | 2.1 | 15.9 | 9 | 19 | |
| Group 2 | ||||||||||
| N | 312 | 27 | 0 | 1 | 12 | 20 | 13 | 51 | 23 | 27 |
| % | 8.7 | 0 | 0.3 | 3.9 | 6.4 | 4.2 | 16.4 | 7.4 | 8.7 | |
| Group 3 | ||||||||||
| N | 81 | 8 | 0 | 0 | 3 | 6 | 4 | 15 | 6 | 4 |
| % | 9.9 | 0 | 0 | 3.7 | 7.4 | 4.9 | 18.5 | 7.4 | 4.9 | |
| Control group | ||||||||||
| N | 217 | 1 | 0 | 0 | 0 | 4 | 5 | 2 | 2 | 3 |
| % | 0.4 | 0 | 0 | 0 | 1.8 | 2.3 | 0.9 | 0.9 | 1.4 |
Group 1, patients with 3 unexplained primary miscarriages before the 8th week of gestation; group 2, patients with one unexplained primary episode of early fetal death from the 10th to the end of the 19th week of gestation; group 3, patients with one unexplained primary episode of late fetal death from the beginning of the 20th week of gestation; control group, healthy mothers of one child. TA, thrombotic antecedents; AT, antithrombin deficiency; PC, protein C deficiency; PS, protein S deficiency; FVL, factor V Leiden mutation; FIIL, allele 20210A in the prothrombin gene; aPLAb, antiphospholipid/antiprotein antibodies; HCY, mild hyperhomocysteinemia; PAI-1, high plasminogen activator inhibitor 1 plasma levels; all these biologic data are according to previously published methods and results.6-9
Methods
Blood samples were collected, processed, and stored at −80°C, according to standard procedures, at least 6 months after the last obstetrical accident, in nontreated patients. Protein Z plasma concentrations were thereafter measured by using a commercially available enzyme-linked immunosorbent assay (Asserachrom Protein Z; Diagnostica Stago and Serbio, Asnières, France).
Statistical analysis
Results are described by using the StatView 5 software (Abacus Concepts, Berkeley, CA) and nonparametric statistics: median, lower-upper quartile values, and range are given. Quantitative results were compared by using the Mann-Whitney rank sum test. Association between categorical variables was tested after cross tabulation by the Pearson chi square and by Fisher exact tests. Crude odds ratios and 95% confidence intervals were calculated by using logistic regression analysis. The level of significance was 0.05.
Results and discussion
The median protein Z plasma concentration obtained in the 200 control women was 2.08 mg/L, and lower-upper quartiles were 1.71 mg/L to 2.55mg/L with a range of 0.68 mg/L to 3.25 mg/L. These values are close to published references.10
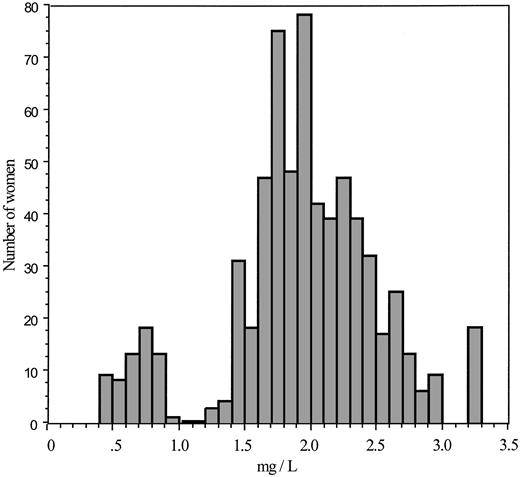
Figure 1 shows the distribution of protein Z plasma concentrations obtained in the 650 patients and control subjects. It clearly shows a bimodal pattern, with a subgroup of 62 women with concentrations lower than 1 mg/L who we assumed to be carriers of a partial deficiency. This protein Z deficiency-related threshold value was close to the value of the 5th percentile calculated in the control group, in the group of patients with recurrent miscarriages, and in patients with late fetal loss (1.05 mg/L). The distribution of these protein Z deficiencies was 8 cases (4%) in control women, 8 (4%) in women with recurrent miscarriages, 2 (4%) in women with late fetal, and 44 cases (22%,P < 10−4) in women who had experienced one early fetal death, with a mean odds ratio, the control group being the reference, reaching 6.7 (95% confidence interval, 3.1-14.8;P < 10−4).
Distribution of the protein Z plasma concentrations in the whole group of 650 women.
Distribution of the protein Z plasma concentrations in the whole group of 650 women.
The aborted products of conception had not been systematically examined pathologically. We only have partial, preliminary data showing, in the written conclusions of the examinations performed in 18 of the 44 early fetal death associated with a partial protein Z deficiency, “a significant growth retardation associated with signs of placental insufficiency, with the presence of thrombotic lesions.”
We thereafter studied, in patients with early fetal loss, the correspondence between the evolution of pregnancy and the protein Z deficiency status: 40 deficiencies were associated with a loss before the end of the 15th week of gestation (115 cases) but only 4 between the beginning of the 16th and the end of the 19th week of gestation (85 cases) (P < 10−4), corresponding, in deficient patients, to an odds ratio for an accident before the end of the 15th week of 10.8 (3.7-31.0; P < 10−4). In the patients described in Table 1 with protein S deficiency, factor V or factor II Leiden mutation, positive antiphospholipid/antiprotein antibodies, or mild hyperhomocysteinemia, early fetal losses had occurred after the end of the 15th week, and late fetal losses could also be observed.
All patients with a deficiency had normal plasma concentrations of the other vitamin-K–dependent coagulation factors, particularly those with a short plasma half-life (protein C and factor VII). Twenty-nine of them agreed to receive a single 10-mg vitamin K1 injection. No significant changes in plasma protein Z concentrations were observed (days 2, 5, and after vitamin supplementation; reported protein Z plasma half-life, 2.5 days) with the final persistence of the deficiencies. We were able to investigate both parents of 8 of these patients; evidence was found of a hereditary protein Z deficiency in 6 of them, one of their parents being also deficient.
In conclusion, our data indicate a high frequency of protein Z deficiency in women with a first primary episode of early fetal death from the 10th to the end of the 15th week of gestation that is not due to an underlying vitamin K1 deficiency and is at least sometimes an inherited one. The observed frequencies of the deficiencies are similar, in our controls and positive patients, to the one previously described in patients with ischemic stroke2 (positive group of patients about 20%; negative groups of patients and controls about 5%). The physiopathology of this association is unclear. It is different from classical thrombophilias, which expose to thrombosis of a normal placental intervillous space. Protein Z deficiency is not to date a risk factor for venous thrombosis, and the onset of associated obstetrical accidents is quite different to the one observed in classical thrombophilias. During the 6 weeks after the connection of the fetal circulation to the uterine one, a primary defective cytotrophoblast invasion of the spiral uterine arteries may occur, the uteroplacental circulation remaining in a state of high resistance, as described during the first phase of the 2-stage model of preeclampsia. In such an arterial-like regimen of blood flux, protein Z deficiency, which is to date involved in thrombotic complications of atherosclerosis, may favor local thrombogenesis.
We thank the numerous current and past obstetricians and gynecologist colleagues who agreed to participate in our Mediterranean Abnormal Pregnancy Study Program and, of course, all patients and controls who agreed to join us in this long-distance running adventure. We thank Margaret Manson for editorial assistance.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Jean-Christophe Gris, Laboratoire d'Hématologie, Centre Hospitalier Universitaire, 5, rue Hoche, F-30 029 Nı̂mes cedex 9, France; e-mail: jcgris@chu-nimes.fr.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal