No definitive biologic function has been associated with the human ABO histo-blood group polymorphism, or any other terminal carbohydrate differences within or between closely related species. We have experimentally addressed the question of whether viral particles can become glycosylated as determined by the glycosylation (eg, ABO) status of the producer cell and as a result be affected by human serum containing specific natural antibodies (NAbs). Measles virus was produced in cells transfected with cDNA encoding, either human A-transferase, B-transferase, an inactive “O-transferase,” or a pig α1-3galactosyltransferase (α1-3GT) synthesizing the Galα1-3Gal structure. The viruses were shown to carry the same ABO structures as the cells; that is, A but not B if produced in A-type cells, and B but not A if produced in B-type cells. Only O was detected on the virus produced from O-type cells, whereas reduced amounts of O appeared on the A- and B-type viral particles. In addition, the Galα1-3Gal structure was transferred onto measles only when grown in human cells expressing this structure. When subjected to human preimmune sera, the A-type, the B-type, and the Galα1-3Gal viral particles were partially neutralized in a complement-dependent manner. However, the O-type or the Galα1-3Gal–negative viral particles were not neutralized. The neutralization appeared to be mediated by specific NAb, as judged by specific inhibition using synthetic A and Galα1-3Gal oligosaccharides. Such viral glycosylation may thus partly explain why the ABO antigens and other similar intraspecies as well as interspecies polymorphic carbohydrates have evolved and been maintained over long evolutionary periods.
Introduction
The ABO (or ABH) histo-blood group system is characterized by the expression of polymorphic carbohydrate termini on several cell types. The genetic basis for this polymorphism in humans is explained by the existence of allelic forms of a single gene encoding glycosyltransferases with specificity for different monosaccharides.1 They appear to be evolutionarily old, being present on glycosylated structures in different eukaryotic as well as prokaryotic organisms, and established their present day polymorphic form in humans at the latest during early primate evolution (for a review, see Blancher et al2). Hence, it would be surprising if the ABO structures did not serve an important purpose. No definitive biologic function has, however, as yet been identified,3 although suggestions have often centered on immunologic explanations.4-7 Another very similar terminal carbohydrate structure, the Galα1-3Galβ1-4GlcNAc-R (referred to as Galα1-3Gal) is present in other mammals but not in humans and other Old World primates.8
Bacteria mimicking vertebrate terminal carbohydrates may have given rise to selection pressures favoring polymorphic glycans.9In addition, many pathogens and their toxins bind to specific terminal carbohydrate structures and may consequently produce selection pressures affecting the evolution of terminal carbohydrate structures.7,10 It has also been previously suggested that viruses may carry ABO structures as part of their envelope11,12 and consequently serve as potential selective forces influencing ABO genotype frequencies in a population.7 Moreover, studies of influenza outbreaks,13,14 as well as a laboratory study of HIV virus from patients,15 have indicated that such suggestions may be relevant in an epidemiological context.
NAbs, that is, spontaneously forming antibodies, may form an early defense mechanism against bacteria as well as virus by binding to and either neutralizing or opsonizing the pathogen, followed by complement- or Fc-receptor–mediated phagocytosis.16,17NAbs may in this way form an important barrier against early viral dissemination to vital organs, as well as provide the adaptive immune response a “head start” in its production of specific antiviral responses.18 As to the specific targets of such NAbs on viruses, very little is known. Although it may, from an immunologic perspective, be more accurate not to call Abs against A/B- or Galα1-3Gal antigens naturally occurring, due to their probable initial production as a result of target antigen encounter in the gut,19,20 we will nevertheless use the definition NAb throughout this paper for simplicity and historical reasons. Takeuchi et al21 and Rother et al22 showed that the well-known neutralizing capacity by human serum of C-type retroviruses produced from, for example, murine cells but not from human cells is due to the binding of NAb and complement. It was shown that these NAbs are specific for the Galα1-3Gal carbohydrate terminus, expressed in all mammals except humans and Old World primates. Subsequently, other enveloped viruses have been shown to be equally sensitive to NAbs against this terminal carbohydrate structure,23 and we hypothesized that such binding may have protected humans from cross-species viral transmissions.21 NAbs against the A and/or the B antigens are, in analogy to the NAbs against Galα1,3Gal, ubiquitously produced in individuals lacking the particular A/B structure. We wished to examine experimentally whether NAbs and virus interactions can be specified by ABO as well as Galα1-3Gal antigens. If that is the case, it would indicate that the ABO histo-blood group polymorphism may have developed and been maintained partly as a means to control or influence immune responses to viral infections. We chose to use measles virus, which together with other paramyxoviruses of the genusMorbilli have constituted a significant immunologic challenge to humans as well as other species throughout evolution and may therefore have taken part in shaping any selective forces brought about by antigenic carbohydrate expression on viral envelopes.
Materials and methods
Virus production
HeLa cells (genotype OO) were transfected with cDNA expression constructs encoding human A- and B-transferase,24 as well as a negative “O-transferase” control construct consisting of a major part of the A-transferase cDNA containing a critical glycine to arginine substitution at codon 268, which is found in some O-alleles, for example, the O2′ allele. This O-transferase construct has previously been shown to nullify the A-transferase activity.25 These cells are hereafter referred to as A, B, or H cells. Transfected cultures were positively sorted and/or cloned for expression of respective transferase to enable maintenance of cell cultures and analyzed using anti-A (81FR2.2), -B (3E7), or -H (92FR-A2) monoclonal antibodies (mAbs), and fluorescein isothiocyanate (FITC)–conjugated goat F(ab′)2 anti–mouse Ig Ab (Dako, Carpinteria, CA) and flow cytometry (Figure1). Similarly, human HT1080 cells have been previously transfected with a pig α1,3galactosyltransferase (α1-3GT) cDNA26 and the resulting Galα1-3Gal–expressing cells, HG13, analyzed using a specific lectin and flow cytometry.21 Loss strain measles27were kindly provided by Dr D. Brown at the Public Health Laboratory Services (PHLS), Colindale, United Kingdom. This measles strain was passaged through human HeLa or HT1080 cells and subsequently used to infect the A, B, H, HT1080, and HG13 cells from which supernatants were harvested upon maximal cytopathic effect. Cell debris were cleared from the viral supernatants by centrifugation following freezing overnight at −80°C, titered on monkey Vero cells as plaque forming units (PFU) per mL (essentially as previously described),28 and aliquots frozen at −80°C. These virus preparations are hereafter referred to as A, B, H, Gal(−), and Gal(+) viruses. An identical procedure was used to produce and collect supernatants from the same, but uninfected, cells.
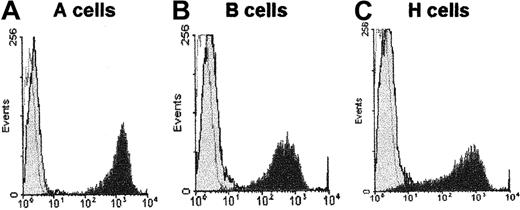
Expression of ABO antigens on HeLa cells.
HeLa cells were transfected with either human A-transferase (A), B-transferase (B), or a “control” O-transferase (C), as previously described,24 and analyzed by specific mAb (as indicated in “Materials and methods”) and flow cytometry. Dark gray indicates cell populations stained with specific Ab and FITC-labeled secondary Ab; light gray indicates cell populations stained with a secondary reagent only; white indicates cells without any staining.
Expression of ABO antigens on HeLa cells.
HeLa cells were transfected with either human A-transferase (A), B-transferase (B), or a “control” O-transferase (C), as previously described,24 and analyzed by specific mAb (as indicated in “Materials and methods”) and flow cytometry. Dark gray indicates cell populations stained with specific Ab and FITC-labeled secondary Ab; light gray indicates cell populations stained with a secondary reagent only; white indicates cells without any staining.
Capture enzyme-linked immunosorbent assay for measles virus
Nunc Maxisorp 96-well plates were coated overnight at 4°C with 1μg of a monoclonal antimeasles hemagglutinin Ab (clone ZD6; Biodesign International, Kennebunk, ME). The wells were washed using 0.1% Tween 20 in phosphate-buffered saline (PBS) and blocked with a PBS solution containing 0.1% Tween 20 and 1% Tween + BSA + PBS (DB) for 1 hour at 25°C, and washed again. Virus supernatants (A, B, H, Gal+, Gal−), diluted with respective uninfected cell supernatants, were added at an identical 5 × 105 PFU/mL and incubated at 37°C for 30 minutes. As controls, virus-free supernatants from the different uninfected cells were always included. New washes were followed by the addition of detection reagents: either, in (Figure 2A), a horseradish peroxidase (HRP)–labeled A-specific lectin from Helix pomatia (Sigma, Poole, Dorset, United Kingdom); in (Figure 2B), the A-specific mouse IgG3 mAb BG-2 (Signet Laboratories, Dedham, MA); in (Figure 2C), the B-specific mouse IgM mAb 3E7 (Dako); in (Figure 2D), an HRP-labeled H-specific lectin from Ulex europaeus (Sigma); or in (Figure 2E), an HRP-labeled Galα1-3Gal–specific lectin from Bandeiraea simplicifolia (Sigma), all at 3 different dilutions in DB and incubated at 37°C for 1 hour. After subsequent wash, the mAb–enzyme-linked immunosorbent assay (ELISA) plates were incubated at 37°C for 1 hour with either an HRP-labeled rat IgG1 kappa mAb against mouse IgG3 heavy chain (Research Diagnostics, Flanders, NJ), or an HRP-labeled rabbit anti–mouse IgM polyclonal Ab (Zymed, San Francisco, CA). The plates were subsequently incubated with either freshly made O-pheny-lenediamine (OPD) peroxidase substrate (Fast; Sigma) or 2,2′-Azino-bis(3-ethylbenzothiozoline-6-sulfonic acid) (ABTS) single solution (Zymed) for 30 minutes and absorbance analyzed at 450 nm or 410 nm, respectively, on a Dynatech MRX plate reader.
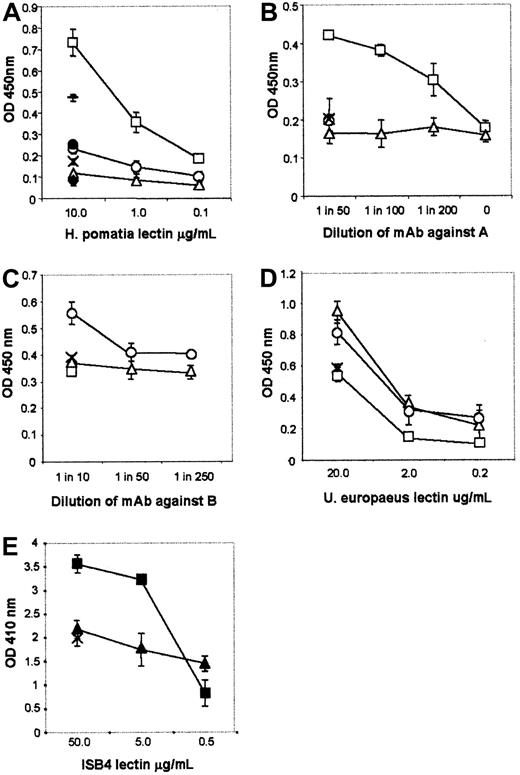
Capture ELISA showing expression of A, B, H, and Galα1-3Gal antigens on measles.
Microwell plates were coated with a monoclonal antimeasles hemagglutinin Ab. Virus-containing supernatants from cells transfected with either A, B, inactive “O-transferase,” or α1-3GT cDNA clones were diluted with respective supernatant from uninfected cells and added at an identical 5 × 105 PFU/mL. Subsequently, the following detection reagents were added: (A) HRP-labeled A-specific lectin from H pomatia; (B) A-specific mAb BG-2 and an HRP-labeled secondary Ab; (C) B-specific mAb 3E7 and an HRP-labeled secondary Ab; (D) H- or O-specific lectin from U europaeus; (E) an HRP-labeled Galα1-3Gal–specific lectin from B simplicifolia. Plates were subsequently incubated with peroxidase substrate and the absorbance analyzed on a plate reader. Open squares indicate A virus; open circles, B virus; open triangles, H virus; solid squares, Gal(+) virus; solid triangles, Gal(−) virus; and crosses, virus-free supernatant from the respective uninfected cells used to produce virus. In addition, in (A), a filled diamond indicates A virus not incubated with lectin; a filled circle, wells without capture Ab; and a horizontal line, virus which had been preincubated with 10 μg/mL capture Ab. The plotted results indicate the mean (SEM) of duplicate samples.
Capture ELISA showing expression of A, B, H, and Galα1-3Gal antigens on measles.
Microwell plates were coated with a monoclonal antimeasles hemagglutinin Ab. Virus-containing supernatants from cells transfected with either A, B, inactive “O-transferase,” or α1-3GT cDNA clones were diluted with respective supernatant from uninfected cells and added at an identical 5 × 105 PFU/mL. Subsequently, the following detection reagents were added: (A) HRP-labeled A-specific lectin from H pomatia; (B) A-specific mAb BG-2 and an HRP-labeled secondary Ab; (C) B-specific mAb 3E7 and an HRP-labeled secondary Ab; (D) H- or O-specific lectin from U europaeus; (E) an HRP-labeled Galα1-3Gal–specific lectin from B simplicifolia. Plates were subsequently incubated with peroxidase substrate and the absorbance analyzed on a plate reader. Open squares indicate A virus; open circles, B virus; open triangles, H virus; solid squares, Gal(+) virus; solid triangles, Gal(−) virus; and crosses, virus-free supernatant from the respective uninfected cells used to produce virus. In addition, in (A), a filled diamond indicates A virus not incubated with lectin; a filled circle, wells without capture Ab; and a horizontal line, virus which had been preincubated with 10 μg/mL capture Ab. The plotted results indicate the mean (SEM) of duplicate samples.
Virus neutralization
Two human measles Ab-negative sera, both of which were blood group O (kindly provided by Dr D. Brown, PHLS, Colindale, United Kingdom), were diluted 1:5 in PBS, of which some aliquots were incubated for 15 minutes at 4°C with synthetic A- or Galα1,3Galβ1,4GlcNAc tri-saccharides (Dextra, Oxford, United Kingdom) in PBS. In addition, aliquots of the serum dilutions were decomplemented at 56°C for 20 minutes. Where relevant, virus supernatants were diluted in PBS to 103 PFU/mL, 90 μL added to 90 μL of the relevant serum sample and incubated for 1.5 hours at 37°C and 5% CO2. Subsequently, virus/serum mixtures were plated on 24-well plates in pentuplicates or triplicates for each experimental group essentially as previously described.28 A quantity of 4 × 105 freshly harvested Vero cells in Dulbecco modified Eagle medium (DMEM) with 2% fetal calf serum (FCS) was added to each well and incubated for 3 hours at 37°C and 5% CO2. The media was subsequently replaced with overlay media (DMEM, 2% FCS, 0.15% sodium bicarbonate, and 0.85% carboxymethyl cellulose) and incubated for 7 days at 37°C and 5% CO2. Overlays were discarded, washed in PBS, fixed for 1 minute in 5% formalin in PBS, incubated for 30 minutes at room temperature with 1 mL crystal violet solution (30 mg crystal violet in 5% formalin and 5% EtOH in PBS). The stain was removed, plates rinsed in water, and plaques that appeared as clear circles on a purple background were counted. Viral titers were expressed as percentages of the mean of wells containing virus incubated without serum (100%); in the experiments described in Figure 3 and in Figure 5, 5 wells; and in the experiment described in Figure 4, 3 wells.
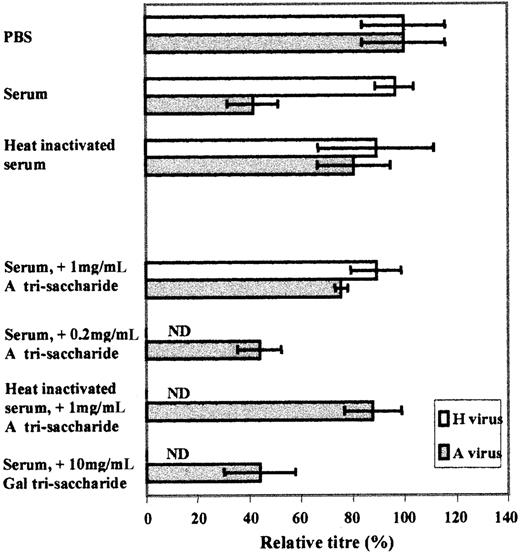
Plaque-reduction neutralization assay showing the effect of A-virus incubation with anti-A/B–containing human serum.
A and H virus supernatants, diluted to 103 PFU/mL, were incubated with a human O-type reference serum, lacking measles-specific Ab and previously diluted 1:5 in PBS. Similarly, diluted A and H virus supernatants were incubated with the same serum, previously either decomplemented by heat-inactivation, or incubated with A or Galα1-3Galβ1-4GlcNAc trisaccharides. Subsequently, virus/serum mixtures were analyzed for viral titers by a plaque-reduction neutralization assay on Vero cells. Results (mean SEM) in pentuplicates are shown as the mean percentages as compared with the untreated (PBS) A- and H-virus titers (100%). ND denotes experimental conditions involving H virus that were not determined.
Plaque-reduction neutralization assay showing the effect of A-virus incubation with anti-A/B–containing human serum.
A and H virus supernatants, diluted to 103 PFU/mL, were incubated with a human O-type reference serum, lacking measles-specific Ab and previously diluted 1:5 in PBS. Similarly, diluted A and H virus supernatants were incubated with the same serum, previously either decomplemented by heat-inactivation, or incubated with A or Galα1-3Galβ1-4GlcNAc trisaccharides. Subsequently, virus/serum mixtures were analyzed for viral titers by a plaque-reduction neutralization assay on Vero cells. Results (mean SEM) in pentuplicates are shown as the mean percentages as compared with the untreated (PBS) A- and H-virus titers (100%). ND denotes experimental conditions involving H virus that were not determined.
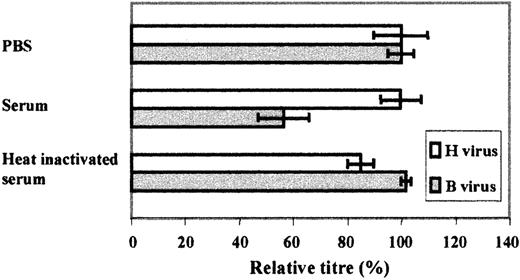
Plaque-reduction neutralization assay showing the effect of B-virus incubation with anti-A/B–containing human serum.
B and H virus supernatants, diluted to 103 PFU/mL, were incubated with a human O-type reference serum, lacking measles-specific Ab and previously diluted 1:5 in PBS. Similarly, diluted B and H virus supernatants were incubated with the same serum, previously decomplemented by heat-inactivation. Subsequently, virus/serum mixtures were analyzed for viral titers by a plaque-reduction neutralization assay on Vero cells. Results (mean SEM) in triplicates are shown as the mean percentages as compared to the untreated (PBS) B- and H-virus titers (100%).
Plaque-reduction neutralization assay showing the effect of B-virus incubation with anti-A/B–containing human serum.
B and H virus supernatants, diluted to 103 PFU/mL, were incubated with a human O-type reference serum, lacking measles-specific Ab and previously diluted 1:5 in PBS. Similarly, diluted B and H virus supernatants were incubated with the same serum, previously decomplemented by heat-inactivation. Subsequently, virus/serum mixtures were analyzed for viral titers by a plaque-reduction neutralization assay on Vero cells. Results (mean SEM) in triplicates are shown as the mean percentages as compared to the untreated (PBS) B- and H-virus titers (100%).
Results
Expression of specific ABO antigens on virus producer cells
The transfection of specific terminal glycosyltransferase (GT) genes into cell lines allows for the modulation of terminal glycosylation in the cells. As shown in Figure 1, transfection of a human A-transferase cDNA, or B-transferase cDNA on a background of O (or H) in human HeLa cells leads to the expression of A or B antigens, respectively. HeLa cells transfected with a nonfunctional O-transferase construct25 ensured that the transfection process itself did not influence the subsequent experimental conditions. The corresponding staining of A antigens on B cells and H cells, and B antigens on A cells and H cells resulted in background levels only, whereas staining of O on A and B cells appeared reduced to less than 30% of the H-cell staining (data not shown). Similarly, a pig α1-3GT cDNA26 was previously transfected into human HT1080 cells.21 Although the genotype of the HT1080 cells was not known, phenotypically they have consistently appeared as O of ABO (data not shown).
Transfer of ABO and Galα1-3Gal antigens from producer cells to virus
Identical PFU of measles virus produced in the transfectants were studied in capture ELISA assays, employing either an A-specific lectin from H pomatia, or a mAb, to detect the A antigen; a mAb to detect the B antigen; and specific lectins from U europaeusand B simplicifolia, to detect H and Galα1-3Gal antigens, respectively. As shown in Figure 2, the assays revealed that only measles produced from the A cells showed reactivity with either of the 2 A-specific reagents (Figure 2A-B). Similarly, although the detection level appeared lower, only virus produced in B cells bound significant levels of mAb against B antigen (Figure 2C). As expected, H-antigen reactivity was detected in all 3 virus types, that is, A, B, and H viruses, with the highest level on measles produced in H cells. Also, the B virus had relatively high levels of H antigen, perhaps in keeping with the lower levels of B antigens on B virus as compared with A antigen on A virus. Levels of Galα1-3Gal antigens were detected at significant levels only on virus produced in the cells transfected with α1-3GT (Figure 2E). Supernatants from the different uninfected transfectants did not show any increased lectin or Ab binding, ensuring that the capture of measles virus did not involve any significant amounts of nonviral material carrying ABO or Galα1-3Gal antigens. In addition, in the A-lectin ELISA, a preincubation step of the virus with unbound capture Ab significantly reduced the binding of A virus to the plate.
Neutralization of virus mediated by serum containing specific natural antibody and complement
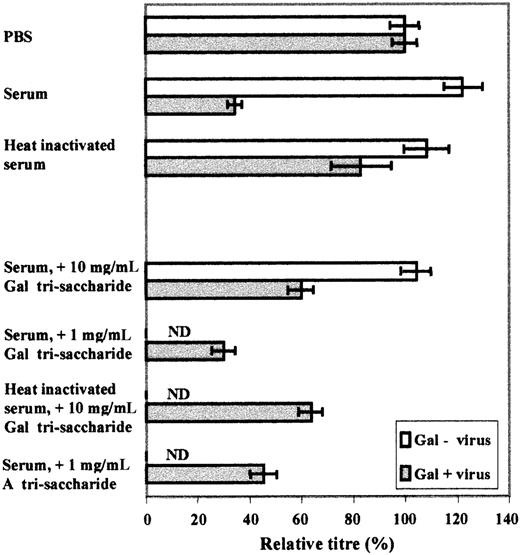
Equal amounts of the otherwise identical A and H viral stocks were incubated with a 1:5 dilution of a confirmed antimeasles negative serum (O-type), and the resulting serum-mediated neutralization assessed in a plaque-forming assay in pentuplicates (Figure3). Similarly, another O-type antimeasles negative serum was used at identical dilution for incubations with equal amounts of B and H viruses and a subsequent plaque-forming assay in triplicates (Figure 4). Virus produced in Galα1-3Gal–positive cells (Gal[+]) and equal amounts of Gal(−) virus were incubated with the same serum as in the first experiment, comparing A and H virus, and also subjected to the plaque-forming assay (Figure 5). In all 3 experiments, serum was either decomplemented by heat-inactivation or not before the incubations. In addition, in the first experiment comparing A and H virus (Figure 3), and in the third experiment comparing Gal(+) and Gal(−) virus (Figure 5), aliquots of the serum were preincubated with different amounts of synthetic trisaccharides, to assess the specificity of the anticarbohydrate activity. All results in the plaque-forming assays were compared with the respective virus incubated in PBS only (100%) and expressed as percentage neutralization thereof. The results in Figure 3 show that A virus is partially neutralized in the presence of serum in a complement-dependent manner, whereas H viruses are unable to serve as targets for neutralizing components in the serum. In addition, preincubation with 1 mg/mL of an A oligosaccharide significantly reduced the degree of neutralization, whereas preincubation with the irrelevant Galα1-3Gal oligosaccharide did not result in significant inhibition of the neutralization. These experiments were repeated several times with similar results. Likewise, B virus is partially neutralized in the presence of an anti-A/B–containing serum, whereas H virus is not (Figure 4). Again, this neutralization appears dependent on complement as indicated by heat-inactivation. In Figure 5, the results show that serum components are able, in a complement-dependent manner, to neutralize Gal(+) virus but not Gal(−) virus. In analogy with the A-virus results, preincubation of the virus with 10 mg/mL Galα1-3Gal oligosaccharide resulted in inhibited neutralization, whereas incubation with irrelevant A oligosaccharides did not. These experiments were also repeated several times with similar results.
Plaque-reduction neutralization assay showing the effect of Gal(+)-virus incubation with anti-Galα1-3Gal–containing human serum.
Gal(+) and Gal(−) virus supernatants, diluted to 103PFU/mL, were incubated with a human O-type reference serum, lacking measles-specific Ab and previously diluted 1:5 in PBS. Similarly, diluted Gal(+) and Gal(−) virus supernatants were incubated with the same serum, previously either decomplemented by heat-inactivation, or incubated with Galα1-3Galβ1-4GlcNAc or A trisaccharides. Subsequently, virus/serum mixtures were analyzed for viral titers by a plaque-reduction neutralization assay on Vero cells. Results (mean SEM) in pentuplicates are shown as the mean percentages as compared to the untreated (PBS) Gal(+) and Gal(−) virus titers (100%). ND denotes experimental conditions involving H virus that were not determined.
Plaque-reduction neutralization assay showing the effect of Gal(+)-virus incubation with anti-Galα1-3Gal–containing human serum.
Gal(+) and Gal(−) virus supernatants, diluted to 103PFU/mL, were incubated with a human O-type reference serum, lacking measles-specific Ab and previously diluted 1:5 in PBS. Similarly, diluted Gal(+) and Gal(−) virus supernatants were incubated with the same serum, previously either decomplemented by heat-inactivation, or incubated with Galα1-3Galβ1-4GlcNAc or A trisaccharides. Subsequently, virus/serum mixtures were analyzed for viral titers by a plaque-reduction neutralization assay on Vero cells. Results (mean SEM) in pentuplicates are shown as the mean percentages as compared to the untreated (PBS) Gal(+) and Gal(−) virus titers (100%). ND denotes experimental conditions involving H virus that were not determined.
Discussion
We have analyzed, in a controlled fashion by using cells transfected with specific glycosyltransferases, whether the terminal glycosylation of a cell determines the terminal glycosylation pattern on measles virus produced from these cells. The results show that the ABO status of the cells results in the appearance of the same ABO antigens on the virus. Moreover, the species-specific Galα1-3Gal antigen was also transferred from cell to measles, as previously shown for other viruses.21-23 Clearly, as can be seen in Figure2D, not all potential A- or B-antigen sites in glycoproteins or glycolipids on the virus are occupied by the respective monosaccharide making up these terminal specificities. Instead, it would appear that many of these sites, also on A and B viruses, remain as H antigens, the precursor substrate for A- and B-transferase. The level of H antigen also appeared to vary according to the amounts of A versus B antigen on the respective virus preparation.
Subsequently, the virus carrying specific terminal ABO or Galα1-3Gal glycosylation was used in experiments designed to test whether anti-ABO or anti-Galα1-3Gal serum components could neutralize the measles virus. The experiments clearly showed that this did happen and that such neutralization was strictly complement-dependent. Although showing the specificity of neutralization by inhibition with synthetic oligosaccharides, we have not formally shown that the components in serum responsible for the specificity against respective terminal glycosylation (ie, A, B, or Galα1-3Gal) are Abs, but we feel that it is reasonable to assume that they are. First, no alternative iso-haemagglutinins with ABO or Galα1-3Gal specificity are known in human serum, and second, previous results have clearly shown that human serum activity against Galα1-3Gal on virus is carried by antibodies and complement.21 22 A difficulty that we encountered in this context is the lack of a suitable antibody-free source of complement, which could be combined with purified anti–carbohydrate Ab as a replacement for the very limited availability of suitable antimeasles Ab-free sera of different ABO type.
Historically, suggested associations of particular ABO phenotypes have ranged from flat feet to severity of “hangovers” (reviewed by Prokop and Uhlenbruck29), including more recently even personality traits,30 intelligent quotient (IQ),31 and socioeconomic group belonging.32However, most recent suggestions for a function of the ABO histo-blood group polymorphism relate to immunologic subjects, such as tumor immunology and infectious agents (reviewed in Garratty33). Interactions between pathogens and host cell membranes may reflect antigenic similarity, receptor adhesion, or modulation of immune responses.34 The geographical distribution of ABO types appears to have been greatly influenced by natural selection.6,7 The fact that the O histo-blood group is universally much more common than the AB histo-blood group may indicate that the presence of anti-A/B Ab is an important selective force, rather than the presence of a particular antigen. Bacteria could be an important target for such an Ab (eg, see Muschel35). Indeed, the presence of carbohydrate substances on bacteria36,37 or other antigenic carriers entering the gut is after all the main suspected reason for the initial development in neonates of ABO Ab, as well as Ab against Galα1-3Gal.19,20 In addition, severe viral diseases have been implicated in this regard (eg, small pox).38 However, here it is important to consider that the glycosylation of a virus must be determined by the previous host cell, since a virus is unable to itself provide the complicated enzymatic machinery needed for glycosylation. This should therefore be born in mind when viral explanations for the patterns of ABO gene frequencies in human populations are considered. Another important factor with regard to a virus-associated function of ABO histo-blood groups concerns their tissue distribution. In contrast to erythrocytes, one tissue that appears to have a largely conserved expression of ABO and Galα1-3Gal antigens in a number of species examined is epithelial structures, in particular exocrine epithelia.39 40 This is interesting and intriguing since such tissues are involved in the spread of many viruses from one individual to another.
It has previously been suggested that Galα1-3Gal antigens acquired from a previous host may have protected humans from certain viral transmissions from other species.21,22 Here we show that the paramyxovirus measles also can carry Galα1-3Gal antigens serving as targets for neutralizing Abs. NAb-mediated protection between species may be particularly relevant for paramyxoviruses since several of these have clearly jumped species barriers, for example, dolphin (DMV) and porpoise morbilli virus (PMV), as well as canine (CDV) and phocine distemper virus (PDV),41 causing devastating epidemics in the new species, for example, PDV in harbor seals,42 CDV in Serengeti lions,43 and DMV in monk seals.44 An emerging viral threat to humans, and with particular relevance to the Galα1-3Gal antigen since it is transmitted from pigs, is the Nipah virus,45 also a member of the paramyxoviruses.
It was recently speculated that carbohydrates differing among individuals in one species (eg, ABO) may also have developed due to their capacity to be transferred onto viruses.7 Previous data from HIV virus produced from A-type lymphocytes appear to support these contentions.15 The data we present here show for the first time, under controlled circumstances with transfected cells, that the presence on virus of ABO antigens determined by the previous host (ie, producer cells) leads to a significant degree of neutralization in the presence of specific NAbs and complement. In addition to the neutralizing effect, it is likely that terminal carbohydrates of the Galα1,3Gal-type46 or the ABO-type aid the rapid uptake and presentation of viral antigens to the immune system, possibly explaining previous data from influenza outbreaks.13 14Although it is clearly not the case that histo-blood group status determines an all-important sensitivity to viral infections, we suggest that the transfer of ABO antigens on viral particles could lead to a situation in which balancing or frequency-dependent selection favors the polymorphic forms of these NAb targets. However, this is likely to have occurred in combination with other selection pressures determined by the presence of ABO-like antigens or their ligands also on bacteria and other pathogens.
We thank Dr David Brown and Dr Bernard Cohen for generous gifts of reagents as well as help with methods. We are also grateful to Prof Christine Kinnon and Dr Yasuhiro Takeuchi for critical review of the manuscript.
Supported by a project grant from the Wellcome Trust, United Kingdom.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Kenth Gustafsson, Molecular Immunology Unit, Institute of Child Health, University College London, 30 Guilford St, London WC1N 1EH, United Kingdom; e-mail: k.gustafsson@ich.ucl.ac.uk.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal