Spleen size was assessed in 73 patients with thrombocytosis and in 15 healthy subjects, comparing palpation with ultrasonography (US) measurement of longitudinal diameter and volume. Intraobserver and interobserver variability for volume on US, checked in 12 patients, was very low. Correlation between spleen volume measured by US and that measured by computed tomography was excellent. Splenomegaly was detected by palpation in 25% of patients, by US assessment of longitudinal diameter in 33%, and by US assessment of volume in 52%. After diagnostic work-up, 54 patients had a diagnosis of essential thrombocythemia (ET), 4 of idiopathic myelofibrosis (IMF), and 15 of secondary thrombocytosis (ST). Spleen volume in patients with ST was in the normal range (138 ± 47 mL) and was significantly lower than that in patients with ET or IMF (370 ± 210 mL;P < .001). Thus, US-measured volume was the most sensitive method for identifying nonpalpable splenomegaly in patients with primary myeloproliferative diseases, and it may help in distinguishing these diseases from reactive disorders.
Introduction
Enlargement of the spleen is an important criterion in diagnosing primary myeloproliferative diseases.1-3Because splenomegaly may occur in patients in whom the spleen is not palpable, the most sensitive imaging procedure for measuring splenic size has been sought. Nuclear medicine techniques, which are relatively complex and not routinely available, expose patients to radiation.4-6 One-dimensional ultrasonography (US) is often inaccurate.7 Computed tomography (CT) and magnetic resonance imaging are relatively expensive. Thus, stringent criteria for defining splenomegaly by using imaging methods are still controversial.1-7 We tested the accuracy of US-measured spleen volume compared with palpation and US-measured longitudinal diameter in detecting splenomegaly in patients with thrombocytosis subsequently classified as having myeloproliferative diseases or reactive conditions. We used a group of healthy subjects to establish reference ranges for US volume and a patient subgroup to assess variability in US measurements and examine the correlation between US-measured and CT-measured spleen volume.
Study design
In the past 3 years, we prospectively studied 73 consecutive patients (43 women and 30 men; median age, 50 years [range, 13-75 years]; median body-surface area, 1.7 m2[range 1.4-2.0 m2]) who presented with thrombocytosis (median platelet count, 720 × 109/L; range, 600-1898 × 109/L) of unknown origin. Patients with overt spleen enlargement (ie, 3 cm from the costal border at palpation) or with a disease associated with splenomegaly (eg, portal hypertension or thalassemia) were excluded from the study. Informed consent to participation was obtained from all subjects studied.
All spleen US scans were performed by the same operator, who used an EUB 525 Hitachi (Tokyo, Japan) instrument with a 2.5/3.5-MHz broadband curvilinear probe. The spleen was scanned in patients who were fasting, in the longitudinal and transverse planes by using an intercostal approach, a subcostal approach, or both. The patient was placed in a supine or right-sided position until complete organ visualization was achieved.8-10 Perimeter, longitudinal diameter, and area, defined as the maximum measurements with splenic borders and angles clearly defined, were measured, and volume (in milliliters) was calculated automatically. Reference values for volume were obtained from measurements in 15 healthy subjects matched with the patients for sex, age, and body-surface area. For each subject, the mean value of 3 measurements repeated on the same occasion was calculated and recorded for final analysis.
Twelve unselected patients were studied by repeated US measurements on 2 occasions at a 1-week interval by the same operator (intraobserver reproducibility) and by another operator unaware of the previous results, with both operators using the same US machine (interobserver reproducibility).11,12 After informed consent to participation was obtained again, the same 12 patients underwent a CT examination. Spleen axial images were obtained by using a multirow helical instrument (Mx 8000; Marconi Medical Systems, Cleveland, OH), to produce a 3-dimensional model used to calculate volumes automatically.13 Technical parameters included 6.5-mm slice width with identical reconstruction index, pitch 1, 200 mA, 120 kilovolt potential, and a rotation time of 0.75 seconds.
All patients underwent physical examination, full blood counts, assessment of blood smears and serum ferritin levels, and a search for possible causes of reactive thrombocytosis. Morphologic, cytogenetic, and molecular studies of bone marrow aspirates and a trephine biopsy with use of the Perls reaction for iron deposits and the silver-impregnation method for grading reticulin fibrosis were performed in all nonsecondary cases. In accordance with the updated criteria of the Polycythemia Vera Study Group,1 2 54 patients were found to be affected by essential thrombocythemia (ET), 4 by idiopathic myelofibrosis (IMF), and 15 by secondary thrombocytosis (ST) due to inflammatory conditions, iron-deficiency anemia, amyloidosis, or metastasizing malignant disease.
Statistical evaluations, including χ2 testing, analysis of variance with Bonferroni correction, and Pearson correlation, were performed with SPSS for Windows software (version 9.0; SPSS, Chicago, IL).
Results and discussion
Intraobserver reproducibility and interobserver reproducibility of measurements of spleen volume by US were excellent, with Pearson values of 0.999 and 0.997, respectively. Spleen-volume measurements by US and by CT scanning were strongly correlated, with a Pearson value of 0.945 (P < .001).
In the healthy subjects, spleen longitudinal diameter ranged from 8 to 11 cm (median, 9.5 cm) and spleen volume from 60 to 200 mL (median, 140 mL). Among the 73 patients studied, spleen enlargement was detected by palpation (between 0.5 and 2 cm below the costal margin) in 18, by US assessment of longitudinal diameter in 24, and by US assessment of volume in 38. A Pearson value of 0.407 indicated a clear disagreement between the volume and longitudinal-diameter measurements. Measurement of volume had significantly higher sensitivity in detecting splenomegaly compared with measurement of longitudinal diameter and palpation (52% versus 33% or 25%; P = .003). Of the 54 patients with ET, 16 (29%) had palpable splenomegaly, 22 (40%) had increased longitudinal diameter on US, and 34 (63%) had volume enlargement on US (overall median, 320 mL; range, 81-1000 mL). The difference in median spleen volume between patients with ET and healthy subjects was significant (P < .001). All 4 patients with IMF had marked spleen-volume enlargement (median, 670 mL; range 510-1000 mL), whereas only 2 of them had splenomegaly on palpation or US assessment of longitudinal diameter. In the group with ST, spleen-volume estimation by US was in the normal range (median, 110 mL).
In a preliminary analysis, we stratified the patients in the ET cohort according to US-measured spleen volume. Twenty patients with a normal volume (≤ 200 mL) had a median serum lactic dehydrogenase (LDH) level of 350 U/L (range, 200-509 U/L; normal value, 227-450 U/L) and no or mild bone marrow fibrosis; 18 patients with a spleen volume between 246 and 490 mL had a median LDH level of 452 U/L (range, 360-774 U/L), with mild to moderate bone marrow fibrosis in 11; and 16 patients with a spleen volume at least 500 mL had a median LDH level of 462 U/L (range, 200-748 U/L), with mild to moderate bone marrow fibrosis in 14. In 2 patients in the latter group, IMF developed after a median follow-up time of 12 months, whereas none of the patients in the other groups had onset of IMF after a median follow-up time of 18 months. Moreover, patients with ET and a spleen volume at least 500 mL had less response to a first-line interferon treatment; only one of the 5 patients in this group had normalization of platelet counts, compared with 11 of 14 patients in the groups with no to moderate (< 500 mL) spleen-volume enlargement.
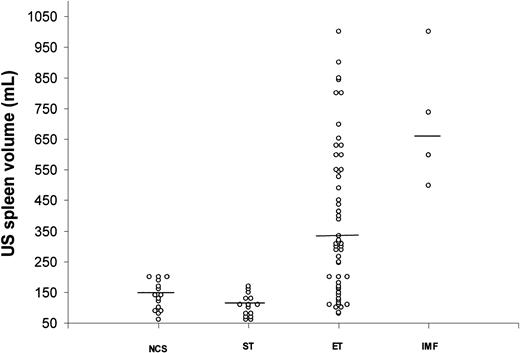
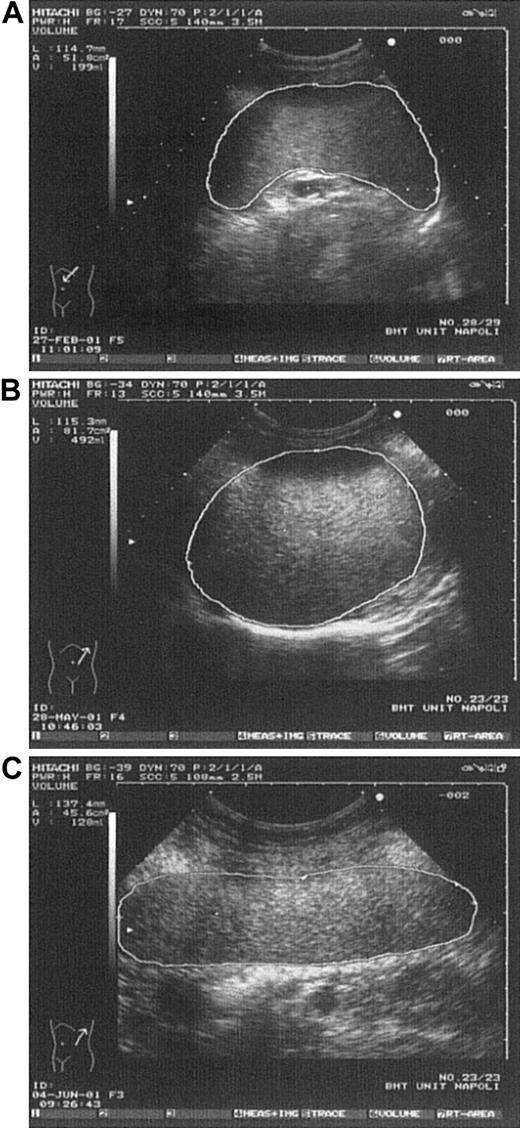
In conclusion, in contrast to other studies employing different methods,5-7 we found a high rate of splenomegaly in patients with ET by using US measurements of volume (Figure1). These findings are consistent with those of another series, in which spleen volume was measured by a radionuclide technique (single-photon emission CT).4Because the spleen is an irregularly shaped organ that may enlarge at different rates in its various dimensions, physical examination1-3 and imaging using one-dimensional measurements5-7 may underestimate the true organ size, thus suggesting an erroneously low incidence of splenomegaly in patients with ET. Multidimensional US spleen-volume measurement (defined as the integration of longitudinal diameter, perimeter, and area) is a rapid, reliable, and low-cost method for detecting the true spleen size (Figure 2). In addition, our data support the concept of clinical heterogeneity in patients with ET3,14 15; a role for spleen-volume measurement in subgrouping these patients will be better evaluated by studies in progress.
Spleen volume in healthy subjects and in patients with thrombocytosis.
Spleen volume was measured by US in healthy control subjects (NCS) and in patients with secondary thrombocytosis (ST), essential thrombocythemia (ET), or idiopathic myelofibrosis (IMF).
Spleen volume in healthy subjects and in patients with thrombocytosis.
Spleen volume was measured by US in healthy control subjects (NCS) and in patients with secondary thrombocytosis (ST), essential thrombocythemia (ET), or idiopathic myelofibrosis (IMF).
Various spleen shapes detected by US.
(A) Spleen in a control subject having normal longitudinal diameter and volume. (B) Spleen in a thrombocythemic patient having longitudinal diameter like that in Figure 2A but clearly enlarged volume. (C) Spleen in a control subject showing enlarged longitudinal diameter but normal volume (rodlike spleen).
Various spleen shapes detected by US.
(A) Spleen in a control subject having normal longitudinal diameter and volume. (B) Spleen in a thrombocythemic patient having longitudinal diameter like that in Figure 2A but clearly enlarged volume. (C) Spleen in a control subject showing enlarged longitudinal diameter but normal volume (rodlike spleen).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Bruno Rotoli, Divisione di Ematologia, Nuovo Policlinico, Via S Pansini 5, 80131, Naples, Italy; e-mail:rotoli@unina.it.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal