In a recent report on adults with idiopathic thrombocytopenic purpura (ITP), Portielje et al1 presented limited data on the morbidity and mortality attributed to the systemic effects of short-course corticosteroids in the context of initial treatment of ITP.2 Certain patients may be at high risk for unusual opportunistic infections.
In this letter we present a patient with ITP and no occupational hazard or apparent underlying disease who, during the course of treatment with oral methylprednisolone (MP), developed invasive bilateral pulmonary aspergillosis and multiple intracerebral lesions, presumably due to aspergillosis. We believe that this is the first reported case of cerebral aspergillosis after short-course corticosteroid treatment in an otherwise immunocompetent host with ITP.
A 52-year-old man was admitted to our department with asymptomatic severe thrombocytopenia (18 × 109/L), found on a routine full blood count (FBC). Clinical examination was unremarkable. Routine blood chemical values were normal, and tumor markers were negative. Serological tests for hepatitis B and C viruses, cytomegalovirus, Epstein-Barr virus, herpes simplex virus, herpes zoster virus, and human immunodeficiency virus (HIV) were negative. The patient had no clinical or laboratory evidence of autoimmune or immunodeficiency syndromes. Findings on chest radiograph and computed tomography (CT) scans of the chest, abdomen, and pelvis were normal. A bone marrow smear revealed normal numbers of megakaryocytes in an otherwise normal bone marrow, while antiplatelet IgG and IgM antibodies were positive. Treatment was initiated with 1 mg/kg oral MP daily, and 3 days later the patient was discharged after a prompt recovery of the platelet (PTL) count (70 × 109/L). The patient was followed up at the outpatient clinic, and tapering of MP was initiated after 4 weeks of treatment, while corticosteroid-induced type 2 diabetes mellitus developed. Eight weeks later, while on 24 mg MP daily, the patient was readmitted, afebrile and with a 3-day history of fatigue and palpitation. The FBC revealed a normal hemoglobin level and white blood cell and platelet counts. A radiograph of the chest showed patchy, nodular consolidations in both lungs. MP was tapered to 16 mg every other day (and discontinued on the 14th day of hospital stay), while cotrimoxazole, ceftriaxone, clarythromycin, and fluconazole were administered. Repeat virology (including HIV) and immunological laboratory tests again excluded any underlying autoimmune or immunodeficiency syndromes. Culture specimens of blood, sputum, and urine were negative for microorganisms. A bone marrow smear was unremarkable. Microscopical examination of a stained specimen of sputum showed no acid-fast bacilli. A urine test for legionella antigen was negative. On the fifth day of hospital stay, the patient became febrile (39°C) and developed a bloodstained productive cough. A chest radiograph revealed an increase in the bilateral nodular and patchy consolidations, while a CT scan of the chest on the eighth day of hospital stay showed bilateral multifocal nodules with cavitation. Amphotericin 1.5 mg/kg IV and itraconazole 400 mg daily were initiated. On the 10th day of hospital stay, a bronchoscopy was performed and aspergillus fumigatus was isolated from bronchoalveolar lavage fluid samples. The patient showed no clinical or radiological improvement over the following days and was switched to liposomal amphotericin 5 mg/kg, while itraconazole was increased to 800 mg daily. The patient showed a slow but stable improvement and, on the 27th day of hospital stay, became afebrile. On the 30th day of hospital stay, the patient developed a brief Jacksonian-type seizure. Magnetic resonance imaging (MRI) of the brain disclosed multiple (19 in total) ring-shaped brain abscesses. T1- and T2-weighted images showed low-intensity lesions containing high-intensity areas and high-intensity lesions, respectively (Figure 1). Cerebrospinal fluid (CSF) revealed a glucose level of 64 mg/dl (serum glucose 160 mg/dl), 2 cells/mm3, 15 RBC/mm3, and 55-mg/dl protein. Microscopic examination (gram staining, acid-fast bacilli, fungi) and CSF cultures were sterile. Serum and CSF enzyme-linked immunosorbent assay antigen test for IgA, IgM, and IgG toxoplasma gondii antibodies and CSF latex agglutination tests for aspergillus and cryptococcus neoformans antigens were negative. The good condition of the patient and the small size of the intracerebral lesions (the largest, 19 mm in diameter) discouraged neurosurgeons from performing a stereotactic biopsy. Although central nervous system (CNS) toxoplasmosis was most unlikely, a 2-week trial of sulfadiazine and pyramethamine was initiated, and follow-up CT scans of the brain failed to show improvement in the lesions, ruling out CNS toxoplasmosis. We persisted with antifungal treatment, and the pulmonary lesions gradually improved while the brain lesions remained unchanged in number and size. On the 60th day of hospital stay, the patient was discharged with itraconazole 400 mg daily, in good condition and with marked improvement of pulmonary lesions but stable cerebral lesions. Over the next months, follow-up CT scans showed a slow improvement of the intracerebral lesions, while a 12-month follow-up MRI scan disclosed complete resolution of these lesions (Figure2). The presenting features and the clinical course yielded an apparent diagnosis of cerebral aspergillosis.
Axial contrast-enhanced T1-weighted MRI image of the brain at diagnosis.
Multiple intraparenchymal lesions are detected, some with surrounding vasogenic edema. Characteristic ring-enhancing lesions are shown at the right inferior frontal gyrus and the corticomedullary junction of the left superior frontal gyrus.
Axial contrast-enhanced T1-weighted MRI image of the brain at diagnosis.
Multiple intraparenchymal lesions are detected, some with surrounding vasogenic edema. Characteristic ring-enhancing lesions are shown at the right inferior frontal gyrus and the corticomedullary junction of the left superior frontal gyrus.
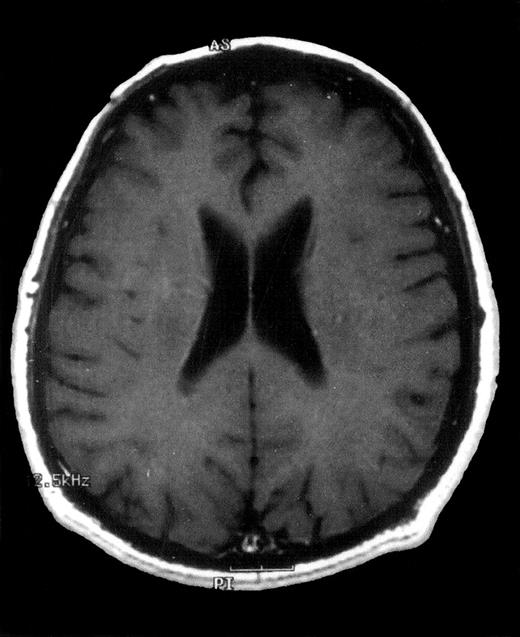
Axial contrast-enhanced T1-weighted MRI image of the brain 12 months after diagnosis.
Complete disappearance of intracerebral lesions after treatment with oral itraconazole.
Axial contrast-enhanced T1-weighted MRI image of the brain 12 months after diagnosis.
Complete disappearance of intracerebral lesions after treatment with oral itraconazole.
It is thought that vascular spread of aspergillosis is not a feature in immunocompetent patients. Immunosupression of a degree sufficient to permit the development of systemic disease in this patient was probably the result of the combination of two cofactors that compromised phagocytosis by macrophages and neutrophils: treatment with corticosteroids and hyperglycemia (a side effect often encountered in clinical practice). Although pneumonia due to aspergillosis in presumably immunocompetent hosts has received increased recognition over the years,3,4 this rare case of successfully treated cerebral aspergillosis suggests that short-course treatment with corticosteroids can exert deleterious systemic effects in certain patients with no evidence of autoimmune or immunodeficiency syndromes.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal