Portielje et al1 recently reported a study on the natural history of idiopathic thrombocytopenic purpura (ITP). Although the design of their study still falls short of a “gold-standard” inception cohort, prospective study required to reliably assess the natural history of a disease,2 their study represents the best available to date to assess the prognosis of adult patients with ITP. The study reaffirmed previous analysis of data that patients with mild and moderate thrombocytopenia have a benign course.3 Portielje et al1 now show that these patients do not have their life expectancy (LE) compromised. But they also show that patients with refractory ITP with persistently low platelet counts (below 30 000/μL) have 4.2-fold increased mortality risk in comparison with the general population. In this population the authors calculated the death rate of 0.019 cases per patient-year at risk. They compared this estimate with our estimate of the fatal bleeding rate in patients with refractory ITP of 0.0162 to 0.0389 cases per patient-year at risk.4 Our estimate, based on pooled data available in literature up to year 1998, showed a considerable compromise in LE in patients with refractory, untreated ITP.4 But by analyzing the cause of death, Portielje et al1 pointed out that half of the deaths were due not to bleeding but rather to the lethal infections likely related to the treatment.
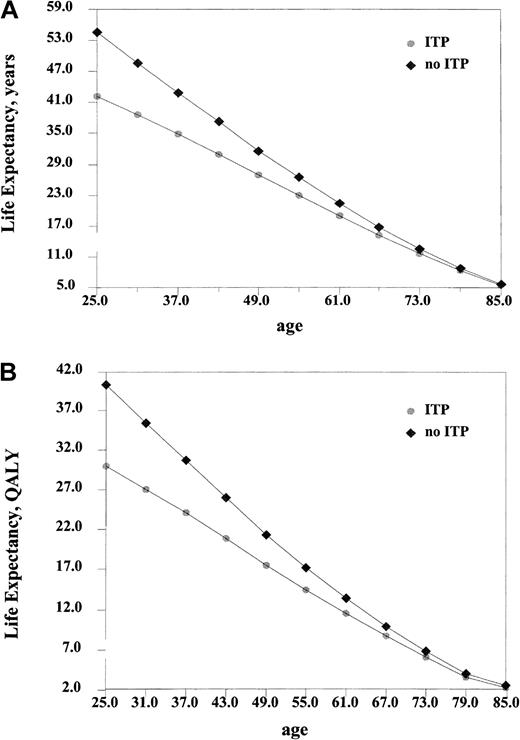
To investigate whether this suggested estimate of the fatal bleeding rate would change calculation of LE in refractory ITP, we assumed that the bleeding rate in refractory, untreated patients would amount to half of the death rate calculated by Portielje et al (= 0.019 / 2). Even with this new assumption, our model4 again demonstrates that LE and QALE (quality-adjusted life expectancy) in patients with refractory ITP are severely compromised (Figure 1). For a typical 30-year-old female, LE is decreased by 10.43 years (an average LE for a 30-year-old healthy female is 49.57 years and an average LE for a 30-year-old female with refractory ITP calculated in our model is 39.14 years) and by 8.72 of QALE (36.21-27.49). This result is based on the constant bleeding risk. We also analyzed the model assuming age-dependent bleeding risk (as was done in our original model). Unfortunately, Portielje et al did not provide death-rate calculations according to age. But since their estimate was quite close to ours (see above), we redid the analysis by assuming half of the fatal-bleeding age-adjusted risk in our original model. As expected, under these assumptions LE and QALE do not change significantly from the model based on the constant bleeding risk for younger patients but are significantly affected for older patients. For example, under the constant-bleeding risk model (Figure 1), a 60-year-old female with untreated refractory ITP will have LE decreased by 2.6 years compared with a healthy 60-year-old female. Under the age-adjusted risk model, a 60-year-old female would have LE decreased by almost 10 years (results not shown).
Life expectancy in refractory patients with ITP with persistently low (below 30 000/μL) platelet counts based on data for fatal bleeding risk by Portielje et al.1 QALY indicates quality-adjusted life years.
Life expectancy in refractory patients with ITP with persistently low (below 30 000/μL) platelet counts based on data for fatal bleeding risk by Portielje et al.1 QALY indicates quality-adjusted life years.
In conclusion, the best data so far indicate that patients with refractory, untreated ITP have a poor prognosis. If we are to believe the current data, then it is difficult to justify complacency in terms of a watchful waiting strategy. A separate issue is whether current available treatments do more good than harm, which neither our model nor Portielje et al's study was designed to answer. As we noted,4 the only way to settle the issue of prognosis is to perform a well-designed prospective inception cohort study of patients with refractory ITP. Until that study is done, recommendations that patients with refractory ITP and low counts should be merely observed is difficult to justify.
Mortality in adults with ITP
We thank Drs Djulbegovic and Cohen for their comments on our recently published study.1-1 As they point out, we estimated the rate of fatal hemorrhage for patients with refractory idiopathic thrombocytopenic purpura (ITP) at 0.019 cases per patient-year at risk (where time at risk was defined as time with fewer than 30 × 109/L platelets), using a method previously described by Cohen et al.1-2 Unfortunately, Drs Djulbegovic and Cohen erroneously assumed that nonhemorrhagic deaths were included in the death rate of 0.019. But this rate only represents fatal hemorrhages and is entirely in accordance with their original estimates obtained from pooled information from 17 case series.
Here we want to address 2 other important issues: First, nonhemorrhagic deaths should also be addressed when defining to what extent ITP compromises life expectancy. This led us to suggest that the only reliable estimate of the risk to die from ITP is obtained by comparing the mortality risk of patients with ITP with mortality risks in the general population, the method applied in our study. Second, hemorrhagic and nonhemorrhagic deaths should be differentiated. In our population, deaths due to lethal infections exceeded deaths due to bleeding, necessitating a discussion about the severe adverse effects of presently available treatment options for refractory ITP.
Therefore, although we did not advocate a “watchful waiting strategy,” our results underscore the fact that risks of hemorrhages and the risks of serious adverse effects must be carefully weighed when administering second-line treatment for refractory ITP.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal