Recently 2 papers dealing with strategies for management of cytomegalovirus (CMV) infection in patients receiving bone marrow transplantation (BMT) have made interesting suggestions,1 2 but we would like to make some comments.
Nichols et al1 found that a more than 2-fold increase of CMV pp65 antigenemia (as compared to baseline) occurring during preemptive anti-CMV treatment should be managed by induction or reinduction doses of antiviral drugs. But we think that the description of this strategy should be clarified. It is, in fact, unclear whether the definition of “baseline” pp65 refers to the levels that were observed when the patients first became positive or whether it refers to levels observed when they became positive again during maintenance treatment, although after a complete clearance (reactivation). Therefore, if they mean “baseline” as the first test with positive result, then considering the 2-fold increase seen in some patients, the reported levels of antigenemia ranging from 0.5 to 1382 cells/slide could reach levels ranging from 1 to 2 but also from 1382 to 2764 (including all the possible intermediate values). We cannot wait for such levels to be reached before changing the antiviral drugs.
Ljiungman et al2 dealt with cidofovir administration for management of pp65 antigenemia. In this paper, they reported a 66% efficacy of cidofovir in patients who failed or relapsed after previous preemptive therapy. Unfortunately, the authors did report which strategies were adopted strategies in the one-third of patients who failed after cidofovir “rescue.”
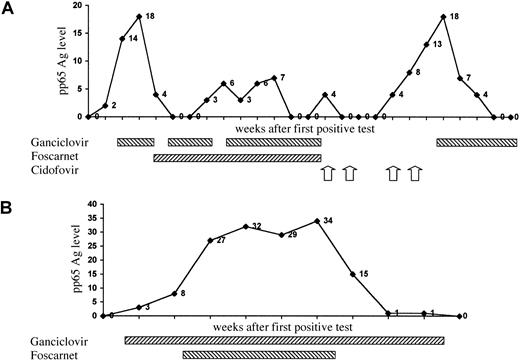
We recently treated 2 pediatric patients receiving matched unrelated donor BMT whose CMV pp65 antigenemia increased during preemptive or maintenance therapy. The time course of CMV antigenemia, the treatment administered, and its “efficacy” are shown in Figure1.
Time course of CMV pp65 antigenemia and antiviral drugs administered.
(A) patient 1; (B) patient 2. The 4 arrows refer to each single dose of cidofovir.
Time course of CMV pp65 antigenemia and antiviral drugs administered.
(A) patient 1; (B) patient 2. The 4 arrows refer to each single dose of cidofovir.
In our first case (Figure 1A), since other antiviral drugs proved to be ineffective, cidofovir was administered to the patient.2When relapse occurred during cidofovir maintenance therapy, we used the same drug after doubling of antigenemia levels, though unsuccessfully. But the same patient responded to ganciclovir, as already reported in another case.3 In the second case (Figure 1B), we observed an increase in pp65 antigenemia despite association therapy with ganciclovir and foscarnet.4 A spontaneous decrease in antigenemia was then observed in this patient without making any changes in immunosuppressive and antiviral therapy.
In both of the patients, in agreement with Nichols et al1we observed that the role of antiviral resistance is probably not very important in determining the time course of pp65 antigenemia in allogeneic BMT recipient. Other unknown factors should likely be considered pivotal in the outcome of these patients.
From our experience, we believe that some clarifications, such as a more clear definition of “baseline” and of “2-fold increase” levels in the first paper,1 and a description of treatment administered in patients who failed to respond to cidofovir administration in the second one,2 would be useful for studying the best strategies for management of relapsing pp65 antigenemia.
Cidofovir against cytomegalovirus after allogeneic stem cell transplantation
It was interesting to see the results from the prospective study by Kiehl and Basara using cidofovir as a first-line preemptive therapy against cytomegalovirus (CMV) after allogeneic stem cell transplantation. The results from their study seem to differ very much from those reported in our recent study.1-1 But the 2 studies do not differ in the response to full-dose cidofovir (58% in our study, 76% in Kiehl and Basara's). Instead, the difference is in a higher relapse rate in the study by Kiehl and Basara. In a recent study by Reusser et al for the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation (EBMT) comparing ganciclovir and foscarnet, it was shown that relapse defined as reappearance of CMV DNA detected by PCR or of pp65 antigenemia is common also when patients are treated by either of these 2 antiviral drugs.1-2 The difference is that in Kiehl and Basara's study reappearance of CMV DNA occurred during maintenance therapy, while in the EBMT study the relapse occurred rapidly after discontinuation of therapy. There are at least 3 possibilities to explain the differences:
First, the risk profile of the patients might differ, such as the type of transplantations performed, the GVHD prophylaxis used, the grades of GVHD, conditioning therapy, and types of donors. This cannot be ascertained by the details given in Kiehl and Basara's letter. But most of their patients had received unrelated donor transplants, indicating a high-risk group.
Second, the diagnostic procedures used for CMV in the different studies might be different. All patients receiving cidofovir as first-line preemptive therapy in our study was monitored by pp65 antigenemia. Kiehl and Basara's study used PCR and antigenemia for monitoring but PCR for definition of relapse. In fact, they give no data at all regarding the results of the antigenemia assay after discontinuation of cidofovir. Furthermore, it is not stated what the material used for the PCR was (leukocytes, plasma, or whole blood). It would be interesting to determine the viral load by quantitative PCR, but viral load determinations were not performed in our study or in Kiehl and Basara's. But Bosi et al1-3 recently presented data at the recent EBMT meeting, indicating that patients with low viral loads have a better response to cidofovir than patients with high viral loads.
Third, treatment schedules might differ, for example, whether the third cidofovir dose was given after 2 or 3 weeks from start of therapy (see below).
These differences can only be controlled in a prospective and randomized study. This was proposed in our paper and is supported in Kiehl and Basara's letter. It is important to point out, however, that when Kiehl and Basara state that their data contradicts our conclusions, this is an incorrect representation of our conclusions. We clearly state that “additional studies are needed before cidofovir can be recommended for preemptive therapy”1(p388) and “we believe that randomized, comparative studies are indicated before CDV is introduced as an accepted agent for first-line preemptive therapy.”1(p391) In our opinion, the most important result from our study is that cidofovir can be used in allogeneic stem cell transplant patients with a risk for toxicity, allowing further studies. This is confirmed by Kiehl and Basara's letter and, thereby, hopefully will make prospective, randomized studies possible.
Castagnola et al ask for the strategies used for patients failing cidofovir “rescue” in our paper. It is important to note that the indication for secondary preemptive therapy could be either relapse or no response to previously given antiviral therapy. Thus, many of the patients were in fact treated for recurring antigenemia or DNAemia rather than increasing antigenemia. Unfortunately, due to the retrospective nature of our study, we do not have the information requested by Castagnola et al. But we agree that both for patients followed by pp65 antigenemia and for those followed by qualitative PCR, low-degree positivity in either of the assays has a low predictive value after antiviral therapy. Furthermore, it is important to differentiate between failure of an antiviral agent to turn a positive test to negative and development of relapse in either antigenemia or DNAemia after the indicator test has become negative. The former probably has to do with viral kinetics and the built-in characteristics of the assay used. The latter is also dependent on the ability of the patient to mount a long-term immune response to handle the virus. It is possible that wider usage of true quantitative assays can give additional important information.
There is one other important question regarding cidofovir raised by both letters. When shall the third cidofovir dose be given? From Castagnola et al's Figure 1, it seems that the third dose was given 2 weeks after the second dose. This is very different from how we give ganciclovir or foscarnet when 2 weeks' induction therapy usually is followed directly by maintenance, although in a lower dose. This means that a patient has therapeutic levels of cidofovir for approximately 2 weeks and then there is a 1-week interval before the drug is given again.
References
Rising cytomegalovirus antigenemia on preemptive therapy: practical aspects
Our study of 119 allogeneic transplant recipients who developed pp65 antigenemia early after transplantation demonstrated that host factors (primarily the dose of corticosteroids administered for graft-versus-host disease [GVHD]), not resistance to antivirals, explain the phenomenon of rising viral load during the first 1-2 months of preemptive therapy.2-1 Thus, we concluded that empiric switches from ganciclovir to foscarnet (to restore activity against ganciclovir resistant strains of cytomegalovirus [CMV]) are not usually necessary. Rather, dose intensification (continued induction dosing or reinduction dosing) should be used as a first-line strategy in the management of these patients.
Castagnola et al raise important issues regarding the practical application of this strategy. The first issue concerns the precise definition of increases of greater than twice baseline. As indicated in “Patients and methods,” we defined the “baseline” antigenemia level as the number of positively staining cells obtained at the first positive test. An increase from 1 cell (at the first positive test) to 2 cells on any subsequent test was thus defined as an increase of 2 times baseline. Operationally, this criterion was met predominantly among patients with low initial antigenemia levels: of 47 patients with greater than 2-fold increases over baseline, 25 (53%) had initial antigenemia levels of no more than 2, and 12 (26%) had initial antigenemia levels of 2.5-10, while only 10 (21%) had initial antigenemia levels above 10. As discussed in the article, initial antigenemia levels did not predict CMV disease in this cohort of patients who were receiving preemptive therapy.
Castagnola et al also refer to the time course of the antigenemia increase. Rising antigenemia was assessed regardless of when the increase occurred. As presented, however, the majority (90%) of patients whose antigenemia levels rose on therapy did so within the first 2 weeks: 43% after 1 week of induction therapy and 47% after 2 weeks of therapy (when the majority had received only 1 week of maintenance therapy). Thus, in our cohort of non–T-cell–depleted patients, these were events that tended to occur early in the course of antiviral therapy rather than during prolonged courses of maintenance therapy. This pattern may be quite different in the patient who receives ganciclovir prophylaxis,2-2 T-cell–depleted transplants,2-3 or salvage therapies for GVHD, all of which impair the recovery of CMV-specific T-cell immunity.
It is difficult to speculate about the possible reasons for failure in the patients presented by Castagnola et al with the limited information provided on the exact timing of events, net status of immunosuppression, and dose regimens of the antiviral drugs. But there are several factors that could be responsible for the failure of antigenemia clearance in the first patient (Figure 1A), including the underlying immunosuppressive regimen or changes thereof, changes in GVHD status, the dosing interval of cidofovir (1 versus 2 weeks), or drug resistance. Also, there are reports in HIV-infected individuals that clearance of CMV from the blood can take a long time with cidofovir, despite efficacy in the treatment of end-organ disease.2-4 The pattern displayed in the second patient (Figure 1B) is compatible with delayed clearance of antigenemia in the presence of anti-CMV treatment. This may occur in a small number of allogeneic stem cell transplant recipients, usually those on intense immunosuppression.
Some final words regarding the quantitative nature of the antigenemia assay are warranted. While the antigenemia assay provides useful data on the quantitative CMV viral load, there are very few data on the interassay variability of antigenemia quantitation. Variability of quantitative results is usually much greater at the lower ranges of antigenemia levels (from 0.5 to 2 cells/slide) when compared to the upper ranges (more than 10 cells/slide). Thus, multiplicative increases in antigenemia may be more reflective of “true” increases in viral load if the initial antigenemia level is higher. Nevertheless, modeling an increase of twice baseline was most correlated with breakthrough CMV disease in our retrospective cohort; regardless of the initial level of antigenemia, rises of twice baseline while on preemptive antiviral therapy appear to reflect the host's inability to control viral replication. In subjects with rising antigenemia levels, continuation of induction dosing or reinduction is now standard practice at our center for those with twice baseline increases. For those patients with very high initial antigenemia levels (more than 100 cells/slide), clinically significant increases may be present even before the cut point of twice baseline is met, especially in patients who are severely immunosuppressed. But in these cases the determination of what is a “true” increase must include consideration of the coefficient of variation of the quantitation method. Since quantitative aspects of antigenemia testing may vary with assay modifications,2-5determination of the coefficient of variation may be required for each individual assay.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal