Acute myeloid leukemia (AML) in older adults carries a poor prognosis, and the optimum treatment remains to be determined. In younger patients, treatment stratification is frequently based upon diagnostic karyotype, which was the most important prognostic factor in the UK Medical Research Council (MRC) AML10 trial. Considered here is whether karyotype is also predictive in older adults; this is done by studying 1065 cases from MRC AML11 (median age, 66 years). Three prognostic groups were distinguished on the basis of response to induction therapy and overall survival (OS). Those with t(15;17), t(8;21), or inv(16) composed the favorable risk group. Overall, these abnormalities predicted a superior complete remission (CR) rate (72%), reflecting relatively low levels of resistant disease (RD) (8%), and lower relapse risk (RR) (56%) associated with superior OS (34% at 5 years). Normal karyotype (CR, 63%; RD, 17%; RR, 78%; OS, 15%) and other noncomplex abnormalities (CR, 53%; RD, 32%; RR, 85%; OS, 10%) composed the intermediate group; while complex karyotype predicted an extremely poor prognosis (CR, 26%; RD, 56%; RR, 91%; OS, 2%). Combining MRC AML10 and AML11 (n = 2677) revealed that the most favorable changes were rarer in older patients (younger than 55 years, 24%; 55 years or older, 7%), while complex abnormalities were more common (6% vs 13%). This study suggests that hierarchical cytogenetic classification identifies biologically distinct subsets of AML that are represented in all age groups. Furthermore, it highlights the importance of karyotype as a critical independent determinant of outcome in older patients with AML, providing a potential framework for stratified treatment approaches.
Introduction
Acute myeloid leukemia (AML) occurring in adults older than 55 years of age is associated with an extremely poor prognosis with an overall survival (OS) of less than 20% at 5 years (reviewed by Hiddemann et al1; see accompanying paper by Goldstone et al,2 page 1302). A number of factors have been implicated in the adverse outcome of this group in comparison with younger individuals. These include poorer tolerance of combination chemotherapy regimens leading to the use of less intensive treatment protocols, as well as increased levels of primary drug resistance associated with overexpression of P-glycoprotein (P-gp), which may in part reflect a higher incidence of secondary leukemias (reviewed by Willman3). Furthermore, poor prognosis in this age group has been ascribed to an increased frequency of adverse cytogenetic features.4 5 However, the prognostic implications of diagnostic karyotype remain to be established in large numbers of older adults subject to an intensive treatment approach.
Despite the generally poor outcome of AML in the elderly, it is of paramount importance to distinguish subgroups of patients with potentially curable disease, who are likely to benefit from treatment, from patients who are essentially incurable with current therapeutic approaches and whose quality of life can perhaps be improved by supportive measures, rather than intensive therapy. To begin to address these issues, it is necessary to identify prognostic factors that could provide the basis for a more rational treatment strategy for AML arising in older adults. A number of previous studies have identified diagnostic cytogenetics as a key determinant of outcome in AML (reviewed by Mrózek et al6,7) although in many instances the prognostic significance of specific abnormalities was difficult to determine owing to relatively small sample sizes and/or variations in treatment approach. However, in the largest study to date, which considered 1612 children and younger adults (mostly younger than 55 years) from the UK Medical Research Council (MRC) AML10 trial, we defined 3 cytogenetic prognostic groups that predicted response to induction therapy, relapse risk (RR), and OS.8 Patients with t(8;21)(q22;q22), t(15;17)(q22;q21), or inv(16)(p13q22) were found to have a relatively favorable prognosis; in the absence of these changes, the presence of a complex karyotype, monosomies of chromosome 5 or 7 (−5, −7), deletions of long arm of chromosome 5 (del[5q]/5q−), or 3q abnormalities predicted an adverse prognosis. The remaining patients, including those with normal karyotype or structural or numerical changes not encompassed by the favorable or adverse risk groups, had an intermediate prognosis. This cytogenetic classification system and response to the first course of chemotherapy were found to provide the 2 most important prognostic factors in the MRC AML10 trial.9 Therefore, these 2 parameters have subsequently been used to determine treatment strategy for AML patients younger than 60 years of age entered into the MRC trials. Patients with favorable cytogenetic abnormalities are no longer transplanted in first complete remission (CR), while patients with adverse cytogenetic features are treated according to a separate protocol (MRC AML-HR).
It is essential that proposed cytogenetic classification systems be subject to validation in fresh data sets, with consideration given to possible influences of age and treatment approach, as highlighted recently by Slovak et al.10 In the present study, through analysis of 1065 cases entered into the MRC AML11 trial, we sought to determine whether the cytogenetic risk groups previously defined in children and younger adults entered into MRC AML108 are also predictive of outcome in older individuals.
Patients and methods
Patients
The MRC AML11 trial was open from November 1990 to June 1998, accruing 1314 patients (median age 66, range 44-91 years); 1002 were registered as having de novo AML, and 299 as secondary AML, while the remaining 13 patients were excluded from further analysis: 12 who were subsequently found not to have untreated AML and 1 who was entered into the MRC AML12 trial instead. One patient with de novo AML was also excluded from the analysis as no follow-up data were available. Cases of AML were classified as secondary on the basis of a history of previous exposure to chemotherapy/radiotherapy (n = 44), antecedent hematologic condition including myelodysplasia (n = 181), myeloproliferative condition (n = 21), or other miscellaneous hematological disorders (n = 31). The reason was unspecified in 22 cases.
Therapy
Details of the MRC AML11 treatment protocol are described in the accompanying paper.2 Patients were randomized to receive 2 courses of daunorubicin, ara-C, 6-thioguanine (DAT) (course 1, DAT 3 + 10, course 2, DAT 2 + 5); ara-C, daunorubicin, etoposide (ADE) (course 1, ADE 10 + 3 + 5, course 2, ADE 5 + 2 + 5); or mitoxantrone, ara-c (MAC) (course 1, MAC 3 + 5, course 2, MAC 2 + 5); followed by a common third treatment course consisting of DAT 2 + 7. Patients were then randomized to receive no further chemotherapy versus an extended consolidation of 3 further courses of chemotherapy consisting of cyclophosphamide, vincristine, ara-C, prednisolone (COAP), followed by DAT 2 + 5 and COAP. Patients were also randomized to interferon-α maintenance for 12 months versus no interferon-α. There were no significant differences in the treatment received according to the cytogenetic abnormality detected at diagnosis. From January 1993, those with a clinical diagnosis of acute promyelocytic leukemia (APL) were eligible for the MRC all-transretinoic acid (ATRA) trial whereby 40 patients were randomized to receive either short or extended courses of ATRA in addition to the AML11 treatment protocol, as previously described.11
Cytogenetics
Cytogenetic analyses were performed as described previously.8 Cytogenetic data were available for 1065 of 1300 eligible AML11 patients, representing 82% of cases of AML in the trial. Among patients reported to have a normal karyotype (n = 507), outcome of the 34 cases with fewer than 20 metaphases analyzed (range 10-19; median 14) did not differ from those with at least 20 metaphases studied, and hence they were retained within the normal karyotype group. A diagnostic result was not available in 235 cases either because cytogenetic studies were not performed (n = 16) or failed (n = 98) or for unknown reasons. To determine whether there was any association between age and the frequency of secondary leukemias and specific cytogenetic abnormalities, data derived from the AML11 trial were combined with data derived from the previously reported AML10 trial, which considered cytogenetic findings in 1612 AML patients, mostly younger than 55 years of age.8,12 Analyses were restricted to the more frequently observed abnormalities, ie, those found in 10 or more patients. We also sought to determine among AML11 cases whether the hierarchical cytogenetic risk-group classification that we previously defined in younger patients with AML8was of predictive value in older patients. According to this classification, cases with t(8;21), t(15;17), or inv(16), irrespective of the presence of additional cytogenetic abnormalities, composed the favorable risk group, while cases lacking these favorable risk aberrations in which complex cytogenetic changes (5 or more unrelated abnormalities), −5, del(5q), −7, or 3q abnormalities were identified composed the adverse risk group. The remaining group of patients composed the intermediate risk category, which included cases with normal karyotype, 11q23 abnormalities, trisomy 8 (+8), or other chromosomal changes not encompassed by the favorable or adverse risk groups. In analyses using hierarchical cytogenetic classification, patients were defined by the primary abnormality and hence were counted only once (Tables 3, 4, 6; Figures 1-3).
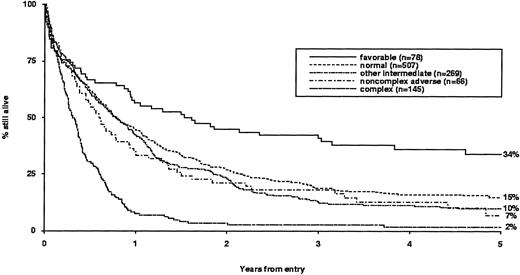
Overall survival in MRC AML11 trial by hierarchical cytogenetic abnormality.
Survival and risk of relapse.
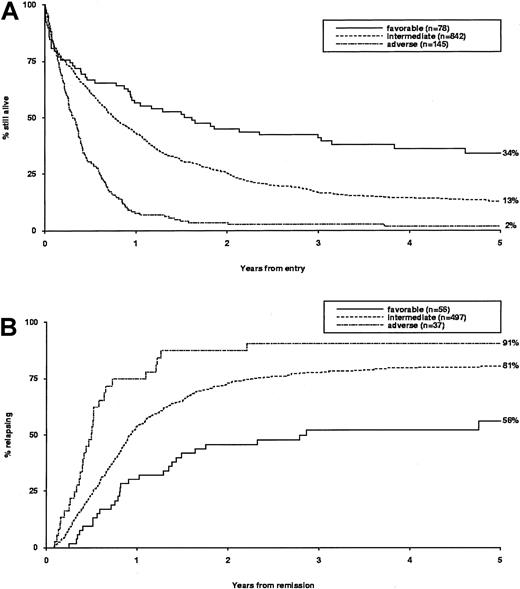
Overall survival (A) and relapse risk (B) in MRC AML11 trial are shown by hierarchical risk group. Outcome is shown applying the revised hierarchical risk group classification that was found to be more predictive in older adults than the original scheme devised in younger patients entered into the MRC AML10 trial. The revised risk groups were as follows. Favorable group: t(15;17), t(8;21), or inv(16), whether alone or in conjunction with other abnormalities. Intermediate group: normal karyotype, all other noncomplex abnormalities. Adverse group: complex karyotype (5 or more unrelated abnormalities), excluding cases with t(15;17), t(8;21), and inv(16).
Survival and risk of relapse.
Overall survival (A) and relapse risk (B) in MRC AML11 trial are shown by hierarchical risk group. Outcome is shown applying the revised hierarchical risk group classification that was found to be more predictive in older adults than the original scheme devised in younger patients entered into the MRC AML10 trial. The revised risk groups were as follows. Favorable group: t(15;17), t(8;21), or inv(16), whether alone or in conjunction with other abnormalities. Intermediate group: normal karyotype, all other noncomplex abnormalities. Adverse group: complex karyotype (5 or more unrelated abnormalities), excluding cases with t(15;17), t(8;21), and inv(16).
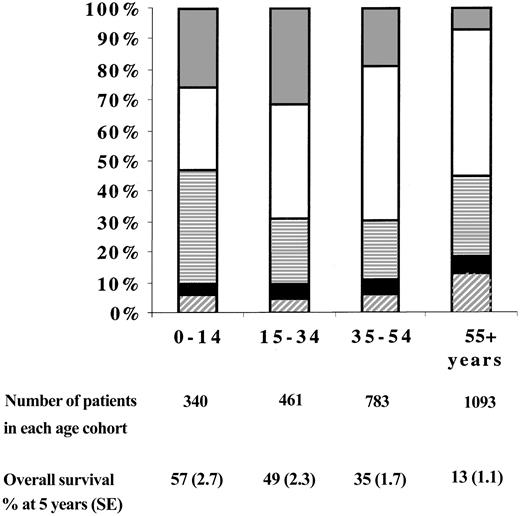
Distribution of hierarchical cytogenetic abnormalities and overall survival by age among patients entered into MRC AML10 and AML11 trials (n = 2677).
In children and younger adults (younger than 55 years), normal and other intermediate groups compose the intermediate (standard) cytogenetic risk category, while those with complex karyotype (5 or more unrelated abnormalities) or adverse changes in a noncomplex karyotype compose the adverse risk group.8 In older adults (55 years or older), a revised hierarchical classification in which cases with noncomplex adverse abnormalities were reassigned to the intermediate risk category was found to be more predictive of outcome. ░ indicates favorable; ■, normal; ▤, other intermediate; ▪, noncomplex adverse; ▨, complex.
Distribution of hierarchical cytogenetic abnormalities and overall survival by age among patients entered into MRC AML10 and AML11 trials (n = 2677).
In children and younger adults (younger than 55 years), normal and other intermediate groups compose the intermediate (standard) cytogenetic risk category, while those with complex karyotype (5 or more unrelated abnormalities) or adverse changes in a noncomplex karyotype compose the adverse risk group.8 In older adults (55 years or older), a revised hierarchical classification in which cases with noncomplex adverse abnormalities were reassigned to the intermediate risk category was found to be more predictive of outcome. ░ indicates favorable; ■, normal; ▤, other intermediate; ▪, noncomplex adverse; ▨, complex.
Definitions of end points
A normocellular bone marrow aspirate containing fewer than 5% blasts and showing evidence of normal maturation of other marrow elements was the criterion for the achievement of CR. Persistence of myelodysplastic features did not exclude the diagnosis of CR. As in previous MRC AML trials, full recovery of normal peripheral blood counts was not required to define CR, although at least 95% of patients considered to be in CR according to the protocol definition also satisfied National Cancer Institute criteria.13Remission failures were classified by the referring clinician either as due to induction death (ID), ie, related to treatment and/or hypoplasia, or as resistant disease (RD), ie, related to the failure of therapy to eliminate the disease (including partial remissions with 5% to 15% blasts). Where the clinician's evaluation was not available, deaths within 30 days of entry were classified as ID and deaths at more than 30 days as RD. The following definitions are also used: OS is the time from entry to death. For remitters, the RR is the cumulative probability of relapse, ignoring (ie, censoring at) death in CR.
Statistical methods
The Mantel-Haenszel test for trend, Fisher exact test, and the Wilcoxon 2 sample test were used to test for associations with age, type of AML, and white blood cell count (WBC) at presentation. Remission rates and reasons for failure to achieve CR were compared by means of the Fisher exact test. Kaplan-Meier life tables were constructed for survival data and were compared by means of the log-rank test, with surviving patients being censored on June 1, 2000 (AML11), or May 1, 1999 (AML10), when follow-up was complete for at least 98% of patients (the small number of patients lost to follow-up are censored at the date they were last known to be alive). Median follow-up was 54 months (range, 1-112 months) in AML11 and 80 months (range, 4-131 months) in AML10 patients with cytogenetic data. AllP values are 2-tailed; because of the large number of significance tests performed and the associated increased probability of obtaining conventionally significant (P < .05) results by chance, only values of P < .01 are quoted.
Results
Incidence of specific cytogenetic abnormalities in AML in older adults
The frequency of the most common cytogenetic abnormalities detected at diagnosis among 1065 cases of AML arising in older adults entered into the MRC AML11 trial and their associated clinical features are presented in Table 1. The most common recurring cytogenetic abnormalities among the de novo AML group were a complex karyotype, +8,−7/del(7q), −5/del(5q), and t(15;17). The spectrum of abnormalities observed in cases of secondary AML was similar; however, the occurrence of a complex karyotype, +8, −7, and other structural changes was significantly more frequent. No significant variation in frequency of particular abnormalities across the age range of patients entered into the trial was noted, with the exception of t(15;17) and del(7q), which were more common in younger patients.
Frequency and percentage of cytogenetic abnormalities in Medical Research Council trial AML11
| Abnormality . | All patients (n = 1065), no. (%) . | Age group, y . | Median age, y . | Median initial WBC* . | Type of AML . | |||
|---|---|---|---|---|---|---|---|---|
| Younger than 65 (n = 440), % . | 65-69 (n = 334), % . | 70 and older (n = 291), % . | de novo (n = 817), % . | Secondary (n = 248), % . | ||||
| Overall | 66 | 10.9 | ||||||
| No abnormality | 507 (48) | 45 | 47 | 52 | 66 | 19.8 | 50 | 39 |
| Complex | 146 (14) | 12 | 19 | 11 | 66 | 4.3† | 12 | 18‡ |
| +8 | 109 (10) | 10 | 10 | 11 | 67 | 6.4† | 9 | 15† |
| −7 | 87 (8) | 8 | 9 | 7 | 66 | 4.7† | 7 | 13† |
| del(5q) | 80 (8) | 7 | 10 | 5 | 66 | 4.3† | 7 | 10 |
| −5 | 55 (5) | 4 | 7 | 4 | 66 | 2.8† | 5 | 7 |
| del(7q) | 48 (5) | 6 | 3 | 3‡ | 64 | 5.2‡ | 4 | 5 |
| t(15;17) | 43 (4) | 6 | 4 | 2‡ | 63† | 1.7† | 5 | 1 |
| abn(3q) | 27 (3) | 2 | 4 | 2 | 66 | 7.0 | 2 | 4 |
| +21 | 26 (2) | 2 | 3 | 3 | 67 | 7.8 | 2 | 3 |
| del(9q) | 24 (2) | 3 | 2 | 1 | 64 | 10.1 | 2 | 2 |
| t(8;21) | 23 (2) | 3 | 2 | 2 | 65 | 13.0 | 2 | 2 |
| +22 | 15 (1) | 2 | 2 | 1 | 65 | 3.3‡ | 1 | 2 |
| inv(16) | 12 (1) | 1 | 1 | 1 | 65 | 11.3 | 2 | 0 |
| 11q23 | 11 (1) | 1 | 1 | 1 | 64 | 9.0 | 1 | 2 |
| Other numerical | 277 (26) | 25 | 28 | 25 | 66 | 5.5† | 25 | 29 |
| Other structural | 295 (28) | 28 | 31 | 23 | 66 | 5.4† | 25 | 38† |
| Abnormality . | All patients (n = 1065), no. (%) . | Age group, y . | Median age, y . | Median initial WBC* . | Type of AML . | |||
|---|---|---|---|---|---|---|---|---|
| Younger than 65 (n = 440), % . | 65-69 (n = 334), % . | 70 and older (n = 291), % . | de novo (n = 817), % . | Secondary (n = 248), % . | ||||
| Overall | 66 | 10.9 | ||||||
| No abnormality | 507 (48) | 45 | 47 | 52 | 66 | 19.8 | 50 | 39 |
| Complex | 146 (14) | 12 | 19 | 11 | 66 | 4.3† | 12 | 18‡ |
| +8 | 109 (10) | 10 | 10 | 11 | 67 | 6.4† | 9 | 15† |
| −7 | 87 (8) | 8 | 9 | 7 | 66 | 4.7† | 7 | 13† |
| del(5q) | 80 (8) | 7 | 10 | 5 | 66 | 4.3† | 7 | 10 |
| −5 | 55 (5) | 4 | 7 | 4 | 66 | 2.8† | 5 | 7 |
| del(7q) | 48 (5) | 6 | 3 | 3‡ | 64 | 5.2‡ | 4 | 5 |
| t(15;17) | 43 (4) | 6 | 4 | 2‡ | 63† | 1.7† | 5 | 1 |
| abn(3q) | 27 (3) | 2 | 4 | 2 | 66 | 7.0 | 2 | 4 |
| +21 | 26 (2) | 2 | 3 | 3 | 67 | 7.8 | 2 | 3 |
| del(9q) | 24 (2) | 3 | 2 | 1 | 64 | 10.1 | 2 | 2 |
| t(8;21) | 23 (2) | 3 | 2 | 2 | 65 | 13.0 | 2 | 2 |
| +22 | 15 (1) | 2 | 2 | 1 | 65 | 3.3‡ | 1 | 2 |
| inv(16) | 12 (1) | 1 | 1 | 1 | 65 | 11.3 | 2 | 0 |
| 11q23 | 11 (1) | 1 | 1 | 1 | 64 | 9.0 | 1 | 2 |
| Other numerical | 277 (26) | 25 | 28 | 25 | 66 | 5.5† | 25 | 29 |
| Other structural | 295 (28) | 28 | 31 | 23 | 66 | 5.4† | 25 | 38† |
Percentages indicate percentage of column total. Percentages do not add to 100 because patients with more than one abnormality are counted more than once. P values are for Mantel-Haenszel test for trend in age (grouped), for Wilcoxon 2-sample test in age and initial WBC (continuous), and for Fisher exact test in type of AML, comparing each abnormality with normal karyotype (ie, no abnormality).
WBC indicates white blood count; AML, acute myeloid leukemia; abn, abnormal.
Initial WBC was not recorded for 22 patients.
P < .001.
P < .01.
A number of cytogenetic abnormalities were associated with a lower presenting WBC, including cases with del(5q)/−5, del(7q)/−7, +8, t(15;17), and complex karyotype. Lower presenting WBC also occurred in cases with other numerical and structural changes, particularly if associated with complex karyotype or abnormalities of chromosomes 5 or 7.
Frequency of additional cytogenetic abnormalities in AML arising in older adults: analysis of cases derived from MRC AML11
To further characterize the cytogenetic features of AML arising in older adults, the frequency of additional changes occurring in conjunction with primary chromosomal aberrations among cases derived from the MRC AML11 trial was determined (Table2). For this analysis, cases were classified according to the original hierarchical system devised for children and younger adults entered into MRC AML10.8Favorable risk abnormalities, ie, t(15;17), t(8;21), or inv(16), were detected in 78 of 1065 (7%) AML11 cases and were accompanied by additional changes in 47%, 74%, and 42% of cases, respectively. In the majority, the additional changes were from the intermediate risk group of abnormalities: t(15;17) was most commonly associated with +8 (12%) and miscellaneous other structural changes (26%); t(8;21) with del(9q) (9%) and with other numerical abnormalities (57%), particularly loss of a sex chromosome (52%); and inv(16) was accompanied by del(7q) (17%) or other structural (17%) or other numerical (25%) changes. The majority of cases classified within the intermediate hierarchical risk group had a normal karyotype (507 of 776 cases, 65%); multiple intermediate abnormalities were detected in 83 of 776 cases (11%); while in the remaining 186 intermediate risk group cases a single aberration was detected: most commonly, +8 (22%), del(9q) (5%), del(7q) (3%), +21 (3%), and 11q23 (2%) rearrangements (Table 2); the rest were composed of miscellaneous structural or numerical changes with an individual frequency of fewer than 10 cases. Overall, 211 of 1065 cases were assigned to the adverse cytogenetic risk category; in 145 of 211 cases (69%), this was based on the presence of a complex karyotype, of which 65 (45%) possessed one adverse cytogenetic abnormality (eg, −5) and 47 (32%) possessed 2 or more. Hence, adverse cytogenetic aberrations frequently occurred in conjunction with one another as part of a complex karyotype. Furthermore, complex karyotypes inevitably included cytogenetic abnormalities, which in their own right would have been considered intermediate risk; it is of note that 63% of cases of del(7q), 50% of cases of +21, and 30% of cases of +8 occurred as part of a complex karyotype (Table 2). The remaining patients in the adverse cytogenetic risk group were classified on the basis of the presence of adverse cytogenetic features occurring in the context of a less complex karyotype (44 of 211 patients, 21%) or, uncommonly, as the sole aberration (22 of 211 patients, 10%).
Characterization of additional cytogenetic changes associated with primary chromosomal aberrations in Medical Research Council trial AML11
| . | Cytogenetic aberration . | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total . | t(15;17) . | t(8;21) . | inv(16) . | +8 . | 7q− . | +21 . | 9q− . | +22 . | 11q23 . | Other structural . | Other numerical . | −7 . | 5q− . | −5 . | abn(3q) . | Complex . | |
| Total | 1065 | 43 | 23 | 12 | 109 | 48 | 26 | 24 | 15 | 11 | 295 | 277 | 87 | 80 | 55 | 27 | 146 |
| Alone | 23 | 6 | 7 | 41 | 5 | 5 | 9 | 1 | 4 | 70 | 51 | 13 | 6 | 1 | 2 | — | |
| With the following: | |||||||||||||||||
| t(15;17) | 43 | — | 0 | 0 | 5 | 1 | 0 | 2 | 0 | 0 | 11 | 3* | 0 | 0 | 0 | 0 | 0* |
| t(8;21) | 23 | — | 0 | 1 | 1 | 0 | 2 | 0 | 1 | 0† | 13* | 1 | 0 | 0 | 0 | 0 | |
| inv(16) | 12 | — | 1 | 2 | 0 | 0 | 1 | 0 | 2 | 3 | 0 | 0 | 0 | 1 | 1 | ||
| +8 | 109 | — | 7 | 10† | 4 | 8† | 1 | 42* | 48† | 11 | 16* | 8 | 6 | 33† | |||
| 7q− | 48 | — | 2 | 2 | 1 | 0 | 35† | 33† | 3 | 11† | 8* | 4 | 30† | ||||
| +21 | 26 | — | 1 | 5† | 0 | 16† | 17† | 2 | 3 | 3 | 1 | 13† | |||||
| 9q− | 24 | — | 0 | 0 | 8 | 9 | 3 | 2 | 1 | 2 | 6 | ||||||
| +22 | 15 | — | 0 | 11† | 11† | 0 | 4 | 3 | 1 | 10† | |||||||
| 11q23 | 11 | — | 6 | 5 | 2 | 0 | 2 | 0 | 3 | ||||||||
| Other structural | 295 | — | 156† | 57† | 62† | 47† | 19† | 129† | |||||||||
| Other numerical | 277 | — | 53† | 56† | 50† | 15* | 140† | ||||||||||
| −7 | 87 | — | 22† | 27† | 12† | 50† | |||||||||||
| 5q− | 80 | — | 2 | 10† | 50† | ||||||||||||
| −5 | 55 | — | 3 | 50† | |||||||||||||
| abn(3q) | 27 | — | 15† | ||||||||||||||
| Complex | 146 | — | |||||||||||||||
| . | Cytogenetic aberration . | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total . | t(15;17) . | t(8;21) . | inv(16) . | +8 . | 7q− . | +21 . | 9q− . | +22 . | 11q23 . | Other structural . | Other numerical . | −7 . | 5q− . | −5 . | abn(3q) . | Complex . | |
| Total | 1065 | 43 | 23 | 12 | 109 | 48 | 26 | 24 | 15 | 11 | 295 | 277 | 87 | 80 | 55 | 27 | 146 |
| Alone | 23 | 6 | 7 | 41 | 5 | 5 | 9 | 1 | 4 | 70 | 51 | 13 | 6 | 1 | 2 | — | |
| With the following: | |||||||||||||||||
| t(15;17) | 43 | — | 0 | 0 | 5 | 1 | 0 | 2 | 0 | 0 | 11 | 3* | 0 | 0 | 0 | 0 | 0* |
| t(8;21) | 23 | — | 0 | 1 | 1 | 0 | 2 | 0 | 1 | 0† | 13* | 1 | 0 | 0 | 0 | 0 | |
| inv(16) | 12 | — | 1 | 2 | 0 | 0 | 1 | 0 | 2 | 3 | 0 | 0 | 0 | 1 | 1 | ||
| +8 | 109 | — | 7 | 10† | 4 | 8† | 1 | 42* | 48† | 11 | 16* | 8 | 6 | 33† | |||
| 7q− | 48 | — | 2 | 2 | 1 | 0 | 35† | 33† | 3 | 11† | 8* | 4 | 30† | ||||
| +21 | 26 | — | 1 | 5† | 0 | 16† | 17† | 2 | 3 | 3 | 1 | 13† | |||||
| 9q− | 24 | — | 0 | 0 | 8 | 9 | 3 | 2 | 1 | 2 | 6 | ||||||
| +22 | 15 | — | 0 | 11† | 11† | 0 | 4 | 3 | 1 | 10† | |||||||
| 11q23 | 11 | — | 6 | 5 | 2 | 0 | 2 | 0 | 3 | ||||||||
| Other structural | 295 | — | 156† | 57† | 62† | 47† | 19† | 129† | |||||||||
| Other numerical | 277 | — | 53† | 56† | 50† | 15* | 140† | ||||||||||
| −7 | 87 | — | 22† | 27† | 12† | 50† | |||||||||||
| 5q− | 80 | — | 2 | 10† | 50† | ||||||||||||
| −5 | 55 | — | 3 | 50† | |||||||||||||
| abn(3q) | 27 | — | 15† | ||||||||||||||
| Complex | 146 | — | |||||||||||||||
P values are for Fisher exact test comparing abnormality A vs not-abnormality A with abnormality B vs not-abnormality B.
abn indicates abnormal.
P < .01.
P < .001.
Prognostic significance of hierarchical cytogenetic classification in older adults with AML
We then sought to determine the prognostic significance of individual abnormalities within the parameters of the original AML10 hierarchical classification (Table 3). Among the favorable risk abnormalities, superior CR rates were observed for cases with t(8;21) where 87% achieved remission. The CR rate among APL cases with the t(15;17) was lower, owing to a high incidence of ID, which was nonsignificantly more common among patients randomized to the inferior short arm of the MRC ATRA trial, whereby patients received ATRA for 5 days prior to induction chemotherapy; 67% of patients receiving extended ATRA therapy simultaneously with induction chemotherapy, but only 42% of patients receiving short-term ATRA therapy, achieved CR. RR for cases with the t(15;17) was 26% at 5 years, which was significantly lower than for all other cytogenetic abnormalities, and was comparable to that observed in younger adults treated with ATRA and chemotherapy.11 This led to a superior OS of 38% at 5 years, which was comparable to cases with t(8;21) (Table 3). A high CR rate was also observed in cases with inv(16); OS was lower than for the other 2 favorable risk abnormalities, although reliability was limited by small sample size.
Complete remission rates, survival, and relapse risk by cytogenetic abnormalities in Medical Research Council trial AML11
| Abnormality . | Total no. . | CR and reason for failure . | Relapse risk at 5 years, % (SE) . | Overall survival at 5 years, % (SE) . | ||
|---|---|---|---|---|---|---|
| CR rate, % . | Induction deaths, % . | Resistant disease, % . | ||||
| Overall | 1065 | 55 | 18 | 26 | 79 (1.8) | 13 (1.1) |
| Favorable | ||||||
| t(15;17) | 43 | 63 | 33 | 5 | 26 (9.1)3-153 | 38 (8.2)3-155 |
| t(8;21) | 23 | 87 | 03-155 | 13 | 84 (12.4) | 35 (9.9) |
| inv(16) | 12 | 75 | 17 | 8 | 89 (10.5) | 17 (10.8) |
| Intermediate | ||||||
| No abnormality | 507 | 63 | 20 | 17 | 78 (2.5) | 15 (1.7) |
| Sole +8 | 41 | 51 | 17 | 32 | 95 (4.9) | 5 (3.4) |
| 11q233-150 | 7 | 86 | 0 | 14 | 100 (0.0) | 0 (0.0) |
| Other intermediate3-151 | 221 | 54 | 16 | 303-153 | 84 (3.6) | 11 (2.2) |
| Adverse | ||||||
| Noncomplex adverse3-152 | 66 | 453-155 | 14 | 413-153 | 81 (8.1) | 7 (3.9) |
| Complex (with no favorable) | 145 | 263-153 | 19 | 563-153 | 91 (5.1)3-153 | 2 (1.2)3-153 |
| Abnormality . | Total no. . | CR and reason for failure . | Relapse risk at 5 years, % (SE) . | Overall survival at 5 years, % (SE) . | ||
|---|---|---|---|---|---|---|
| CR rate, % . | Induction deaths, % . | Resistant disease, % . | ||||
| Overall | 1065 | 55 | 18 | 26 | 79 (1.8) | 13 (1.1) |
| Favorable | ||||||
| t(15;17) | 43 | 63 | 33 | 5 | 26 (9.1)3-153 | 38 (8.2)3-155 |
| t(8;21) | 23 | 87 | 03-155 | 13 | 84 (12.4) | 35 (9.9) |
| inv(16) | 12 | 75 | 17 | 8 | 89 (10.5) | 17 (10.8) |
| Intermediate | ||||||
| No abnormality | 507 | 63 | 20 | 17 | 78 (2.5) | 15 (1.7) |
| Sole +8 | 41 | 51 | 17 | 32 | 95 (4.9) | 5 (3.4) |
| 11q233-150 | 7 | 86 | 0 | 14 | 100 (0.0) | 0 (0.0) |
| Other intermediate3-151 | 221 | 54 | 16 | 303-153 | 84 (3.6) | 11 (2.2) |
| Adverse | ||||||
| Noncomplex adverse3-152 | 66 | 453-155 | 14 | 413-153 | 81 (8.1) | 7 (3.9) |
| Complex (with no favorable) | 145 | 263-153 | 19 | 563-153 | 91 (5.1)3-153 | 2 (1.2)3-153 |
Percentages may not add to 100 because of rounding. Pvalues are for Fisher exact test (CR and reasons for failure) or log-rank test (relapse risk and overall survival) comparing each abnormality with normal karyotype (ie, no abnormality). MostP values remain at a similar level of significance when adjusted for age, type of leukemia (de novo or secondary), and WBC at presentation, except for the following: induction death: t(15;17) vs normal, P = .08 unadjusted, P = .007 adjusted; overall survival: t(15;17) vs normal, P = .005 unadjusted, P = .1 adjusted.
CR indicates complete remission.
Excludes patients with 11q23 in a favorable karyotype (n = 1) and in an adverse karyotype (n = 3).
Includes all patients not otherwise classified as favorable or adverse risk.
Includes patients with −7, del(5q), −5, and abnormal (3q) alone and in combination with up to 3 other cytogenetic abnormalities.
P < .001.
P < .01.
In comparison with the favorable cytogenetic group, cases classified within the intermediate cytogenetic risk category had a poorer outcome: overall CR rates were lower (60%) owing to a higher incidence of RD (21%), and RR was higher (81% at 5 years), leading to an inferior OS of 13% at 5 years. Overall, cases classified within the adverse cytogenetic risk group were found to have an even poorer prognosis, with only 32% achieving CR owing to high rates of RD (51%); furthermore, the small proportion of patients achieving CR almost invariably relapsed (RR, 86%), leading to an OS of only 4% at 5 years. Further analysis revealed that the subgroup with complex karyotype had the poorest outcome, while the prognosis of cases with noncomplex adverse abnormalities was more comparable to the group with cytogenetic changes classed as intermediate risk (Table 3, Figure1). The CR rate of 45% for cases with noncomplex adverse abnormalities was significantly better than the CR rate of 26% in cases with complex karyotype (P = .006), but not significantly different from the 54% CR rate observed in the other intermediate cytogenetic risk group (P = .2).
Therefore, the hierarchical cytogenetic classification that was devised for children and younger adults entered into the MRC AML10 trial, which predicted CR rate, RR, and OS, was also found to be highly predictive of outcome in older adults entered into the MRC AML11 trial. However, in contrast to younger patients in whom outcomes of cases with complex karyotype and noncomplex adverse abnormalities were found to be comparable,8 the outcome of older adults with noncomplex karyotypes, including chromosomal abnormalities of 3q, 5, or 7, was comparable to that of patients with abnormalities associated with intermediate risk and normal karyotype (Figure 1). This observation led to development of a revised hierarchical cytogenetic classification that was more predictive in this age group (Table4, Figure2). Differences in outcome between particular cytogenetic abnormalities remained significant when adjusted for age, type of leukemia (de novo or secondary), and presenting WBC. In accordance with the analysis of cases entered into AML10,8 the presence of additional cytogenetic abnormalities had no significant influence on prognosis in AML11 (favorable alone: CR, 68%; RR and OS at 5 years, 51% and 31%, respectively; favorable plus other aberrations: CR, 76%; RR, 57%; OS, 37%). Among patients in the intermediate cytogenetic risk category, the relatively small subgroup remaining in first CR at 5 years could not be distinguished from those who relapsed or died in remission before 5 years on the basis of pretreatment characteristics (age, sex, cytogenetic abnormality, type of leukemia, presenting WBC, and platelet count) or subsequent treatment randomizations. In the subgroup of intermediate risk patients with a cytogenetic abnormality, increasing complexity of karyotype was associated with a decrease in OS owing to poorer CR rates, which reflected increasing rates of RD (for 1, 2, 3, and 4 unrelated abnormalities: CR, 58%, 54%, 24%, 44%,P = .005; RD, 28%, 29%, 58%, 40%, P = .004; and OS, 9%, 13%, 6%, 8%, P = .01, respectively). Within cytogenetic risk groups, patients with residual normal metaphases tended to have a better prognosis than those in whom solely abnormal metaphases were detected; however, this effect was not strong enough to merit any further modification of the cytogenetic classification system.
Complete remission rates, reasons for failure, relapse risk, and survival in Medical Research Council trial AML11 by the new hierarchical cytogenetic risk group
| Cytogenetic risk group4-150 . | Total no. . | CR and reason for failure . | Relapse risk at 5 years, % (SE) . | Overall survival . | |||
|---|---|---|---|---|---|---|---|
| CR rate, % . | Induction deaths, % . | Resistant disease, % . | At 5 years, % (SE) . | Median . | |||
| Favorable | 78 | 724-151 | 21 | 84-151 | 56 (7.5)4-151 | 34 (5.7)4-151 | 559 days4-151 |
| Intermediate | 842 | 59 | 18 | 23 | 81 (1.9) | 13 (1.2) | 276 days |
| Adverse | 145 | 26 | 19 | 56 | 91 (5.1) | 2 (1.2) | 113 days |
| Cytogenetic risk group4-150 . | Total no. . | CR and reason for failure . | Relapse risk at 5 years, % (SE) . | Overall survival . | |||
|---|---|---|---|---|---|---|---|
| CR rate, % . | Induction deaths, % . | Resistant disease, % . | At 5 years, % (SE) . | Median . | |||
| Favorable | 78 | 724-151 | 21 | 84-151 | 56 (7.5)4-151 | 34 (5.7)4-151 | 559 days4-151 |
| Intermediate | 842 | 59 | 18 | 23 | 81 (1.9) | 13 (1.2) | 276 days |
| Adverse | 145 | 26 | 19 | 56 | 91 (5.1) | 2 (1.2) | 113 days |
P values are for Mantel-Haenszel (CR and reasons for failure) or log-rank (relapse risk and overall survival) test for trend. All P values remain at a similar level of significance when adjusted for age, type of leukemia (de novo or secondary), and white blood count at presentation.
CR indicates complete remission.
Favorable: t(15;17), t(8;21), or inv(16) whether alone or in conjunction with other abnormalities. Intermediate: normal karyotype, all other noncomplex abnormalities. Adverse: complex karyotype (5 or more unrelated abnormalities), excluding cases with t(15;17), t(8;21), and inv(16).
P < .001.
Influence of age on epidemiology and prognostic implications of cytogenetic aberrations in AML
To examine potential reasons for the poorer prognosis of AML in older adults, we considered the frequency of particular cytogenetic abnormalities according to age of patients entered into the MRC AML10 and AML11 trials, representing 2677 cases (Table5). Favorable risk abnormalities were detected less frequently in older adults than in younger patients; the presence of a complex karyotype, −5, and del(5q) were significantly more common in the older age group. A number of other cytogenetic aberrations demonstrated significant variation in frequency according to age. These included changes involving 11q23, t(6;9)(p23;q34), +8, and +21 and nonrecurring structural abnormalities that were more common in younger individuals; normal karyotype was more common in older adults. A significantly greater proportion of cases of secondary AML was found to have a complex karyotype; −7, del(5q),−5, or 3q abnormalities; or +8 and other numerical and structural abnormalities. Secondary leukemias were confirmed to be more common in older patients (P < .001), while t(15;17) was more common in de novo AML. Table 5 also highlights the rarity of some primary recurring cytogenetic abnormalities associated with AML such as t(9;22)(q34;q11) and t(6;9); all remaining recurrent abnormalities that were not listed were extremely uncommon, with an individual frequency of fewer than 10, eg, t(8;16)(p11;p13) (n = 6).
Percentage of cytogenetic abnormalities in Medical Research Council trials AML10 and AML11
| Abnormality . | All patients (n = 2677), no. (%) . | de novo (n = 2310), % . | Secondary (n = 367), % . | 0-14 years (n = 340), % . | 15-34 years (n = 461), % . | 35-54 years (n = 783), % . | 55+ years (n = 1093), % . |
|---|---|---|---|---|---|---|---|
| None | 1187 (44) | 45 | 38 | 27 | 38 | 51 | 48 |
| +8 | 257 (10) | 9 | 135-150 | 14 | 10 | 7 | 105-151 |
| Complex | 241 (9) | 8 | 155-151 | 6 | 6 | 6 | 135-150 |
| t(15;17) | 241 (9) | 10 | 25-151 | 9 | 19 | 10 | 45-151 |
| −7 | 148 (6) | 4 | 125-151 | 4 | 3 | 4 | 8 |
| t(8;21) | 145 (5) | 6 | 2 | 12 | 6 | 7 | 25-151 |
| del(5q) | 108 (4) | 3 | 85-150 | 1 | 1 | 2 | 75-151 |
| −5 | 81 (3) | 3 | 55-150 | 1 | 2 | 2 | 55-151 |
| del(7q) | 80 (3) | 3 | 5 | 2 | 2 | 2 | 4 |
| 11q23 | 72 (3) | 3 | 1 | 8 | 5 | 2 | 15-151 |
| +21 | 71 (3) | 3 | 4 | 6 | 3 | 1 | 25-151 |
| inv(16) | 69 (3) | 3 | 1 | 5 | 6 | 2 | 15-151 |
| abn(3q) | 67 (3) | 2 | 45-150 | 2 | 3 | 2 | 3 |
| del(9q) | 49 (2) | 2 | 2 | 4 | 1 | 1 | 2 |
| +22 | 37 (1) | 1 | 2 | 1 | 2 | 1 | 1 |
| t(9;22) | 18 (1) | 1 | 1 | 1 | 0 | 1 | <1 |
| t(6;9) | 15 (1) | 1 | 0 | 1 | 1 | 1 | <15-151 |
| Other structural | 634 (24) | 22 | 375-151 | 29 | 18 | 20 | 275-150 |
| Other numerical | 560 (21) | 20 | 265-150 | 23 | 18 | 15 | 26 |
| Abnormality . | All patients (n = 2677), no. (%) . | de novo (n = 2310), % . | Secondary (n = 367), % . | 0-14 years (n = 340), % . | 15-34 years (n = 461), % . | 35-54 years (n = 783), % . | 55+ years (n = 1093), % . |
|---|---|---|---|---|---|---|---|
| None | 1187 (44) | 45 | 38 | 27 | 38 | 51 | 48 |
| +8 | 257 (10) | 9 | 135-150 | 14 | 10 | 7 | 105-151 |
| Complex | 241 (9) | 8 | 155-151 | 6 | 6 | 6 | 135-150 |
| t(15;17) | 241 (9) | 10 | 25-151 | 9 | 19 | 10 | 45-151 |
| −7 | 148 (6) | 4 | 125-151 | 4 | 3 | 4 | 8 |
| t(8;21) | 145 (5) | 6 | 2 | 12 | 6 | 7 | 25-151 |
| del(5q) | 108 (4) | 3 | 85-150 | 1 | 1 | 2 | 75-151 |
| −5 | 81 (3) | 3 | 55-150 | 1 | 2 | 2 | 55-151 |
| del(7q) | 80 (3) | 3 | 5 | 2 | 2 | 2 | 4 |
| 11q23 | 72 (3) | 3 | 1 | 8 | 5 | 2 | 15-151 |
| +21 | 71 (3) | 3 | 4 | 6 | 3 | 1 | 25-151 |
| inv(16) | 69 (3) | 3 | 1 | 5 | 6 | 2 | 15-151 |
| abn(3q) | 67 (3) | 2 | 45-150 | 2 | 3 | 2 | 3 |
| del(9q) | 49 (2) | 2 | 2 | 4 | 1 | 1 | 2 |
| +22 | 37 (1) | 1 | 2 | 1 | 2 | 1 | 1 |
| t(9;22) | 18 (1) | 1 | 1 | 1 | 0 | 1 | <1 |
| t(6;9) | 15 (1) | 1 | 0 | 1 | 1 | 1 | <15-151 |
| Other structural | 634 (24) | 22 | 375-151 | 29 | 18 | 20 | 275-150 |
| Other numerical | 560 (21) | 20 | 265-150 | 23 | 18 | 15 | 26 |
Percentages indicate the percentage of the column total. Percentages do not add to 100 because patients with more than one abnormality are counted more than once. P values are for Mantel-Haenszel test for trend in age (grouped) and for Fisher exact test in type of AML comparing each abnormality with normal karyotype (ie, no abnormality). P values for type of leukemia (de novo vs secondary) remain at a similar level of significance when adjusted for age group. Most P values for age group remain at a similar level of significance when adjusted for type of leukemia (de novo vs secondary) except for del(9q):P = .08 unadjusted, P < .001 adjusted; other numerical, P = .2 unadjusted, P< .001 adjusted. Secondary leukemias are more common in older patients (Mantel-Haenszel chi-square for trend, P < .001).
P < .01.
P < .001.
The poorer OS of older patients with favorable cytogenetic abnormalities in comparison with younger individuals entered into the AML10 trial could not be accounted for by the frequency, nature, or number of secondary aberrations (Table 2,8 and data not shown). We also sought to investigate the influence of the relative proportions of hierarchical risk groups on outcome of AML arising in different age cohorts (Figure 3). There was a significant increase in the relative proportion of normal and complex karyotypes with advancing age, while favorable karyotypes were infrequent in older patients, being most commonly observed in cases of AML presenting in children and younger adults. The deleterious effect of advancing age at the time of diagnosis on subsequent outcome is highlighted by data presented in Figure 3; indeed, age remained a highly significant prognostic factor (P < .001) even when hierarchical cytogenetic risk group was taken into account. Hierarchical cytogenetic risk group also retained its prognostic value (P < .001) when age was taken into account. This shows that differences in the distribution of cytogenetic risk groups, shown in Figure 3, influence but do not explain the deterioration in outcome with increasing age.
The DAT 3 + 10 and ADE 10 + 3 + 5 regimens employed as the first induction course in the AML11 trial2 were common to the AML10 protocol for younger patients.12 We then considered the influence of karyotype on response to the initial course of chemotherapy among cohorts of patients younger than 55 or 55 years of age or older derived from the MRC trials randomized to DAT or ADE (Table 6). In both age groups, cases with favorable karyotype were characterized by higher CR rates associated with lower levels of RD. In contrast, cases with complex karyotype were typified by low CR rates owing to high levels of RD (Table 6), while intermediate CR and RD rates were observed in the group with other intermediate changes and normal karyotype. This confirmed that the hierarchical cytogenetic risk groupings are highly predictive of outcome for AML in all age groups (Table 6).
Impact of cytogenetic risk group on outcome to identical combination chemotherapy regimens within age group
| Hierarchical cytogenetic risk group by age . | No. patients randomized to DAT or ADE . | Status after course 1 . | ||
|---|---|---|---|---|
| CR, % . | Induction death, % . | Resistant disease, % . | ||
| Younger than 55 years | ||||
| Overall | 1500 | 59 | 8 | 33 |
| Favorable | 354 | 646-150 | 9 | 276-150 |
| No abnormality | 646 | 63 | 6 | 31 |
| Other intermediate | 345 | 57 | 7 | 36 |
| Noncomplex adverse | 71 | 31 | 15 | 54 |
| Complex | 84 | 43 | 12 | 45 |
| Older than 55 years | ||||
| Overall | 568 | 43 | 20 | 37 |
| Favorable | 39 | 566-150 | 18 | 266-150 |
| No abnormality | 270 | 49 | 23 | 29 |
| Other intermediate | 152 | 39 | 16 | 44 |
| Noncomplex adverse | 35 | 37 | 11 | 51 |
| Complex | 72 | 26 | 22 | 51 |
| Hierarchical cytogenetic risk group by age . | No. patients randomized to DAT or ADE . | Status after course 1 . | ||
|---|---|---|---|---|
| CR, % . | Induction death, % . | Resistant disease, % . | ||
| Younger than 55 years | ||||
| Overall | 1500 | 59 | 8 | 33 |
| Favorable | 354 | 646-150 | 9 | 276-150 |
| No abnormality | 646 | 63 | 6 | 31 |
| Other intermediate | 345 | 57 | 7 | 36 |
| Noncomplex adverse | 71 | 31 | 15 | 54 |
| Complex | 84 | 43 | 12 | 45 |
| Older than 55 years | ||||
| Overall | 568 | 43 | 20 | 37 |
| Favorable | 39 | 566-150 | 18 | 266-150 |
| No abnormality | 270 | 49 | 23 | 29 |
| Other intermediate | 152 | 39 | 16 | 44 |
| Noncomplex adverse | 35 | 37 | 11 | 51 |
| Complex | 72 | 26 | 22 | 51 |
Mantel-Haenszel test for trend was performed, P values for effect of hierarchical cytogenetic risk group on status after course 1 within age group. DAT indicates daunorubicin, ara-C, 6-thioguanine; ADE, ara-C, daunorubicin, etoposide; CR, complete remission.
P < .001.
Discussion
For many years, it has been appreciated that age is a key prognostic factor in AML, with a steady deterioration in outcome with increasing years (reviewed by Harousseau14). However, in order to improve the therapeutic approach for older patients with this disease it is essential to establish the basis of this phenomenon. This is likely to be a consequence of 3 key variables: the characteristics of the patient population, the intensity of the chemotherapy protocol employed, and the nature of the leukemia itself. However, the extent to which each of these factors contributes to the unfavorable prognosis of AML in older patients has been somewhat unclear. This information is critical to predict whether innovations in treatment are likely to be of any clinical benefit. A potential advantage of studies such as the MRC trials is that they provide some insights into these issues.
To some extent, an inferior outcome in older adults is to be expected, owing to the increased likelihood of coexistent end-organ damage leading to a poorer tolerance of combination chemotherapy regimens, associated with higher rates of ID. While it is accepted that older individuals entered into leukemia trials represent a highly selected group and that the number of cases considered was relatively small, AML11 is consistent with the concept that the biological behavior of cases of AML with particular cytogenetic abnormalities in older patients is comparable to that of cases with the same aberrations arising in younger individuals.
MRC AML11 also shows that intensive induction therapy is feasible in some older individuals.2 Concern about toxicity has in some instances prompted the use of less intensive protocols, including curtailed or indeed no consolidation therapy. This is likely to be a key reason why the majority of older patients with AML who successfully achieve CR nevertheless ultimately die from leukemic relapse. This is supported from analyses of patients with t(8;21) and inv(16) derived from AML11. While the CR rate for this group was not significantly different from that of younger patients with these abnormalities using identical or comparable combination chemotherapy,8 RR was significantly higher in patients treated in AML11 (83% in AML11 vs 33% in AML10 at 5 years, P < .0001); however, age could also be a contributory factor to this phenomenon. Intensive induction therapy may therefore be beneficial in these cytogenetically defined subgroups of AML, and it is possible that further improvements may be feasible with enhanced consolidation therapy. However, the options available to this age group are relatively limited, owing to the risks of excessive toxicity. In selected patients, more intensive chemotherapy, autologous bone marrow transplantation (BMT)/peripheral blood stem cell transplantation,15 or nonmyeloablative allogeneic BMT16 could be investigated. However, such strategies are likely to prove impractical for the vast majority of patients in this age group and confer no overall benefit in terms of OS or quality of life. Therefore, there is considerable interest in alternative approaches that are more specific to the underlying cytogenetically/molecularly defined abnormality and may provide an inherently less toxic form of consolidation therapy. APL associated with the t(15;17), leading to formation of the PML-RARα oncoprotein, has provided the first such example, being sensitive to ATRA and arsenic trioxide (reviewed by Grimwade17). As well as conferring a survival advantage when combined with induction chemotherapy, ATRA has been shown to reduce the risk of relapse when used as maintenance therapy, particularly in combination with 6-mercaptopurine and methotrexate.18 It is possible that the ABL-specific tyrosine kinase inhibitor STI57119 could have a role in infrequent cases of t(9;22)/BCR-ABL–associated AML. Furthermore, a number of studies have implicated deregulation of histone acetylation in the development of some subtypes of AML, including APL and those associated with t(8;21)/AML1-ETO (reviewed by Redner et al20). This suggests a further target for future therapies, which has already been exploited in a previously resistant case of APL with the use of sodium phenylbutyrate.21 It is presently unclear whether the latter approach is likely to be fruitful in the majority of cases of AML arising in the elderly, in which the molecular events underlying leukemogenesis remain to be characterized; nevertheless, the generally poor prognosis supports the reliable evaluation of novel therapeutic approaches in large phase III trials in this group.
While increased susceptibility to treatment toxicity undoubtedly contributes to adverse outcome in older adults (Table 6), failure to achieve CR in this age group is more commonly the result of intrinsic resistance of leukemic blasts to chemotherapy (Table 3). This observation has led to considerable interest as to whether AML arising in older adults represents a distinct disease entity from that developing in younger individuals, which could be the key reason underlying the adverse prognosis. In this regard, secondary leukemias are more common in older adults (Table 1 and Grimwade et al8), arising following an antecedent hematologic disorder, particularly myelodysplasia, and have been associated with a poor prognosis.22 AML arising in older adults is also associated with higher rates of P-gp expression, correlated with a poor response to induction chemotherapy.5,23 Furthermore, a number of studies have highlighted the detection of adverse karyotypic features, notably abnormalities of chromosomes 5 and 7, in elderly AML, changes that had previously been associated with secondary AML.4,5,24,25 This has led to the suggestion that the disease arising in the elderly is more akin to secondary AML and that in patients lacking a documented history of antecedent hematologic disorder or previous chemotherapy/radiotherapy, it could reflect an increased genetic susceptibility to environmental mutagens (reviewed by Willman3). This is supported by a recent study that has identified cases of AML arising in elderly patients with a mutator phenotype, associated with lack of expression of MSH2 and mutations of p53,26 reminiscent of therapy-related AML in which a high incidence of p53 mutations and microsatellite instability have been reported previously.27 However, it is clear from the present study that the spectrum of cytogenetic abnormalities detected among older patients with AML is identical to that detected in younger patients, although the relative frequency of particular aberrations varies considerably with age (Table 5). Overall, favorable risk abnormalities were relatively uncommon in the elderly, whereas normal and complex karyotypes were more common (Figure 3). However, above 55 years of age no further increase in the proportion of cases with adverse cytogenetic features was observed (Table 1), suggesting that the presumed poorer prognosis of very elderly patients who are rarely entered into clinical trials will not be accounted for by the karyotypic profile of this group. The variation in the relative size of the hierarchical risk groups with age is clearly a major influence, but does not account for the adverse outcome of older adults with AML. This study also shows that high CR rates are attainable in older patients with favorable risk cytogenetic abnormalities, associated with low rates of induction failure due to RD. This would suggest that expression of proteins conferring a drug resistance phenotype is unlikely to be prevalent in this group. This is supported by a number of studies undertaken in younger adults with AML with favorable cytogenetics, though these studies have largely focused on AML with the t(15;17).23,28,29 In the present study, the CR rate for older patients with t(15;17) was inferior to that of younger individuals (63% AML11, 87% AML10,P < .001), owing partly to a higher ID rate among patients randomized to receive only 5 days of ATRA prior to induction chemotherapy; overall, the RR for older APL patients was only 26% at 5 years in AML11, which is comparable to younger patients with this disease (37% in AML10). The European APL93 study has recently reported excellent results in older patients with low presenting WBC induced with extended ATRA and combination chemotherapy (CR, 90%; RR, 7%; and OS, 69% at 2 years).18 It appears highly plausible that AML associated with favorable karyotypes arising in older patients is biologically similar to leukemias with the same abnormalities occurring in younger individuals and demands specific treatment approaches. Furthermore, poor CR rates, which reflected comparably high levels of RD, were observed among older and younger patients with adverse cytogenetic features. Previous work undertaken in elderly AML suggests that this is likely to reflect the high rates of P-gp expression in this group.5 In a more recent study involving a younger cohort of patients with newly diagnosed AML, Leith et al23 also observed a trend toward a higher incidence of P-gp expression in cases with adverse cytogenetics in comparison with those with more favorable karyotypes. Furthermore, Legrand et al30 have reported that combined activity of multidrug-resistance proteins P-gp and MRP1 is more predictive of adverse outcome than the activity of either protein alone, and that coexpression was most closely correlated with the presence of adverse karyotypic features. This is important, since chemoresistance mediated by both of these mechanisms is potentially amenable to modulation, which could lead to significant improvements in clinical outcome. Further evidence supporting the notion that karyotype analysis identifies subgroups of AML that are biologically similar irrespective of the age of the patient has been provided by recent studies reporting a close correlation between cytogenetic subgroup and bax/bcl2 ratio,31 immunophenotypic profile,32 and the behavior of primary leukemic blasts, both in vitro, in terms of proliferative activity, semisolid colony growth, and response to granulocyte-macrophage colony-stimulating factor,33,34 and in vivo, influencing engraftment characteristics in nonobese diabetic/severe combined immunodeficient mice.35
To date, cytogenetic classification systems used to predict outcome in AML have been somewhat inconsistent. This is likely to reflect influences of sample size and interstudy and intrastudy variation in treatment approach, as well as differences in the age of the study population. Recent studies have highlighted the importance of validation of proposed cytogenetic classification systems in independent data sets.10,36 The original MRC AML10 hierarchical cytogenetic classification has subsequently been prospectively validated in children and younger adults entered into the MRC AML12 trial,36 and in the present study, it was also found to be of prognostic value in an older cohort of patients that was the subject of the MRC AML11 trial. However, in the latter group, a minor modification entailing assignment of noncomplex adverse abnormalities to the intermediate risk category was found to provide a more predictive and clinically relevant system. The classification system clearly identified the group with favorable cytogenetics, who appeared most likely to benefit from intensive treatment in terms of CR and OS rates, with a third of patients alive at 5 years. Furthermore, the modified system distinguished those with complex karyotype who had an extremely poor prognosis; in accordance with a recent report from the German AML Cooperative Study Group,37 these patients are only very rarely cured with intensive therapy and might therefore be best treated according to a more palliative approach.
While cytogenetic analysis provides a framework that can clearly distinguish groups of patients with differing responses to treatment and likelihoods of relapse, it lacks the ability to distinguish cohorts of patients with differing prognoses within cytogenetic risk groups. This may be enhanced in the future with discovery of novel rearrangements associated with AML, such as Flt3mutations,38-40 and analysis of larger cohorts of patients, permitting more confident assignment of prognostic significance to rare recurrent cytogenetic abnormalities. Previous work has suggested that determination of P-gp status could be helpful in distinguishing subgroups of patients with differing prognoses within cytogenetic risk groups, which could prove of value to the design of future stratified treatment approaches.5 Studies considering the impact of a multidrug-resistant phenotype on prognosis, in conjunction with the present study considering the outcome of older and younger patients with identical cytogenetic abnormalities treated with comparable induction therapy, afford the opportunity to take a more reasoned approach to treatment of AML in older adults.
We thank all the clinicians participating in the MRC trials, as detailed in the accompanying paper,2 and the cytogeneticists involved in performing the karyotype analyses.
The following cytogenetics laboratories participated in the study. Ireland: Department of Genetics, Trinity College, Dublin and University College Hospital, Galway. England: Hospital cytogenetic laboratories participating included Birmingham Maternity and Heartlands; Southmead, Bristol; Addenbrooke's, Cambridge; St Richard's, Chichester; Queen's, Croydon; Northwick Park, Harrow; Ipswich; St James', Leeds; Liverpool Women's; Christie, Manchester; Middlesbrough General; Norfolk and Norwich; Nottingham City; Hammersmith, King's College, Royal Free, St Mary's, and University College, London; Churchill, Oxford; Salisbury District and Royal Marsden, Sutton, in addition to Geoffrey Schofield Laboratories, British Nuclear Fuels, Cumbria; Leicester Royal Infirmary; Department of Human Genetics, University of Newcastle, and Centre for Human Genetics, Sheffield. New Zealand: The following centers participated: Auckland, Christchurch, Dunedin, Palmerston, Waikato, and Wellington. Northern Ireland: Department Medical Genetics, Belfast City Hospital. Scotland: Medical Genetics Laboratories, Aberdeen; Ninewells Hospital Medical School, Dundee; MRC Human Genetics Unit, Western General Hospital, Edinburgh; Duncan Guthrie Institute of Medical Genetics, Yorkhill, Glasgow; Royal Northern Infirmary, Inverness. Wales: Department of Haematology and Institute of Medical Genetics, University Hospital of Wales, Cardiff.
Supported by the Leukaemia Research Fund of Great Britain (D.G.); the MRC trials database is supported by the Kay Kendall Leukaemia Fund.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
A. H. Goldstone, North London Cancer Network, 6th Floor, Rosenheim Wing, University College Hospital, 25 Grafton Way, London WC1E 6DB, United Kingdom; e-mail: anthony.goldstone@uclh.org.