Abstract
Using murine models, primitive hematopoietic cells capable of repopulation have been shown to reside in various anatomic locations, including the aortic gonad mesonephros, fetal liver, and bone marrow. These sites are thought to be seeded by stem cells migrating through fetal circulation and would serve as ideal targets for in utero cellular therapy. In humans, however, it is unknown whether similar stem cells exist. Here, we identify circulating hematopoeitic cells present during human in utero development that are capable of multilineage repopulation in immunodeficient NOD/SCID (nonobese diabetic/severe combined immunodeficient) mice. Using limiting dilution analysis, the frequency of these fetal stem cells was found to be 1 in 3.2 × 105, illustrating a 3- and 22-fold enrichment compared with full-term human cord blood and circulating adult mobilized–peripheral blood, respectively. Comparison of in vivo differentiation and proliferative capacity demonstrated that circulating fetal stem cells are intrinsically distinct from hematopoietic stem cells found later in human development and those derived from the fetal liver or fetal bone marrow compartment at equivalent gestation. Taken together, these studies demonstrate the existence of unique circulating stem cells in early human embryonic development that provide a novel and previously unexplored source of pluripotent stem cell targets for cellular and gene-based fetal therapies.
Introduction
The hematopoietic system comprises cells derived from rare multipotent stem cells that are tightly controlled to regulate differentiation and proliferation into mature blood cells.1,2 Differentiation into functionally mature cells generally depends on the passage of stem cells through a stage of committed progenitor cells.2,3 However, these progenitors retain limited proliferative capacity and must therefore be sustained by rarer primitive stem cell populations throughout the life span of the animal.1 Based on their reconstituting properties, it is these hematopoietic cells that are generally targeted for clinical gene therapy to combat congenital disorders for permanent correction.4 The application of stem cell transplantation and gene therapy would be best served if therapy could be implemented in earlier life and thus inhibit the course and severity of disease progression. This implies that in utero intervention would be the most beneficial. In utero therapy has only recently been considered as a potential method of disease management because of the technological advancements in performing early gestational cellular transplants using high-resolution ultrasound.5 Although the basis of in utero hematopoietic stem cell therapy is well assembled, preliminary trials have failed, reflecting our current lack of understanding of human embryonic blood formation.6
The anatomic orchestration and compartmentalization of blood stem cells during human fetal development is not well defined. The current model obtained from studies using the mouse suggests that the para-aortic region and the fetal liver (FL) are the first sites in which reconstituting hematopoietic stem cells can be detected in the embryo and that migrating stem cells seed the developing bone marrow (BM).7,8 Although a variety of primitive blood cell types can be detected using in vivo assays in the mouse, such as colony-forming units–spleen (CFU-S), radioprotective repopulating cells, and long-term reconstituting cells, assays for similar stem cell populations in humans are limited.2,3 Dick and colleagues have pioneered the development of a quantitative assay for primitive human hematopoietic cells capable of multilineage repopulation using immunodeficient NOD/SCID (nonobese diabetic/severe combined immunodeficient) mice as transplant recipients.9 These human repopulating cells are operationally defined as SCID-repopulating cells (SRCs) and have been shown to be more primitive and functionally distinct from cells detectable using human in vitro clonogenic assays.10 11 Using this human-mouse xenotransplantation system, we have now identified human hematopoietic stem cells capable of repopulating NOD/SCID mice in the circulation of the human fetus during early embryonic development. The frequency, proliferative, and differentiative capacity of human fetal blood (FB) stem cells differed substantially from repopulating cells derived from full-term cord blood (CB) and primitive cells derived from human FL or fetal BM (FBM). These studies demonstrate the isolation of human fetal stem cells with unique intrinsic properties from repopulating cells found later in human development that may provide a novel and clinically advantageous target population for in utero therapies.
Materials and methods
Human cells
Samples of FB, FBM, and FL from 12- to 18-week abortus and full-term umbilical CB were obtained in conjunction with local ethical and biohazard authorities of the University of Western Ontario and London Health Sciences Centre. FB was procured in a manner that precluded the potential contamination of maternal blood and was similar to diagnostic methods of FB sampling.12 Whole blood and FBM was diluted (1:3) in α-minimal essential medium (Gibco BRL, Grand Island, NY) or phosphate-buffered saline (PBS), and mononuclear cells (MNCs) were collected by centrifugation on Ficoll-Paque (Pharmacia) as shown previously.13
Cell purification
Subsets of CD34−CD38−Lin−, CD34+CD38−Lin−, and CD34+CD38+Lin− cells were isolated and analyzed using standard protocols.13 14 Briefly, MNCs were first enriched for lineage-depleted (Lin−) cells by negative selection using a cocktail of lineage antibodies and the StemSep device similar to that described by the manufacturers (Stem Cell Technologies, Vancouver, Canada). These cell fractions were then stained with antihuman CD34-allophycocyanin (APC) and antihuman CD38-phycoerythrin (PE) (Becton Dickinson Immunocytometry Systems, San Jose, CA) and then analyzed and sorted on a FACSVantage SE (Becton Dickinson). Sorting gates used are indicated in Figure3A. Data acquisition and analyses were performed using Cell Quest software (Becton Dickinson).
Clonogenic progenitor assays
Human clonogenic progenitor assays were performed by plating various cell populations at concentrations ranging from 1 × 102 to upward of 1 × 103 cells into a methlycellulose cocktail, Methocult H4434 (Stem Cell Technologies), containing 50-ng/mL recombinant human (rh) stem cell factor, 10-ng/mL rh granulocyte-macrophage colony-stimulating factor, 10-ng/mL rh interleukin-3, and 3-U/mL rh erythropoietin, and incubating at 37°C with 5% CO2 in a humidified atmosphere. Differential colony counts were scored by morphologic characteristics using an inverted microscope after 10 to 14 days.
Transplantation of human cells into NOD/SCID mice
Cells were transplanted by tail vein injection into sublethally irradiated NOD/LtSz-scid/scid (NOD/SCID) mice (350 cGy137Cs) according to standard protocols.13 Mice were killed 6 to 8 weeks after transplantation, and BM cells were collected from murine femurs, tibiae, and iliac crests for analysis, along with organ tissue that included kidney, liver, lung, spleen, and skeletal muscle.
Analysis of human cell engraftment
High molecular weight DNA was isolated from the BM cells and organ tissue of transplanted mice, digested with EcoRI restriction enzyme, and the percentage of human cells determined by probing Southern blots with a human chromosome 17–specific α-satellite probe as previously described.13 The level of human cell engraftment was quantified by analysis of Southern blots using a phosphorimager (Molecular Dynamics) and Image-Quant software by comparing the characteristic 2.7-kilobase band with human-to-mouse DNA mixture controls (limit of detection, 0.05% human DNA) that provided a linear signal response. In addition, the BM of transplanted mice was analyzed by staining with the human panleukocyte marker CD45 to detect the presence of human hematopoietic cells by flow cytometric analysis using a FACSCalibur and Cell Quest software as described below.
Flow cytometric analysis of murine BM
To prepare cells for flow cytometry, contaminating red cells were lysed with a 0.8% ammonium chloride solution, and the remaining cells were washed in PBS containing 5% fetal calf serum (FCS). Cells were resuspended in 0.25 mL of PBS plus 5% FCS, washed, and then incubated with monoclonal antibodies at a concentration of 5 μg/mL for 30 minutes at 4°C. The antibody combinations used are indicated in Figure 4 (CD45 was conjugated to PerCP; CD20 and CD33 were conjugated to fluorescein isothiocyanate [FITC]; CD38, CD15, and CD19 were conjugated to PE; and CD34 was conjugated to APC). Cells were then washed 3 times in PBS plus 5% FCS and analyzed on a FACSCalibur or FACSVantage SE. For each mouse analyzed, cells were also stained with mouse immunoglobulin G1 conjugated to FITC, PE, PerCP, and APC as isotype controls.
Statistical analysis
The data were analyzed by the unpaired, 2-tailed Studentt test assuming a Gaussian distribution (parametric test) using the Graphpad Prism package Version 2.0 (Graphpad, San Diego, CA). For limiting dilution analysis, a transplanted mouse was scored positive for human engraftment if human DNA was detectable by Southern blot analysis and CD45+ cells were detected in the BM of transplanted mice. Data from limiting dilution experiments were pooled and analyzed by applying Poisson statistics to the single-hit model.15 The frequency of SRCs in fetal circulation was calculated with the maximum likelihood estimator as shown previously.11 15
Results
Phenotypic comparison of human fetal and cord blood MNCs
Maturation of fetal erythropoiesis involving globin switching has been well described in the developing human.16 17 However, other cellular components during early stages of blood formation are not well characterized, including cell types that constitute the fetal circulation. MNCs from FB were collected at 12 to 18 weeks of human gestation and compared with the composition of MNCs from full-term human CB. A representative sample is shown in Figure1, with the average percentage of specific cell populations shown for 4 independent samples of both FB and CB. Proportions of committed myeloid cells that express CD33 or myelogranulocytic cells expressing CD15, and the maturation of the B-cell lymphoid compartment expressing CD19 and CD20, were similar in both FB and CB (Figure 1A-D). However, fetal circulation contained fewer T cells expressing either CD4 or CD8 than CB, with early CD4+CD8+ T cells being extremely rare in FB (0.1%) versus CB (4.5%) (Figure 1E,F), illustrating a deficiency in an important immunologic subset associated with fetal development. Although the primitive subfractions of cells expressing the stem cell–associated marker CD34 were similar in both FB and CB (Figure1G,H), the immature subset of CD34+CD38− cells was present at a significantly higher frequency in FB than CB (0.3% vs 0.09%, P < .001). Based on this analysis, it seems that the composition of human FB and full-term CB are dissimilar in both T-cell maturation and primitive cell populations, suggesting that the in vivo processes regulating differentiation of pluripotent stem cells differs between these 2 stages of human ontogeny.
Comparison of mature and primitive cell subsets constituting human fetal and CB-MNCs.
Representative analysis of cell surface markers using multiparameter flow cytometry of FB- and CB-MNCs. Composition of myeloid cells was indicated by CD33 and CD15 (A,B), B-lymphoid cells by CD19 and CD20 (C,D), T-lymphoid cells by CD4 and CD8 (E,F), and primitive subsets by CD34 and CD38 (G,H) cell surface expression. Average percentage for each subpopulation was calculated with SEM and indicated in each dot plot based on at least 4 independent FB and CB samples. Quadrant settings for each phenotype were based on isotype controls.
Comparison of mature and primitive cell subsets constituting human fetal and CB-MNCs.
Representative analysis of cell surface markers using multiparameter flow cytometry of FB- and CB-MNCs. Composition of myeloid cells was indicated by CD33 and CD15 (A,B), B-lymphoid cells by CD19 and CD20 (C,D), T-lymphoid cells by CD4 and CD8 (E,F), and primitive subsets by CD34 and CD38 (G,H) cell surface expression. Average percentage for each subpopulation was calculated with SEM and indicated in each dot plot based on at least 4 independent FB and CB samples. Quadrant settings for each phenotype were based on isotype controls.
Human fetal blood contains cells capable of repopulating NOD/SCID mice
The recent development of the SRC assay has provided an in vivo functional measurement for the investigation of primitive human hematopoietic cells.18 Most of these studies have characterized human SRCs derived from adult BM and CB based on the ability of primitive cells at these stages of ontogeny to repopulate the BM of sublethally irradiated immunodeficient NOD/SCID mice after intravenous transplantation.19 20 To determine whether hematopoietic stem cells were present in the fetal circulation, fetal MNCs were transplanted into NOD/SCID mice. DNA from BM and other tissues were extracted from mice 8 weeks posttransplantation and analyzed for human sequence by Southern blot analysis. Two representative mice transplanted with 4 × 105 cells isolated from an individual FB sample are shown in Figure2A. The BM from recipient mouse FB12.8 contained human cells and was verified by flow cytometry using a human-specific panleukocyte marker CD45, demonstrating that human FB contains primitive cells capable of repopulation. We have termed these fetal blood repopulating cells FB-SRCs. In addition, human cells were detected in various tissues of transplanted mice, indicating that FB-SRCs are capable of engrafting sites other than the murine BM that included liver, lung, spleen, kidney and, surprisingly, skeletal muscle (Figure 2A). Based on this result and the fact that FB-SRCs represent a previously uncharacterized cell population with unknown homing and retention properties, we analyzed the tissue of transplanted mice in which we were unable to detect human cells in the BM compartment. A representative mouse, FB12.9, that tested negative for human cells in the BM, was confirmed not to contain detectable human cells in any other tissues (Figure 2A), demonstrating that BM analysis of mice transplanted with FB is representative of FB-SRC activity and that repopulating activity does not preferentially occur in other tissue sites. In all NOD/SCID recipients analyzed (n = 6), detection of human cells in organ sites was always associated with human chimerism in the BM compartment; reciprocally, BM chimerism was concomitant with organ engraftment (data not shown). Taken together, these data demonstrate that FB stem cells exist in human embryonic circulation at early stages of in utero development and that the engraftment of FB repopulating cells can occur in multiple tissue environments, including the murine BM.
Analysis of human engraftment and frequency of primitive human FB cells capable of repopulating NOD/SCID mice.
(A) Representative Southern blot analysis of liver, lung, muscle, spleen, kidney, and BM of 2 individual NOD/SCID mice transplanted with 4 × 105 human FB-MNCs. DNA was extracted from murine BM 8 weeks posttransplantation and hybridized with a human chromosome 17–specific α-satellite probe. Human cells were detectable in the BM of mouse FB12.8 by flow cytometric analysis using the human-specific panleukocyte marker CD45, whereas no human CD45+ cells were detectable in the BM of mouse FB12.9. (B) Representative Southern blot analysis of 9 individual NOD/SCID mice transplanted with a single FB sample using 8 × 105 (lanes 1-3), 4 × 105(lanes 4-6), and 2 × 105 FB-MNCs (lanes 7-10). (C) Summary of the level of human cell engraftment in the BM of mice transplanted with human FB-MNCs from 6 independent samples. NOD/SCID mice (n = 27) were transplanted with various doses of FB cells (range, 1 × 105 to 1 × 106). Each symbol represents a single NOD/SCID recipient. Mice were considered to be engrafted if a band was detectable by Southern blotting of the extracted DNA followed by hybridization with a human-specific probe (limit of detection of 0.05% human). Poisson statistics were applied to the single-hit model, and the frequency of SRCs, calculated using the maximum likelihood estimator, was 1 SRC in 3.2 × 105FB-MNCs (95% confidence interval, 1 in 1.8 × 105 to 1 in 7.2 × 105).
Analysis of human engraftment and frequency of primitive human FB cells capable of repopulating NOD/SCID mice.
(A) Representative Southern blot analysis of liver, lung, muscle, spleen, kidney, and BM of 2 individual NOD/SCID mice transplanted with 4 × 105 human FB-MNCs. DNA was extracted from murine BM 8 weeks posttransplantation and hybridized with a human chromosome 17–specific α-satellite probe. Human cells were detectable in the BM of mouse FB12.8 by flow cytometric analysis using the human-specific panleukocyte marker CD45, whereas no human CD45+ cells were detectable in the BM of mouse FB12.9. (B) Representative Southern blot analysis of 9 individual NOD/SCID mice transplanted with a single FB sample using 8 × 105 (lanes 1-3), 4 × 105(lanes 4-6), and 2 × 105 FB-MNCs (lanes 7-10). (C) Summary of the level of human cell engraftment in the BM of mice transplanted with human FB-MNCs from 6 independent samples. NOD/SCID mice (n = 27) were transplanted with various doses of FB cells (range, 1 × 105 to 1 × 106). Each symbol represents a single NOD/SCID recipient. Mice were considered to be engrafted if a band was detectable by Southern blotting of the extracted DNA followed by hybridization with a human-specific probe (limit of detection of 0.05% human). Poisson statistics were applied to the single-hit model, and the frequency of SRCs, calculated using the maximum likelihood estimator, was 1 SRC in 3.2 × 105FB-MNCs (95% confidence interval, 1 in 1.8 × 105 to 1 in 7.2 × 105).
Previous studies have attempted to provide evidence for the theoretical enrichment of mammalian fetal hematopoietic stem cells compared with that found later in development by using mouse fetal stem cells in murine transplantation systems. However, similar analysis cannot be applied to human fetal development because of ethical concerns and the lack of a similar assay. Taking advantage of the fact that the NOD/SCID model can provide a surrogate in vivo assay for fetal stem cells (Figure 2A) and is capable of quantitative analysis for the absolute number of human stem cells from a given source of human hematopoietic tissue,11 we performed limiting dilution analysis to determine the number of repopulating cells in fetal circulation. Figure2B shows the results of a representative experiment using one FB sample where cells were transplanted into groups of mice at various doses as indicated. The repopulation results of NOD/SCID mice (n = 27) transplanted with MNCs from 6 independent human FB samples at dose ranges indicated are summarized in Figure 2C. Human engraftment was detected with as few as 1 × 105 transplanted cells in some experiments (Figure 2C). The number of human repopulating cells in fetal circulation was analyzed by Poisson statistics and the frequency of FB-SRCs determined by the maximum likelihood estimator. We determined that 1 FB-SRC was present in 3.2 × 105 MNCs (95% confidence interval, 1 in 1.8 × 105 to 1 in 7.2 × 105), representing a 3- and 22-fold enrichment of human stem cells compared with CB and adult mobilized–peripheral blood (M-PB), respectively.21
To determine whether the volume of whole blood collected from a single fetus would be adequate for reconstituting function in autologous transplantation, we calculated the number of FB-SRCs theoretically required for a fetal recipient weighing less than 0.5 kg22-24 at 12 to 18 weeks of gestation (Table1). This was extrapolated from the only clinical data available in humans to predict successful reconstitution that has correlated the number of MNCs that must be transplanted per kilogram of the recipient's body weight in adult patients receiving autologous M-PB that ensure hematologic recovery and long-term engraftment.25-27 Based on a total of 22 independent FB collections of 3.5 mL (a volume that does not cause hemodynamic compromise28), we estimate that a total of 34.7 FB-SRCs (9.93 FB-SRCs/mL × 3.5 mL; Table 1) can be safely collected without harm to fetal development. Because our estimations indicate that 1.425 FB-SRCs are required to reconstitute an average fetal recipient (Table1), our data suggest that the number of repopulating cells obtained per collection should provide sufficient reconstitution to the fetal recipient. Circulating fetal cells represent a highly enriched source of human blood stem cells that can be obtained without harm to the fetus, in contrast to FL tissue collection, and may therefore have superior utility for autologous transplantation therapy in utero.
Preclinical estimation of the number of hematopoietic stem cells required for in utero reconstitution using FB as a novel source of transplantable hematopoietic tissue
| . | Number of MNCs per mL (106) . | Number of FB-SRCs per mL . | Total number of FB-SRCs in 3.5 mL of whole blood collection . | Total number of FB-SRCs required for reconstitution . |
|---|---|---|---|---|
| Whole FB (collection at 12-18 wk) | 3.1 ± 0.6 | 9.93* | 9.93 FB-SRC/mL × 3.5 mL = 34.7 FB-SRC per collection | Based on avg wt of fetal recipient and placenta of 0.5 kg 0.5 kg × 2.85† = 1.425 FB-SRC |
| . | Number of MNCs per mL (106) . | Number of FB-SRCs per mL . | Total number of FB-SRCs in 3.5 mL of whole blood collection . | Total number of FB-SRCs required for reconstitution . |
|---|---|---|---|---|
| Whole FB (collection at 12-18 wk) | 3.1 ± 0.6 | 9.93* | 9.93 FB-SRC/mL × 3.5 mL = 34.7 FB-SRC per collection | Based on avg wt of fetal recipient and placenta of 0.5 kg 0.5 kg × 2.85† = 1.425 FB-SRC |
The total number of human FB repopulating cells (FB-SRCs) was estimated based on whole FB collection of 3.5 mL at 12 to 18 weeks' gestation (n = 22 independent samples). This volume was previously shown not to induce hemodynamic damage to the fetus. Based on this estimation, we suggest that an excess number of FB stem cells can be collected from the fetus in utero for autologous transplantation.
The total number of FB-SRCs was calculated by dividing the average number of FB-MNCs per milliliter of whole blood by the frequency of FB-SRCs per 106 MNCs (3.1 × 106/0.32 × 106).
Using the clinically accepted number of cells required for long-term reconstitution in the adult as 2 × 106CD34+ per kilogram of the recipient's body weight and a 10% enrichment of CD34+ cells upon mobilization among peripheral blood MNCs, it was estimated that 20 × 106MNCs/kg are required for engraftment. Because the frequency of adult M-PB SRCs is 1 in 7 × 106 MNCs, it was estimated that 2.85 SRCs/kg are required for reconstitution (20 × 106 MNCs/kg divided by 7.0 × 106 MNCs for 1 SRC) and was used to estimate the number of FB-SRCs needed for engraftment in the fetal recipient.
Phenotypic characterization of primitive human FB cells
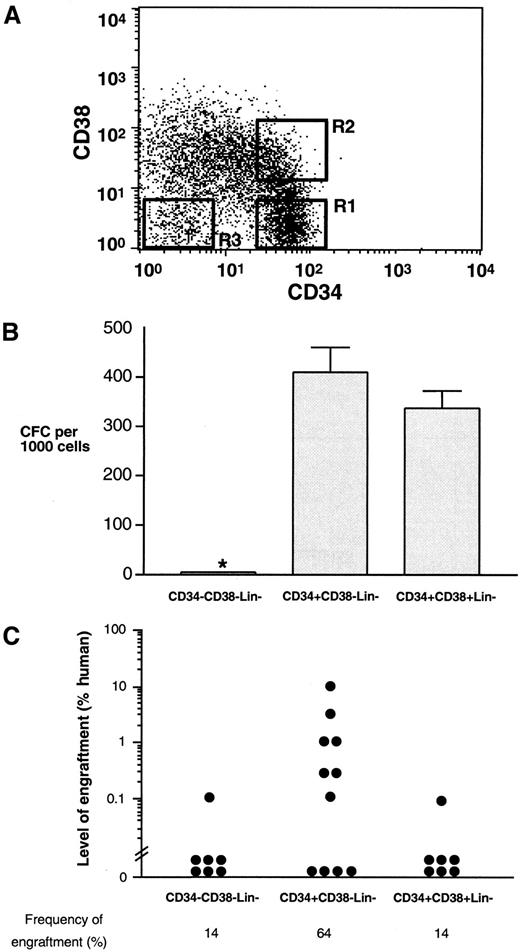
To characterize primitive circulating cells in the human fetus, subpopulations were purified and assayed for multiple progenitor and pluripotent repopulating function. Previous studies using multiparameter flow sorting for the isolation of subfractions of phenotypically primitive lineage-depleted CB and adult BM cells (Lin−) has indicated that stem cell activity is found in the CD34+CD38−Lin− or CD34−CD38−Lin−subfractions.11 14 Lineage-committed FB-MNCs were eliminated to allow for the isolation of a fraction of uncommitted FB Lin− cells. Lin− cells were stained with fluorochrome-conjugated antibodies against CD34 and CD38 and analyzed by flow cytometry. A representative analysis for the expression of CD34 and CD38 in FB Lin− cells is shown in Figure 3A. Populations of CD34+CD38−Lin−(gated R1), CD34+CD38+Lin− (gated R2), and CD34−CD38−Lin− (gated R3) cells were isolated by high-speed flow cytometric sorting. Reanalysis of sorted populations demonstrated the purity to be more than 98% (data not shown). Clonogenic assays were performed on purified subfractions to detect hematopoietic progenitors (colony-forming cells [CFCs]) in vitro or were transplanted into NOD/SCID mice by intravenous injection for the detection of repopulating cells in vivo.
Phenotypic characterization of primitive human FB subsets capable of in vitro progenitor and repopulating capacity in NOD/SCID mice.
(A) Representative analysis of cell surface CD34 and CD38 by multiparameter flow cytometry of human FB cells depleted for cells expressing lineage commitment markers (Lin−). Subpopulations of CD34+CD38−Lin−, CD34+CD38+Lin−, and CD34−CD38−Lin− were gated R1, R2, and R3, respectively, and isolated for functional analysis using in vitro and in vivo assays. (B) CFC capacity was assessed in subfractions indicated and represented as the number of CFCs per 1000 purified cells. Values are the mean and SEM of determinations from up to 5 separate FB samples. (C) Summary of the level of human cell engraftment in the BM of NOD/SCID mice transplanted (n = 25) with purified cell fractions from 6 independent FB samples. Each symbol represents a single NOD/SCID recipient.
Phenotypic characterization of primitive human FB subsets capable of in vitro progenitor and repopulating capacity in NOD/SCID mice.
(A) Representative analysis of cell surface CD34 and CD38 by multiparameter flow cytometry of human FB cells depleted for cells expressing lineage commitment markers (Lin−). Subpopulations of CD34+CD38−Lin−, CD34+CD38+Lin−, and CD34−CD38−Lin− were gated R1, R2, and R3, respectively, and isolated for functional analysis using in vitro and in vivo assays. (B) CFC capacity was assessed in subfractions indicated and represented as the number of CFCs per 1000 purified cells. Values are the mean and SEM of determinations from up to 5 separate FB samples. (C) Summary of the level of human cell engraftment in the BM of NOD/SCID mice transplanted (n = 25) with purified cell fractions from 6 independent FB samples. Each symbol represents a single NOD/SCID recipient.
The number of CFCs per 1000 cells from purified subsets of FB cells is shown in Figure 3B. Similar to previous studies using CB and BM, fetal CD34−CD38−Lin− cells contained few primitive clonogenic progenitors,14,29 whereas both CD34+CD38−Lin− and CD34+CD38+Lin− fractions were found to be highly clonogenic in vitro.13 This indicates that factors capable of supporting the survival, growth, and differentiation of primitive human CB and adult BM progenitors are similar to the extrinsic growth factor requirements of human fetal progenitors detected in vitro. However, in contrast to CD34+Lin− CB and adult BM,13there was no significant difference in the frequency of progenitors between CD38− or CD38+ subsets derived from FB (Figure 3B). Table 2 compares the types of CFUs that constitute the progenitor compartment of all subfractions isolated from human FB and CB. From these data, subpopulations of FB and CB demonstrated similar lineage commitment profiles, indicating that the progenitors from both FB and CB have equivalent differentiative capacity.
Percentage of clonogenic progenitors within subpopulations of CD34−CD38−Lin−, CD34+CD38−Lin−, and CD34+CD38+Lin− cells from human FB and CB
| Subpopulation phenotype . | CFU-M, % . | CFU-G, % . | CFU-GM, % . | BFU-E, % . | CFU-GEMM, % . |
|---|---|---|---|---|---|
| Fetal blood | |||||
| CD34−CD38−Lin− | 0.0 ± 0.0 | 27.0 ± 27.0 | 9.5 ± 9.5 | 63.5 ± 36.5 | 0.0 ± 0.0 |
| CD34+CD38−Lin− | 17.3 ± 4.3 | 41.8 ± 14.8 | 3.5 ± 0.5 | 36.7 ± 18.2 | 0.65 ± 0.65 |
| CD34+CD38+Lin− | 9.4 ± 2.3 | 26.7 ± 1.6 | 4.3 ± 1.0 | 59.6 ± 2.9 | 0.0 ± 0.0 |
| Cord blood | |||||
| CD34−CD38−Lin− | 4.3 ± 1.7 | 25.0 ± 7.5 | 0.5 ± 0.5 | 65.0 ± 9.5 | 5.2 ± 0.9 |
| CD34+CD38−Lin− | 9.2 ± 2.7 | 54.9 ± 9.9 | 2.6 ± 1.3 | 30.3 ± 7.4 | 2.9 ± 1.5 |
| CD34+CD38+Lin− | 2.5 ± 0.0 | 51.8 ± 0.0 | 0.0 ± 0.0 | 45.5 ± 0.0 | 0.0 ± 0.0 |
| Subpopulation phenotype . | CFU-M, % . | CFU-G, % . | CFU-GM, % . | BFU-E, % . | CFU-GEMM, % . |
|---|---|---|---|---|---|
| Fetal blood | |||||
| CD34−CD38−Lin− | 0.0 ± 0.0 | 27.0 ± 27.0 | 9.5 ± 9.5 | 63.5 ± 36.5 | 0.0 ± 0.0 |
| CD34+CD38−Lin− | 17.3 ± 4.3 | 41.8 ± 14.8 | 3.5 ± 0.5 | 36.7 ± 18.2 | 0.65 ± 0.65 |
| CD34+CD38+Lin− | 9.4 ± 2.3 | 26.7 ± 1.6 | 4.3 ± 1.0 | 59.6 ± 2.9 | 0.0 ± 0.0 |
| Cord blood | |||||
| CD34−CD38−Lin− | 4.3 ± 1.7 | 25.0 ± 7.5 | 0.5 ± 0.5 | 65.0 ± 9.5 | 5.2 ± 0.9 |
| CD34+CD38−Lin− | 9.2 ± 2.7 | 54.9 ± 9.9 | 2.6 ± 1.3 | 30.3 ± 7.4 | 2.9 ± 1.5 |
| CD34+CD38+Lin− | 2.5 ± 0.0 | 51.8 ± 0.0 | 0.0 ± 0.0 | 45.5 ± 0.0 | 0.0 ± 0.0 |
Progenitor content was measured by enumerating the colony-forming units (CFU) from equal numbers of phenotypically distinct subpopulations isolated from lineage-depleted samples of human fetal blood and cord blood. The number of each type of CFU was determined from plating conditions outlined in “Materials and methods” and identified according to standard protocols. CFU-M indicates CFU-macrophage; CFU-G, CFU-granulocyte; CFU-GM, CFU-granulocyte, macrophage; BFU-E, burst-forming unit-erythroid; and CFU-GEMM, CFU-granulocyte, erythroid, macrophage, megakaryocyte. The percentage of each colony type is calculated as the mean ± SEM.
Figure 3C summarizes the level of human chimerism in the BM of NOD/SCID mice transplanted with highly purified subpopulations of cells within fetal circulation. The repopulating activity and level of human engraftment from FB was found to be enriched in the CD34+CD38−Lin− subfraction (Figure 3C), similar to CD34+ SRCs from CB and adult BM.11,30 As few as 250 CD34+CD38−Lin− cells isolated from the fetal circulation were capable of engrafting NOD/SCID mice. The low number of purified cells required to detect engraftment suggests that purified fractions of FB are more highly enriched for SRC activity and is consistent with the higher frequency of SRCs found within unfractionated FB-MNCs determined by limiting dilution analysis (Figure 2B,C). Similar to previous studies using human CB or adult BM,14 repopulating cells were rarely detected in mice transplanted with the CD34−CD38−Lin− fraction, and only 1 mouse of 7 transplanted with individual FB samples was found to be engrafted. Therefore, although CD34− FB-SRCs can be detected, the frequency of detecting these CD34−stem cells is rare. Similar to our previous studies using CB CD34− SRCs, CD34− FB-SRCs may require prestimulation in ex vivo culture prior to transplantation into NOD/SCID mice before enhanced repopulation activity can be detected.14 Our data demonstrate that primitive repopulating cells can be purified from fetal circulation in humans, suggesting that purging strategies to remove infected or transformed mature cells can potentially be used during in utero autologous transplantation without loss of reconstituting stem cells.
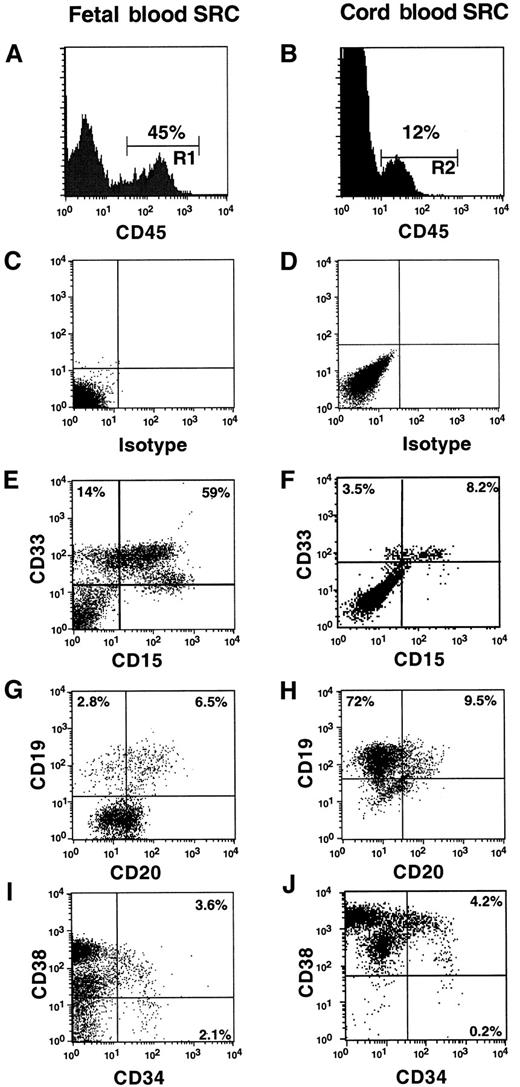
Intrinsic differences in the differentiation and proliferation of human FB and CB repopulating cells
The differentiative and proliferative capacity of FB-SRCs was compared with that of CB repopulating cells by flow cytometric analysis of human cell chimerism in the BM of engrafted NOD/SCID mice. For illustration, a representative analysis of the BM of 2 NOD/SCID mice transplanted with 2 FB-SRCs (6 × 105 FB-MNCs) and 2 CB-SRCs (20 × 105 CB-MNCs) is shown in Figure4. The human-specific panleukocyte marker CD45 was used to analyze human cells in the BM of engrafted animals and, accordingly, human CD45+ cells (indicated by R1 and R2 gates in Figure4A,B) were used for subsequent multilineage analyses.20The isotype control shown in Figure 4C,D is specific for each mouse analysis and was used to establish quadrants for subsequent multilineage analysis. The BM of these mice contained 45% and 12% CD45+ human cells from FB and CB transplants, respectively, even though each mouse was transplanted with an approximately equivalent number of repopulating cells (Figure 4A,B). The proportion of myeloid cells, demonstrated by CD15+ and CD33+ fractions, was greater in mice transplanted with FB-SRCs (59%) than in mice engrafted with CB-SRCs (8.2%) (Figure4E,F). Consistent with the multilineage engraftment, lymphoid cells were present in the BM of mice transplanted with either FB or CB cells as shown by staining for CD19 and CD20 human B cells (Figure 4G,H). CB-SRCs proliferate and differentiate to produce a large proportion of human B cells as shown previously (Figure 4H),11 30while FB-SRCs demonstrated a lower degree of B-lymphoid commitment (Figure 4G) (72% vs 2.8%, respectively). In addition to the production of mature cells in engrafted mice, a small proportion of CD34+ cells were detected, along with CD34+CD38− cells (Figure 4I,J), providing evidence that phenotypically immature cells are produced and maintained from both FB- and CB-SRCs. Similar to the composition of cells constituting de novo isolated FB (Figure 1), FB-SRCs exhibited a greater production of phenotypically primitive CD34+CD38− subsets compared with CB-SRCs (2.1% vs 0.2%) in the NOD/SCID mouse. In 2 of 3 samples, serial transplantation of human FB cells isolated from primary recipient mice engrafted with FB-SRCs allowed for repopulating function in secondary recipients, indicating that human FB repopulating cells were present in the primary host (data not shown). Differences in engraftment patterns between FB-SRCs and CB-SRCs were observed irrespective of whether MNCs or highly purified subpopulations were transplanted, indicating that the non–stem cell component did not influence the developmental capacity and repopulating function of the stem cell populations. A summary of the relative proportions of human progeny in NOD/SCID mice from both unfractionated (n = 5) and purified FB (n = 3) and unfractionated (n = 2) and purified full-term CB repopulation (n = 5) is shown in Table 3. In addition, the engraftment patterns of FB-SRCs were compared to ontogenically similar FL- (n = 4) and FBM- (n = 3) derived repopulating cells. Our results indicate the FB-SRCs are not only distinct from CB-SRCs but also from FL-SRCs. Surprisingly, the intrinsic properties of FB-SRCs, as measured by proliferative and differentiative capacity in vivo, is similar to that of FBM-SRCs with the exception of CD34+ subsets, suggesting these circulating cells play a greater role in postnatal hematopoiesis arising from the BM compartment (Table 3). Because these differential engraftment patterns were observed in genetically identical hosts, our data indicate that circulating fetal stem cells possess a distinct developmental program from human stem cells found later in human ontogeny and to those found in the FL compartment at similar ontogenic stages.
Comparison of engraftment composition in the BM of NOD/SCID mice transplanted with human fetal and CB stem cells.
BM from representative engrafted mice transplanted with 6 × 105 (2 FB-SRCs) or 20 × 105 (2 CB-SRCs) MNCs. Murine BM cells were stained with various human-specific monoclonal antibodies and analyzed by flow cytometry. (A,B) Histograms of CD45 (panleukocyte marker) expression indicating that 45% and 12% of the cells present in the murine BM were human from FB- and CB-transplanted animals, respectively. Analysis of lineage markers was done on cells within gate R1 and R2 (CD45+). (C,D) Representative isotype controls for nonspecific immunoglobulin G staining for each mouse. (E,F) Expression of myeloid marker CD33 and mature myeloid marker CD15, (G,H) pan–B-cell markers CD19 and CD20, and (I,J) CD38 and immature hematopoietic marker CD34. Multilineage engraftment shown here was similar to that found in additional mice transplanted with FB- and CB-MNCs and purified subsets of FB and CB CD34+CD38−Lin− cells.
Comparison of engraftment composition in the BM of NOD/SCID mice transplanted with human fetal and CB stem cells.
BM from representative engrafted mice transplanted with 6 × 105 (2 FB-SRCs) or 20 × 105 (2 CB-SRCs) MNCs. Murine BM cells were stained with various human-specific monoclonal antibodies and analyzed by flow cytometry. (A,B) Histograms of CD45 (panleukocyte marker) expression indicating that 45% and 12% of the cells present in the murine BM were human from FB- and CB-transplanted animals, respectively. Analysis of lineage markers was done on cells within gate R1 and R2 (CD45+). (C,D) Representative isotype controls for nonspecific immunoglobulin G staining for each mouse. (E,F) Expression of myeloid marker CD33 and mature myeloid marker CD15, (G,H) pan–B-cell markers CD19 and CD20, and (I,J) CD38 and immature hematopoietic marker CD34. Multilineage engraftment shown here was similar to that found in additional mice transplanted with FB- and CB-MNCs and purified subsets of FB and CB CD34+CD38−Lin− cells.
Composition of human cell chimerism in the BM of engrafted NOD/SCID mice transplanted with FB, FBM, FL, and CB repopulating cells
| Lineage phenotype . | FB-SRC, % . | FBM-SRC, % . | FL-SRC, % . | CB-SRC, % . |
|---|---|---|---|---|
| CD33+CD15+ | 43 ± 13.8* | 31.5 ± 8.2* | 9 ± 2.1 | 11 ± 6.1 |
| CD33+CD15− | 8.1 ± 4.1 | 16.5 ± 8.1 | 12 ± 1.4 | 4.3 ± 3.8 |
| CD19+CD20+ | 5.8 ± 3.9 | 13 ± 3.6 | 8.3 ± 2.6 | 8.9 ± 4.1 |
| CD19+CD20− | 4.8 ± 3.2* | 17 ± 6.8* | 53 ± 20.1 | 74 ± 12.1 |
| CD34+ | 6.8 ± 3.5 | 6.5 ± 3.7 | 7.2 ± 3.3 | 5.6 ± 2.1 |
| CD34+CD38− | 2.4 ± 0.9* | 0.2 ± 0.1 | 0.8 ± 0.4 | 0.2 ± 0.2 |
| Lineage phenotype . | FB-SRC, % . | FBM-SRC, % . | FL-SRC, % . | CB-SRC, % . |
|---|---|---|---|---|
| CD33+CD15+ | 43 ± 13.8* | 31.5 ± 8.2* | 9 ± 2.1 | 11 ± 6.1 |
| CD33+CD15− | 8.1 ± 4.1 | 16.5 ± 8.1 | 12 ± 1.4 | 4.3 ± 3.8 |
| CD19+CD20+ | 5.8 ± 3.9 | 13 ± 3.6 | 8.3 ± 2.6 | 8.9 ± 4.1 |
| CD19+CD20− | 4.8 ± 3.2* | 17 ± 6.8* | 53 ± 20.1 | 74 ± 12.1 |
| CD34+ | 6.8 ± 3.5 | 6.5 ± 3.7 | 7.2 ± 3.3 | 5.6 ± 2.1 |
| CD34+CD38− | 2.4 ± 0.9* | 0.2 ± 0.1 | 0.8 ± 0.4 | 0.2 ± 0.2 |
Unfractionated or purified human FB, FBM, FL, and CB cells were transplanted into NOD/SCID mice, and murine BM was analyzed after 8 weeks. Human CD45+ cells were gated and analyzed for composition of myeloid (CD33 and CD15), B-lymphoid (CD19 and CD20), and primitive human subsets (CD34 and CD38). The percentage of each lineage is calculated as the mean ± SEM of human cells and was compared between mice transplanted with FB-SRC, FBM-SRC, FL-SRC, or CB-SRC. Data were analyzed by the unpaired, two-tailed Student t test assuming a Gaussian distribution (parametric test) and demonstrated differences as indicated (*); P < .001, n = 3-8.
Discussion
Previous attempts to reconstitute the hematopoietic system by transplantation in utero have failed. Because both adult BM and FL have been shown to contain primitive hematopoietic cells, human clinical studies have used these sources for in utero transplantation. Most of these trials resulted in low to undetectable levels of hematopoietic chimerism in the fetal recipient from donor cells, suggesting that the source of primitive cells used was either devoid of stem cells or contained stem cells that lacked the predicted in vivo repopulation capacity.31 For example, adult BM stem cells may be incompatible for reconstituting function in the fetal environment, while allogenic FL stem cell transplants may fail because of the lack of homing or proliferative ability required to seed the recipient fetal BM compartment. Previous transplants using experimental models such as concordant in utero sheep indicated that, although presumptive hematopoietic stem cells from FL and BM are capable of homing to BM sites of recipient fetal animals, these cells provide little to no hematopoietic function in postnatal life.32 This experimental result parallels the human trials for in utero blood reconstitution and suggests that an alternative source of human stem cells should be investigated for in utero cellular therapy.
Knowledge gained from transplantation models using embryonic systems can be used to increase the efficacy and safety of in utero stem cell transplants. In humans, there is therefore a need to evaluate stem cell function from human embyronic sources as a preclinical model using surrogate in vivo assay systems. Our current study provides a novel source of human fetal stem cells, distinct from FL stem cells, as targets for in utero cellular therapy and may provide several advantages for in utero transplantation over sources previously used in clinical trials. Although allogenic FL-derived hematopoietic stem cells fail to sustain hematopoiesis after birth, circulating fetal stem cells may provide an alternative source of reconstituting cells that may circumvent this limitation by allowing for autologous transplantation, because our data suggest that these circulating stem cells are more similar to intrinsic stem cells found in the definitive human FBM (Table 3).
The practicality of in utero stem cell transplantation therapies has been questioned because it is unknown whether sufficient stem cells can be removed and manipulated for gene therapy, ex vivo expansion, or cellular purging and then be reinfused into the developing human fetus. Using our xenotransplantation model, quantitative analysis by limiting dilution in recipient NOD/SCID mice has allowed us to enumerate circulating fetal stem cells and establish a preclinical framework in which to base clinical trials in utero. Our study suggests that a sufficient number of repopulating cells can be harvested from a single collection for autologous transplantation during in utero development.33,34 This is supported by unrelated studies that have required FB in a noninvasive manner as a diagnosis of congential disorders and fetal rhesus D immunotyping.33,34Therefore, these early studies, together with our work here, suggest that the ability to harvest hematopoietic stem cells directly from the circulation provides a practical procedure for the transplantation, expansion, and genetic modification of blood stem cells that eliminates the need for evasive extraction of hematopoietic tissue and the need for allogenic transplantation. This is best illustrated in adults undergoing autologous stem cell transplantation using chemically induced mobilized stem cells from the BM compartment into the peripheral blood. In the case of the human fetus, our data indicate that circulating repopulating cells can be obtained between 12 and 18 weeks of gestation, thus circumventing the need to extract cells and damage sites of active hematopoiesis such as the FL35,36 or the use of drug-induced mobilization.37 Based on our current study, we suggest that circulating fetal hematopoietic stem cells can be procured and autologously reintroduced into the fetal circulation, thereby providing an alternative source of target stem cells for in utero cellular and gene-based therapies.
The mechanisms responsible for regulating human stem cell commitment, differentiation, and proliferation are poorly characterized.38 It has been proposed that self-renewal and commitment decisions of stem cells are regulated by stochastic processes.39,40 The stochastic model states that commitment of stem cells is a result of an internally driven program that is cell-autonomous and assumes that the environment supplies growth factors and protein interactions that are merely permissive in allowing cell fate decisions.39,40 In contrast to the stochastic model, the deterministic model argues that the environment dictates cell fate decisions by external factors. Many of these concepts are based on in vitro study of primitive hematopoietic cells derived from different ontogenic stages of human development.41,42 Primitive progenitors isolated from human FL, CB, and adult BM demonstrate differences in response to similar cytokine treatment using serum-free cultures.41 In these studies, the proliferative capacity and production of immature CD34+ progenitors by FL cells was greater than that of CB and adult BM, suggesting that the turnover rate and differentiative capacity of stem cells decreases during human ontogeny and may be due to intrinsically controlled differences between these purified stem cell populations.43 However, experimental support for intrinsic differences among blood stem cells throughout human development has yet to be demonstrated in vivo.40,44 In recent studies by Holyoake et al and Nicolini et al, analysis of human FL cells was revisited by transplantation in NOD/SCID mice, and these investigators suggest that the FL is enriched for repopulating cells as compared with CB.35 36 Only upon human cell isolation from the recipient NOD/SCID mice could differences be distinguished using progenitor assays in vitro. Similar to our data, these studies found that the composition of human grafts from FL repopulating cells did not differ from CB repopulating function, suggesting that FL-SRCs and CB-SRCs represent intrinsically similar stem cells (Table 3). However, both FL- and CB-SRCs differ in their proliferative and differentiative capacity in vivo compared with the novel circulating FB repopulating stem cells identified here (Table 3). Analysis of the graft composition in recipient immune deficient NOD/SCID mice indicated profound differences in proliferative and differentiative capacity of human fetal stem cells from more developmentally mature stem cell populations. Because distinct reconstitution capacity was observed using genetically identical recipient animals, thereby controlling for extrinsic influences, we suggest these differences reflect unique intrinsic properties of circulating stem cells found at this stage of human development.
In the murine system, failure of mouse embryonic cells derived from hematopoietic sites to repopulate adult lethally irradiated mice has been proposed to be due to developmental distinctions in the requirements of embryonic stem cells.2 45 These experiments suggest that regulators supplied by the adult recipient are not compatible with embryonic source material because of the lack of factors required to support the proliferation and differentiation of transplanted fetal stem cells. This incompatibility creates a barrier in the analysis of blood stem cells during early ontogeny where in vivo transplantation assays used to define stem cells are considered the gold standard. In the human scenario, the NOD/SCID mice and fetal sheep have provided xenotransplantion models to detect human stem cell populations. Our data here illustrate that the NOD/SCID model can be used as an in vivo assay for human repopulating stem cells and is capable of detecting aspects associated with differences in the intrinsic properties of stem cells of fetal origin and fetal stem cell compartmentalization, such as those of the FL. Therefore, transplantation of human fetal cells into NOD/SCID mice provides an in vivo model system to be used for the optimization and design of preclinical protocols required for successful in utero gene therapy, purging strategies, and stem cell expansion that target human stem cells present in fetal circulation.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
References
Author notes
Mickie Bhatia, The John P. Robarts Research Institute, Developmental Stem Cell Biology, 100 Perth Dr, London, Ontario, N6A 5K8; e-mail: mbhatia@rri.on.ca.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal