We analyzed data on 612 patients who had undergone high-dose chemoradiotherapy (HDT) with autologous stem cell rescue for Hodgkin's disease (HD) and non-Hodgkin's lymphoma (NHL) at the City of Hope National Medical Center, to evaluate the incidence of therapy-related myelodysplasia (t-MDS) or therapy-related acute myeloid leukemia (t-AML) and associated risk factors. A retrospective cohort and a nested case-control study design were used to evaluate the role of pretransplant therapeutic exposures and transplant conditioning regimens. Twenty-two patients developed morphologic evidence of t-MDS/t-AML. The estimated cumulative probability of developing morphologic t-MDS/t-AML was 8.6% ± 2.1% at 6 years. Multivariate analysis of the entire cohort revealed stem cell priming with VP-16 (RR = 7.7, P = 0.002) to be independently associated with an increased risk of t-MDS/t-AML. The influence of pretransplant therapy on subsequent t-MDS/t-AML risk was determined by a case-control study. Multivariate analysis revealed an association between pretransplant radiation and the risk of t-MDS/t-AML, but failed to reveal any association with pretransplant chemotherapy or conditioning regimens. However, patients who had been primed with VP-16 for stem cell mobilization were at a 12.3-fold increased risk of developing t-AML with 11q23/21q22 abnormalities (P = 0.006). Patients undergoing HDT with stem cell rescue are at an increased risk of t-MDS/t-AML, especially those receiving priming with VP-16 for peripheral stem cell collection.
High-dose chemoradiotherapy (HDT) with stem cell rescue has become the treatment of choice for patients with Hodgkin's disease (HD) and non-Hodgkin's lymphoma (NHL) who have a suboptimal response to initial therapy or for patients with refractory or relapsed disease. Long-term disease-free survival rates of 40% to 50% are reported in patients treated with this approach.1-10 With improvement in survival following intensive therapy, posttransplant therapy-related myelodysplasia (t-MDS) and secondary therapy-related acute myeloid leukemia (t-AML) are emerging as serious long-term complications.11-18 The cumulative probability of t-MDS/ t-AML reported in the literature has ranged from 4% at 5 years15 to 18% at 6 years.16 Some of the risk factors predicting an increased risk of t-MDS/t-AML following transplant have included older age at transplant,14,17radiation therapy,15,16 and a low platelet count at transplant.16 It is unclear whether t-MDS/t-AML is related to pretransplant chemotherapy and radiotherapy or is the result of transplant conditioning and stem cell priming regimens, or a cumulative effect of all of these exposures.
This investigation analyzed data on 612 patients undergoing HDT with stem cell rescue for HD or NHL to evaluate whether pretransplant therapeutic exposures or transplant conditioning and stem cell priming regimens were associated with an increased risk of t-MDS/t-AML. Patients and methods
Both a retrospective cohort and a nested case-control study design were used to evaluate the role of pretransplant therapeutic exposures, stem cell priming, and transplant conditioning regimens in the development of t-MDS/t-AML.
Cohort analysis
Between 1986 and 1998, 612 patients received HDT with autologous stem cell rescue for HD or NHL. Data were obtained from the bone marrow transplant (BMT) database at the City of Hope, and included the unique patient number (UPN), initial diagnosis, gender, date of birth, date of transplant, source of stem cells (bone marrow [BM], peripheral stem cells [PSC] or bone marrow and peripheral stem cells [BM+PSC]), and CD34+ cell dose. For patients who developed t-MDS/t-AML, the date of diagnosis and morphology were recorded. Slides of BM from all patients with t-MDS/t-AML were reviewed. FAB criteria were used for classification of MDS. Cytogenetic studies on BM or unstimulated blood samples were performed using standard methods followed by G-banding with trypsin-Giemsa. Karyotypes were interpreted using International System for Human Cytogenetic Nomenclature (ISCN), 1995.19Karyotypes were considered normal diploid if no clonal abnormalities were detected in a minimum of 20 metaphases examined and if 2 independent cell-processing methods were used.
Cumulative probabilities of developing t-MDS/t-AML over time were calculated using the Kaplan Meier technique.20 The log rank test was used to compare the various subpopulations. Cox regression techniques were used for calculating relative risk estimates. Variables included in the regression model were primary diagnosis, gender, age at transplant, source of stem cells, stem cell priming, and CD34+ cell dose. Age at transplant (< 40 versus ≥ 40 years) and CD34+ cell dose (≤ 3 × 106/kg versus > 3 × 106/kg) were taken as categorical variables. Because stem cell priming with VP-16 began in 1994 at City of Hope, the risk of developing t-MDS/t-AML was also assessed before and after 1994.
This cohort provided us with a sampling frame from which to select controls for the case-control study.
Case-control analysis
For each of the t-MDS/t-AML cases, multiple controls (1-3) were randomly selected from within the cohort, using the following matching criteria: primary disease, age at transplant (± 2 years) and duration of follow-up (± 1 year). For the cases and controls so identified, the entire medical record (which occasionally consisted of records from more than 1 hospital if portions of treatment were provided elsewhere) was used to abstract clinical information important for assessing the characteristics and treatment of the malignancy before the transplant. The following data were collected: (1) disease characteristics—diagnosis (histology), stage, and primary site; (2) treatment prior to transplant— chemotherapy—dates, protocols/regimens, agents, dose schedules, routes of administration, and cumulative dose for selected agents (anthracyclines, alkylating agents, epipodophyllotoxins, etc); radiation therapy—dates, total dose, field, fractions, dose per fraction, equipment, and a copy of the institutional radiation therapy summary report; surgical and other procedures—a summary of all surgical procedures was completed and attached to a copy of institutional surgical reports; (3) priming regimens for stem cell mobilization; (4) source of stem cells; and (5) conditioning regimens used—radiation, chemotherapy.
Analyses of the case-control study measured the degree of association of antecedent factors (eg, chemotherapy, radiation) with adverse outcome (t-MDS/t-AML) by estimation of odds ratios. Exact confidence limits of the odds ratios were calculated. Test for trend was used when analyzing categorical data ordered by degree of intensity or duration or both. Logistic regression was used to investigate the simultaneous effects of several variables. The variables included in the model were pretransplant exposures to alkylating agents and topoisomerase II inhibitors (quantification described below), source of stem cells, various conditioning regimens, and priming for stem cell collection with high-dose VP-16. We also conducted the case-control analysis after excluding patients who had received VP-16 priming, to explore further the association between pretransplant therapy and t-MDS/t-AML in the non-VP-16 primed group.
Chemotherapy quantification
An attempt was made to quantify an individual's exposure to all alkylating agents and topoisomerase II inhibitors. The following drugs were included in the alkylating agent category: nitrogen mustard, cyclophosphamide, chlorambucil, procarbazine, nitrosureas, triethylenemelamine, thiotepa, and dacarbazine. An alkylating agent dose score (AA score) was calculated for each patient (described by Meadows et al21). A single alkylating agent administered for 6 months was assigned a score of 100; for double alkylating agent therapy given for 6 months, a score of 200 was assigned, etc. Similarly, for assessing the topoisomerase exposure, the following drugs were included: etoposide and anthracyclines. A topoisomerase inhibitor dose score was calculated for each patient as follows: a single topoisomerase inhibitor used for 6 months was assigned a score of 100; for double topoisomerase inhibitor therapy given for 6 months, a score of 200 was assigned, etc. The alkylating agent and topoisomerase inhibitor scores were computed for each patient by summing all such scores corresponding to the patient's treatment course and rounding off to the nearest integer. The score thus was a measure of the amount of alkylating agent and topoisomerase inhibitor received as part of pretransplant therapy. VP-16 used as part of priming or conditioning regimens was not included in the above computed scores, but was analyzed separately.
Results
Cohort study
As of July 1998, 60% of the cohort of 612 patients who had received HDT with stem cell rescue at the City of Hope were alive at time of last contact and had a median follow-up of 3.0 years (range, 0.1-10.6 years). The cohort had accrued 1406 person-years of follow-up from transplant. The median age at transplant for the entire cohort was 39.5 years (range, 6-69 years). Fifty-six percent of the cohort was male (Table 1).
Characteristics of the patient population (cohort study)
| Patient Characteristics . | Total Cohort (n = 612) . | t-MDS/t-AML (n = 22) . | ||
|---|---|---|---|---|
| HD . | NHL . | HD . | NHL . | |
| No. of patients | 218 | 394 | 11 | 11 |
| Age at transplant (y) | ||||
| Median (range) | 32.2 (13-66) | 44.6 (6-69) | 30.2 (19-45) | 46.4 (20-61) |
| <40 y | 165 (76%) | 132 (34%) | 9 (81%) | 3 (27%) |
| ≥40 y | 53 (24%) | 262 (66%) | 2 (19%) | 8 (73%) |
| Follow-up (y) | ||||
| Median (range) | 1.9 (0-10.2) | 1.6 (0-10.6) | — | — |
| Gender | ||||
| Males | 118 (54%) | 228 (58%) | 4 (36%) | 5 (46%) |
| Females | 100 (46%) | 166 (42%) | 7 (64%) | 6 (54%) |
| Source of stem cells | ||||
| BM | 31 (14%) | 30 (7%) | 2 (18%) | 1 (9%) |
| PSC/BM + PSC | 187 (86%) | 364 (93%) | 9 (88%) | 10 (91%) |
| Priming with VP-16 | 22 (10%) | 39 (10%) | 2 (18%) | 1 (9%) |
| Years to t-MDS/t-AML | ||||
| from primary diagnosis | — | — | 3.8 | 3.8 |
| from transplant | — | — | 0.9 | 2.4 |
| Vital status | ||||
| Died | 89 (41%) | 156 (40%) | 6 (55%) | 9 (82%) |
| Patient Characteristics . | Total Cohort (n = 612) . | t-MDS/t-AML (n = 22) . | ||
|---|---|---|---|---|
| HD . | NHL . | HD . | NHL . | |
| No. of patients | 218 | 394 | 11 | 11 |
| Age at transplant (y) | ||||
| Median (range) | 32.2 (13-66) | 44.6 (6-69) | 30.2 (19-45) | 46.4 (20-61) |
| <40 y | 165 (76%) | 132 (34%) | 9 (81%) | 3 (27%) |
| ≥40 y | 53 (24%) | 262 (66%) | 2 (19%) | 8 (73%) |
| Follow-up (y) | ||||
| Median (range) | 1.9 (0-10.2) | 1.6 (0-10.6) | — | — |
| Gender | ||||
| Males | 118 (54%) | 228 (58%) | 4 (36%) | 5 (46%) |
| Females | 100 (46%) | 166 (42%) | 7 (64%) | 6 (54%) |
| Source of stem cells | ||||
| BM | 31 (14%) | 30 (7%) | 2 (18%) | 1 (9%) |
| PSC/BM + PSC | 187 (86%) | 364 (93%) | 9 (88%) | 10 (91%) |
| Priming with VP-16 | 22 (10%) | 39 (10%) | 2 (18%) | 1 (9%) |
| Years to t-MDS/t-AML | ||||
| from primary diagnosis | — | — | 3.8 | 3.8 |
| from transplant | — | — | 0.9 | 2.4 |
| Vital status | ||||
| Died | 89 (41%) | 156 (40%) | 6 (55%) | 9 (82%) |
BM indicates bone marrow; HD, Hodgkin's disease; NHL, non-Hodgkin's lymphoma; PSC, peripheral stem cells; t-MDS/t-AML, morphologic therapy-related myelodysplasia and therapy-related acute myeloid leukemia.
Twenty-two patients developed morphologic evidence of t-MDS/t-AML at a median of 1.9 years from transplant and 3.8 years from diagnosis of the primary disease. Twenty of these patients had karyotypic abnormalities (abnormalities of chromosome 5 or 7 [n = 10], 11q23 or 21q22 abnormalities [n = 6] and other nonspecific abnormalities [n = 4]); 2 patients had normal cytogenetics. None of these 20 patients had karyotypic abnormalities before transplant. Of the 22 patients with morphologic evidence of t-MDS/t-AML, 6 had AML, 11 patients developed refractory anemia, 2 developed refractory anemia with excess blasts, 1 patient had refractory anemia with ringed sideroblasts, and 1 had refractory anemia with excess blasts in transformation. The remaining patient had trilineage dysplasia, associated with clonal karyotypic abnormalities including del (5), and unexplained persistent cytopenia.
Eight patients underwent allogeneic or unrelated transplants after the development of t-MDS/t-AML. All patients received busulfan (4 mg/kg/d for 4 days) and cytoxan (60 mg/kg/d for 2 days). Total body irradiation was not used because all patients had received prior irradiation. Three patients died of regimen-related toxicity before day 100, 2 died of graft versus host disease (GVHD) at 2 and 5 months from transplant, and 1 patient died of relapsed MDS at 14 months from transplant. Two patients are alive and well at 18 and 24 months from BMT. Overall, of the 22 patients, 15 have died, with the median actuarial survival being 6 months from the diagnosis of t-MDS/t-AML (range, 1-24 months).
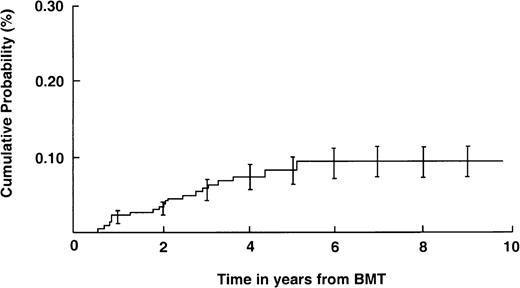
The estimated cumulative probability for morphologic t-MDS/t-AML is shown in Figure 1, and was 8.6% ± 2.1% at 6 years. For the purpose of analysis, patients with morphologic t-MDS/t-AML were further categorized into those with cytogenetic abnormalities suggestive of alkylating agent-associated injury (−5, del(5q) or −7, del(7q); n = 10) and those with abnormalities suggestive of topoisomerase II inhibitor-associated injury (11q23/21q22; n = 6). The cumulative probability of developing alkylating agent-associated t-MDS/t-AML approached 4.7% ± 1.7% at 6 years; that for topoisomerase II inhibitor-associated t-MDS/t-AML was 2.2% ± 0.9%. The median time to development of t-MDS/t-AML was 3.8 years from diagnosis and 2.6 years from transplant for alkylating agent-associated t-MDS/t-AML, and was 3.4 years from diagnosis and 0.9 years from transplant for topoisomerase II inhibitor associated t-AML.
Cumulative probability of t-MDS/t-AML.
The cumulative probability of the occurrence of morphologic t-MDS/t-AML is shown for 612 patients undergoing high-dose chemotherapy with autologous stem cell rescue for Hodgkin's disease and non-Hodgkin's lymphoma. Bars indicate standard errors.
Cumulative probability of t-MDS/t-AML.
The cumulative probability of the occurrence of morphologic t-MDS/t-AML is shown for 612 patients undergoing high-dose chemotherapy with autologous stem cell rescue for Hodgkin's disease and non-Hodgkin's lymphoma. Bars indicate standard errors.
Risk factor analysis
Univariate analysis revealed that age at transplant (< 40 years versus ≥ 40 years) was not associated with an increased risk of developing t-MDS/t-AML (RR = 1.1, P = 0.8). Patients who received PSC alone or BM + PSC following HDT were also not at an increased risk of developing t-MDS/t-AML as compared with patients who received autologous BM alone (RR = 1.2, P = 0.8). Among the recipients of PSC, those patients who received priming with VP-16 for stem cell mobilization (n = 61) were 4.7-fold more likely to develop t-MDS/t-AML as compared with patients who did not receive VP-16 priming (P = .005).
Risk of developing t-AML with 11q23 abnormalities was also assessed for the “pre-priming era” (before 1994, n = 281) and the “priming era” (1994 and after, n = 331). There was a statistically significant increased risk of developing t-AML with 11q23 abnormalities among patients who underwent BMT during and after 1994, when priming with VP-16 was being used for stem cell collection (RR = 5.2, P = .03).
Multivariate analysis revealed priming with VP-16 (RR = 7.7, 95% CI, 2.1-28.7, P = .002) to be independently associated with an increased risk of t-MDS/t-AML (Table 2). Source of stem cells (PSC versus BM), primary disease (HD versus NHL), age at transplant (< 40 years versus ≥ 40 years), and gender were not associated with an increased risk of t-MDS/t-AML.
Multivariate analysis of risk factors associated with t-MDS/t-AML (cohort study)
| Risk Factors . | Total Cohort (n = 612) Relative Risk (95% CI*) . | Hodgkin's Disease (n = 218) Relative Risk (95% CI*) . | Non-Hodgkin's Lymphoma (n = 394) Relative Risk (95% CI*) . |
|---|---|---|---|
| Age at transplant | |||
| <40 y | 1.0 | 1.0 | 1.0 |
| ≥40 y | 1.1 (0.5-2.6) | 1.1 (0.2-5.2) | 2.2 (0.6-8.1) |
| Gender | |||
| Males | 1.0 | 1.0 | 1.0 |
| Females | 2.2 (0.9-5.3) | 2.4 (0.6-9.2) | 1.8 (0.6-5.9) |
| Primary diagnosis | |||
| NHL¶ | 1.0 | ||
| HD† | 1.6 (0.6-3.7) | — | — |
| Source of stem cells | |||
| BM | 1.0 | 1.0 | 1.0 |
| PSC/BM + PSC‡ | 0.9 (0.3-3.0) | 0.8 (0.2-3.8) | 1.0 (0.1-8.1) |
| Priming with VP-16 | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 7.7 (2.1-28.7)† | 8.3 (1.6-43.9)† | 5.9 (0.6-57.1) |
| Risk Factors . | Total Cohort (n = 612) Relative Risk (95% CI*) . | Hodgkin's Disease (n = 218) Relative Risk (95% CI*) . | Non-Hodgkin's Lymphoma (n = 394) Relative Risk (95% CI*) . |
|---|---|---|---|
| Age at transplant | |||
| <40 y | 1.0 | 1.0 | 1.0 |
| ≥40 y | 1.1 (0.5-2.6) | 1.1 (0.2-5.2) | 2.2 (0.6-8.1) |
| Gender | |||
| Males | 1.0 | 1.0 | 1.0 |
| Females | 2.2 (0.9-5.3) | 2.4 (0.6-9.2) | 1.8 (0.6-5.9) |
| Primary diagnosis | |||
| NHL¶ | 1.0 | ||
| HD† | 1.6 (0.6-3.7) | — | — |
| Source of stem cells | |||
| BM | 1.0 | 1.0 | 1.0 |
| PSC/BM + PSC‡ | 0.9 (0.3-3.0) | 0.8 (0.2-3.8) | 1.0 (0.1-8.1) |
| Priming with VP-16 | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 7.7 (2.1-28.7)† | 8.3 (1.6-43.9)† | 5.9 (0.6-57.1) |
95% CI denotes 95% confidence interval.
P < 0.05.
BM indicates bone marrow alone as the source of stem cells; HD, Hodgkin's disease; NHL, non-Hodgkin's lymphoma; PSC/BM + PSC, peripheral stem cells or bone marrow and peripheral stem cells as the source of stem cells.
PSC CD34+ cell dose and risk of t-MDS/t-AML
Information on CD34+ cell dose was available for 258 of the 403 patients (64%) who had received PSC transplants. The median CD34+ cell dose was 3.6 × 106/kg (range, 0.14-57.3). There was a 3-fold increased risk of developing t-MDS/t-AML among patients who had a CD34+ cell dose that was less than or equal to 3 × 106 CD34+cells/kg, as compared with those whose CD34+ cell dose exceeded 3 × 106/kg, but this did not reach statistical significance (P = 0.20).
Priming with VP-16 for PSC collection
Sixty-one patients (22 patients with HD and 39 patients with NHL) received priming with VP-16. These patients were further examined for therapy received before transplant to evaluate the role of prior therapy in this subgroup of patients. Fifty-two of the 61 (85%) patients received 2 g/m2 of VP-16 for priming; the other 9 received either 1 g/m2 or 1.5 g/m2. Priming with granulocyte colony-stimulating factor (G-CSF) alone before VP-16 was attempted in only 2 patients. Three patients developed t-AML in this cohort, and all 3 had 11q23 cytogenetic abnormalities. Pre-BMT chemotherapy was quantified as described under Materials and methods. No significant difference was found in the alkylating agent scores (a reflection of pretransplant alkylating agent exposure) between the patients who did (mean AA score 90) and did not develop t-AML (mean AA score 130, P = .30). Similarly, there was no difference in the topoisomerase score between those who did (mean topoisomerase score 77) and did not develop t-AML (mean topoisomerase score 57,P = .60). The conditioning regimens included Cytoxan, VP-16, and total body irradiation in 43 patients (70%) and Cytoxan, BCNU, and VP-16 in the other 18, and did not appear to influence the risk of t-AML (P = .50).
Hodgkin's disease
The median age at transplant for the 218 patients transplanted for HD was 32.2 years (range, 13-66 years) (see Table 1). Eleven patients developed t-MDS/t-AML with the estimated cumulative probability approaching 8.1% ± 2.5% at 6 years. The median time to development of t-MDS/t-AML was 3.8 years from diagnosis and 0.9 years from transplant. Multivariate analysis revealed priming with VP-16 to be the only independent factor associated with increased risk of t-MDS/t-AML (RR = 8.3, 95% CI 1.6 to 43.9, P = .01) (see Table 2).
Non-Hodgkin's lymphoma
The median age at transplant of the 394 patients with NHL was 44.6 years (range, 6-69 years; see Table 1). Eleven patients developed t-MDS/t-AML with the estimated cumulative probability approaching 9.1% ± 3.0% at 6 years. The median time to development of t-MDS/t-AML was 3.8 years from diagnosis and 2.4 years from transplant. Multivariate analysis failed to reveal any association between t-MDS/t-AML and the risk factors examined (see Table 2).
Case-control study
The characteristics of the cases and the controls are shown in Table3; 64% of the cases and 40% of the controls had AA scores above the median (170) for the whole group. Fifty-five percent of the cases and 46% of the controls had topoisomerase II inhibitor scores above the median (110) for the entire group. The cases were more likely to have received radiation therapy before transplant (50%) as compared to the controls (29%). Again, for the purpose of analysis, patients with morphologic t-MDS/t-AML were further categorized into those with cytogenetic abnormalities suggestive of alkylating agent-associated injury (−5, del(5q) or −7, del(7q)), and those with abnormalities suggestive of topoisomerase II inhibitor-associated injury (11q23/21q22 abnormality).
Characteristics of the patient population (case-control study)
| Patient Characteristics . | Cases3-150 . | Controls3-150 . |
|---|---|---|
| No. patients | 22 | 48 |
| Pretransplant AA score3-151 | ||
| Median | 200.0 | 168.5 |
| AA score ≤170 | 8 (36%) | 29 (60%) |
| AA score >170 | 14 (64%) | 19 (40%) |
| Pretransplant topoisomerase score | ||
| Median | 126.5 | 110.0 |
| Topoisomerase score <110 | 10 (45%) | 26 (54%) |
| Topoisomerase score >110 | 12 (55%) | 22 (46%) |
| Pretransplant radiation | ||
| Yes (25) | 11 (50%) | 14 (29%) |
| No (45) | 11 (50%) | 34 (71%) |
| Source of stem cells | ||
| BM | 4 (18%) | 7 (15%) |
| PSC/BM + PSC | 18 (82%) | 41 (85%) |
| Priming with VP-16 | ||
| No | 18 (72%) | 45 (94%) |
| Yes | 4 (18%) | 3 (6%) |
| Conditioning regimens | ||
| TBI/VP16/CY | 16 (73%) | 33 (69%) |
| CBV | 6 (27%) | 15 (31%) |
| Patient Characteristics . | Cases3-150 . | Controls3-150 . |
|---|---|---|
| No. patients | 22 | 48 |
| Pretransplant AA score3-151 | ||
| Median | 200.0 | 168.5 |
| AA score ≤170 | 8 (36%) | 29 (60%) |
| AA score >170 | 14 (64%) | 19 (40%) |
| Pretransplant topoisomerase score | ||
| Median | 126.5 | 110.0 |
| Topoisomerase score <110 | 10 (45%) | 26 (54%) |
| Topoisomerase score >110 | 12 (55%) | 22 (46%) |
| Pretransplant radiation | ||
| Yes (25) | 11 (50%) | 14 (29%) |
| No (45) | 11 (50%) | 34 (71%) |
| Source of stem cells | ||
| BM | 4 (18%) | 7 (15%) |
| PSC/BM + PSC | 18 (82%) | 41 (85%) |
| Priming with VP-16 | ||
| No | 18 (72%) | 45 (94%) |
| Yes | 4 (18%) | 3 (6%) |
| Conditioning regimens | ||
| TBI/VP16/CY | 16 (73%) | 33 (69%) |
| CBV | 6 (27%) | 15 (31%) |
Group-matching criteria included primary disease, age at transplant (±2 y) and duration of follow-up.
AA score is the alkylating agent score.
TBI/VP-16 indicates conditioning with total body irradiation, etoposide, and cytoxan; CBV, conditioning with cytoxan, BCNU, and vincristine.
Risk factor analysis
As seen in Table 4, multivariate analysis revealed an association between pretransplant radiation therapy and the risk of developing MDS/t-AML, especially among the cohort that had not received VP-16 priming (RR = 3.2, 95% CI, 1.0-10.2, P = .05). In addition, patients who had been primed with VP-16 for stem cell mobilization were at a 12.3-fold increased risk of developing t-AML with 11q23/21q22 abnormalities (P = .006).
Multivariate analysis of risk factors associated with t-MDS/t-AML (case-control study)
| Risk Factors . | All Cases (n = 22) RR (95% CI)4-150 . | -5/5q- or -7/7q(n = 10) RR (95% CI)4-150 . | 11q23/21q22 (n = 6) RR (95% CI)4-150 . |
|---|---|---|---|
| Alkylating agent score | |||
| <170 | 1.0 | 1.0 | 1.0 |
| >170 | 1.2 (0.4-3.4) | 1.5 (0.4-5.4) | 1.1 (0.2-5.1) |
| non-VP-16 primed group4-151 | 1.4 (0.4-4.2) | 1.3 (0.3-4.7) | 2.8 (0.3-29.9) |
| Topoisomerase score | |||
| <110 | 1.0 | 1.0 | 1.0 |
| >110 | 1.0 (0.4-2.8) | 0.8 (0.2-2.8) | 1.4 (0.3-6.5) |
| non-VP-16 primed group4-151 | 1.0 (0.3-3.0) | 0.7 (0.2-2.7) | 2.3 (0.2-24.1) |
| Pretransplant radiation | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 2.5 (0.9-7.3) | 2.4 (0.7-9.0) | 2.3 (0.5-10.9) |
| non-VP-16 primed group4-151 | 3.2 (1.0-10.2)‡ | 2.5 (0.7-9.3) | 7.1 (0.7-76) |
| Source of stem cells | |||
| BM | 1.0 | 1.0 | 1.0 |
| BM + PSC/PSC | 0.9 (0.2-3.5) | 0.6 (0.1-2.9) | 0.5 (0.1-3.3) |
| non-VP-16 primed group4-151 | 0.8 (0.2-3.0) | 0.7 (0.1-3.2) | 0.2 (0.0-1.7) |
| Priming with VP-16 | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 2.9 (0.6-14.3) | NC | 12.3 (2.0-76)‡ |
| Conditioning regimens | |||
| Cytoxan | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 0.5 (0.3-0.9) | 0.3 (0.2-0.6) | 0.2 (0.1-0.4) |
| non-VP-16 primed group4-151 | 0.5 (0.3-0.8) | 0.3 (0.2-0.6) | 0.1 (0.0-0.3) |
| VP-16 | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 0.5 (0.3-0.9) | 0.3 (0.2-0.6) | 0.2 (0.1-0.4) |
| non-VP-16 primed group4-151 | 0.5 (0.3-0.8) | 0.3 (0.2-0.6) | 0.1 (0.0-0.3) |
| BCNU | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 0.7 (0.2-2.1) | 1.0 (0.3-3.8) | 0.6 (0.1-3.1) |
| non-VP-16 primed group4-151 | 0.7 (0.2-2.3) | 1.0 (0.2-3.8) | 0.6 (0.1-5.8) |
| TBI | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 1.5 (0.5-4.6) | 1.0 (0.3-4.1) | 1.8 (0.3-10.1) |
| non-VP-16 primed group4-151 | 1.5 (0.4-5.0) | 1.0 (0.3-4.1) | 1.8 (0.2-19.3) |
| Risk Factors . | All Cases (n = 22) RR (95% CI)4-150 . | -5/5q- or -7/7q(n = 10) RR (95% CI)4-150 . | 11q23/21q22 (n = 6) RR (95% CI)4-150 . |
|---|---|---|---|
| Alkylating agent score | |||
| <170 | 1.0 | 1.0 | 1.0 |
| >170 | 1.2 (0.4-3.4) | 1.5 (0.4-5.4) | 1.1 (0.2-5.1) |
| non-VP-16 primed group4-151 | 1.4 (0.4-4.2) | 1.3 (0.3-4.7) | 2.8 (0.3-29.9) |
| Topoisomerase score | |||
| <110 | 1.0 | 1.0 | 1.0 |
| >110 | 1.0 (0.4-2.8) | 0.8 (0.2-2.8) | 1.4 (0.3-6.5) |
| non-VP-16 primed group4-151 | 1.0 (0.3-3.0) | 0.7 (0.2-2.7) | 2.3 (0.2-24.1) |
| Pretransplant radiation | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 2.5 (0.9-7.3) | 2.4 (0.7-9.0) | 2.3 (0.5-10.9) |
| non-VP-16 primed group4-151 | 3.2 (1.0-10.2)‡ | 2.5 (0.7-9.3) | 7.1 (0.7-76) |
| Source of stem cells | |||
| BM | 1.0 | 1.0 | 1.0 |
| BM + PSC/PSC | 0.9 (0.2-3.5) | 0.6 (0.1-2.9) | 0.5 (0.1-3.3) |
| non-VP-16 primed group4-151 | 0.8 (0.2-3.0) | 0.7 (0.1-3.2) | 0.2 (0.0-1.7) |
| Priming with VP-16 | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 2.9 (0.6-14.3) | NC | 12.3 (2.0-76)‡ |
| Conditioning regimens | |||
| Cytoxan | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 0.5 (0.3-0.9) | 0.3 (0.2-0.6) | 0.2 (0.1-0.4) |
| non-VP-16 primed group4-151 | 0.5 (0.3-0.8) | 0.3 (0.2-0.6) | 0.1 (0.0-0.3) |
| VP-16 | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 0.5 (0.3-0.9) | 0.3 (0.2-0.6) | 0.2 (0.1-0.4) |
| non-VP-16 primed group4-151 | 0.5 (0.3-0.8) | 0.3 (0.2-0.6) | 0.1 (0.0-0.3) |
| BCNU | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 0.7 (0.2-2.1) | 1.0 (0.3-3.8) | 0.6 (0.1-3.1) |
| non-VP-16 primed group4-151 | 0.7 (0.2-2.3) | 1.0 (0.2-3.8) | 0.6 (0.1-5.8) |
| TBI | |||
| No | 1.0 | 1.0 | 1.0 |
| Yes | 1.5 (0.5-4.6) | 1.0 (0.3-4.1) | 1.8 (0.3-10.1) |
| non-VP-16 primed group4-151 | 1.5 (0.4-5.0) | 1.0 (0.3-4.1) | 1.8 (0.2-19.3) |
95% confidence interval.
Non-VP-16 primed group denotes patients who did not receive priming with VP-16 prior to stem cell collection.
P ≤ 0.05.
NC indicates not convergent.
Discussion
High-dose chemoradiotherapy with stem cell rescue has emerged as the treatment of choice for patients with lymphoid malignancies who have suboptimal response to initial therapy or for patients with refractory or relapsed disease.1 With the increased success of this therapeutic option, there have been several reports of t-MDS/ t-AML.12-18 Some of the risk factors predicting an increased risk of t-MDS/t-AML following transplant have included older age at transplant,14,17 radiation therapy,15,16and a low platelet count at transplant.16 It is unclear whether t-MDS/t-AML is related to pretransplant chemotherapy and radiotherapy, or transplant conditioning or stem cell priming regimens, or the source of stem cells, or is a cumulative effect of all of these exposures. This study evaluated whether pretransplant therapeutic exposures or transplant conditioning and stem cell priming regimens were associated with an increased risk of t-MDS/t-AML. Among the 612 patients who were treated with HDT and stem cell rescue at the City of Hope National Medical Center between 1986 and 1998 for HD and NHL, the cumulative risk of t-MDS/t-AML was 8.6% at 6 years for the entire cohort. The cumulative probability was 8.1% and 9.1% for patients with a primary diagnosis of HD and NHL, respectively.
Therapy-related MDS/AML is a well-known late complication after conventional chemotherapy or radiation therapy for treatment of lymphoid malignancies.21-37 The incidence of t-MDS/t-AML following conventional chemotherapy ranges from 0.8% at 30 years37 to 6.3% at 20 years.26 Some of the factors associated with an increased risk of t-MDS/t-AML in this population include older age at diagnosis and treatment,24-26 alkylating agents,24,28combined modality therapy (radiation and chemotherapy),29-32 epipodophyllotoxins,33,34and splenectomy.26,35 36 The current nested case-control study offered more detailed information on exposure to various chemotherapeutic agents before transplant. To obtain an index of the total amount of the alkylating agents and topoisomerase II inhibitors received, we used a previously developed score as a method for combining different drugs. Summing the individual drug scores produced a measure of exposure. An attempt was made to evaluate the separate effects of individual alkylating agents and topoisomerase II inhibitors, but this was not possible because of small numbers and because drugs were frequently given in combination. No association was shown between pretransplant exposure to the various chemotherapeutic agents and t-MDS/ t-AML in this study. However, there was an association between radiation therapy given before transplant and the risk of developing t-MDS/t-AML, which was particularly apparent among patients who had not been primed with VP-16 for stem cell mobilization.
Use of VP-16 has been shown to be an effective and safe method for mobilization of PSC and an effective agent in tumor reduction in patients with NHL and HD.41 42 VP-16 as a priming agent for PSC mobilization was initiated in 1994 at City of Hope, and so far 61 patients have received primed stem cell transplants. VP-16 was used for the dual purposes of cytoreduction and PSC mobilization. The dose of VP-16 used for priming in our study population was 2000 mg/m2 in 85% of this cohort and 1000 to 1500 mg/m2 in the rest. Patients were not randomized to priming with VP-16 and G-CSF versus G-CSF alone. Only 2 patients had failed initial priming attempts with G-CSF alone. Three patients who had received VP-16 priming developed t-AML, and all 3 had 11q23 cytogenetic abnormalities. This study demonstrated that priming with VP-16 was a predictor for t-AML with 11q23/21q22 abnormalities. There was a 5-fold increased risk of developing t-AML for patients transplanted after 1994, as compared with those transplanted before 1994, further suggesting a correlation between VP-16 priming and t-AML.
Exposure to epipodophyllotoxins in a nontransplant setting has been associated with increased risk of AML, typically characterized by a short latency (median of 24-30 months), predominance of monocytic phenotypes (M4 and M5), and acute onset, often with a high blast count, rather than an initial myelodysplastic presentation.33,34,38-40 In addition, there appears to be a dose-intensity effect, with the risk of leukemia remaining low in patients receiving 2000 mg/m2 VP-16 or less, but increasing rapidly in patients receiving high doses, with greatly elevated risks among patients receiving more than 4000 mg/m2.38,43 44 Because VP-16 priming was not offered as part of a randomized study, we wanted to explore any differences in prior therapy that could have influenced the risk of developing t-AML. Therefore, patients who had received priming with VP-16 were examined for therapy received before transplant. There was no difference in the topoisomerase score between those that did and did not develop t-AML. In addition, there was no significant difference in the alkylating agent scores between the patients who did and did not develop t-AML. The conditioning regimens did not influence the risk of t-AML. However, the small number of events and the brief follow-up period for the cohort that received VP-16 priming allow us to ascribe only a limited significance to this risk factor.
No association was seen between the conditioning regimens used and the risk of t-MDS/t-AML. Total body irradiation as a risk factor for t-MDS/t-AML has been reported previously.15 45 In our study, however, exposure to radiation as total body irradiation given as part of the myelosuppressive regimen for the transplant process was not a significant risk factor. Again, the failure to demonstrate an association could possibly be because of small numbers or because of a lack of heterogeneity in the treatment exposures received by the case and control populations.
No pretransplant karyotypic abnormalities were detected among the patients who developed t-MDS/t-AML post-BMT. The onset of karyotypic abnormalities was after transplant in all patients who developed t-MDS/t-AML. Because the BM or PSC were not exposed to the transplant conditioning therapy, the source of the eventual cytogenetic abnormalities would therefore be either the transplanted autologous stem cells (injured by pretransplant chemotherapy or stem cell priming regimens or both) or residual marrow cells, assuming less than complete eradication of all endogenous bone marrow by the myeloablative conditioning regimens. At present no method is available to predict who is at increased risk for developing this complication, although there are reports in the literature attempting to identify populations at increased risk.46-48 Legare et al showed that clonality analysis can be predictive of the development of t-MDS/t-AMT after autologous transplant, and could potentially offer important insights into the pathogenesis and associated risk factors of t-MDS/t-AML.46 Abruzzese et al conducted a retrospective study examining pretransplant marrow or peripheral stem cells from 11 patients who subsequently developed myelodysplasia after HDT.47 To determine if the abnormal clone was present prior to HDT, they used fluorescent in situ hybridization to detect the cytogenetic markers observed at the onset of MDS. In 8 of the 11 cases, the same cytogenetic abnormality observed at the time of MDS diagnosis was detected in the pre-HDT specimen, thus supporting the hypothesis that stem cell damage leading to posttransplant MDS may result from prior conventional-dose chemotherapy. To formally prove the source of the myelodysplastic clone, however, we would have to genetically mark the graft,49 and eventually assay the myelodysplastic clone.
Therapy-related MDS/AML is associated with a very poor outcome, with an estimated 12-month survival of 10%.50 This study has shown that patients undergoing HDT with stem cell rescue are at an increased risk of t-MDS/t-AML, especially those receiving priming with VP-16 for PSC collection. The use of increasingly intensive chemotherapy with stem cell support means that t-MDS/t-AML is likely to remain an important clinical problem. Appropriate surveillance of treatment-specific cohorts is essential to characterize the incidence and the risk factors for the occurrence of t-MDS/t-AML. Moreover, identification of populations with increased genetic susceptibility to leukemia may allow prevention or early treatment of t-MDS/t-AML.
Supported in part by grants CA 30206 and CA 33572 from the National Cancer Institute.
Reprints:Smita Bhatia, Division of Pediatric Oncology, City of Hope National Medical Center, 1500 East Duarte Road, Duarte, CA 91010-3000; e-mail: sbhatia@smtplink.coh.org.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal