With the aim of determining the incidence of idiopathic thrombocytopenic purpura (ITP) in adults, we searched all adult ITP patients diagnosed from April 1, 1973 to December 31, 1995 in the County of Funen in Denmark. This county comprises 9% of the total Danish adult population. A total of 221 patients fulfilled the inclusion criteria, yielding an annual standardized incidence rate of 2.68 per 100,000. The median age of the patient population was 56 years, and the female to male ratio was 1.7. Changing the platelet count cut-off point from 100 × 109/L to 50 × 109/L changed the incidence rate to 2.25 per 100,000. Comparing patients less and more than 60 years old, the incidence rate more than doubled and the sex difference was eliminated in the older age group. These two age groups were almost identical regarding platelet count at diagnosis and number of asymptomatic cases. The incidence rate increased in the study period. This increase in particular involved asymptomatic patients and old males who were both symptomatic or not symptomatic. Including additional patients identified by a questionnaire study of the contribution from the primary care physicians and the practicing specialists in the second half of the study period, a reliable estimate of the annual ITP incidence in Danish adults, using a platelet concentration cut-off point of 50 × 109/L, is 3.2 per 100,000 persons.
DESPITE THE FACT THAT idiopathic thrombocytopenic purpura (ITP) is considered a relatively common and easily recognized disease, no firm data are available on its incidence. Based on 2 differently structured case studies and 1 quoted estimate of the incidence of childhood ITP, an adult ITP incidence of 6.6 per 100,000 persons per year was estimated by extrapolation from other case series, including both children and adults.1 Even if it is the general view that most patients are young women,1 the impression that the adult ITP population may be older than hitherto supposed has been expressed previously.2 3 However, there are no firm data describing the demographic aspects of adult ITP. In an attempt to address this issue, we have studied all cases of adult ITP in the well-defined health care region of a Danish county during a 22.75-year period.
MATERIALS AND METHODS
The background population and the health care system.
In 1984, corresponding to the middle of the study period, the population of the County of Funen comprised 368,491 inhabitants more than 15 years of age, corresponding to 8.9% of the analogous total Danish population. In 1973 and 1995, the numbers were 339,578 and 387,841, respectively, corresponding to 8.8% and 9.0% of the total Danish population more than 15 years of age. Valid data describing the mobility of the inhabitants of the County of Funen exist from 1979 and onwards. In 1979, 1987, and 1995, the fractions of newcomers more than 15 years of age constituted 2.2%, 2.3%, and 2.4%, respectively. The corresponding fractions of residents leaving the county were 2.2%, 2.2%, and 2.5%, respectively. The health care system of the County of Funen that takes care of virtually all patients living in its area consists of one tertiary referral center (Odense University Hospital, Odense, Denmark) and 9 county hospitals, with a total of 63 out-patient clinics attached. The number of general practices at the end of the study period was 183, corresponding to 282 doctors. In addition, the 11 practicing internists and dermatologists of the county were found relevant for this study.
Searching the records of ITP patients.
We retrieved the records of all ITP patients more than 15 years of age living in the County of Funen at the time of diagnosis in the 22.75-year period from April 1, 1973 to December 31, 1995. During this period, all discharge diagnoses in the county were entered into a computer database. In the out-patient clinics, registration of diagnoses started at different times from 1978 to 1993; the hematological out-patient clinic at Odense University Hospital entered data from 1983.
An initial computer search was conducted applying the following patient characteristics: (1) residency in the County of Funen at the time of diagnosis; (2) more than 15 years of age; and (3) characterized by one or more of the following ICD 8 and ICD 10 classification codes at discharge (Denmark never used the ICD 9): ICD 8 codes: 287.10 (idiopathic thrombocytopenia), 287.11 (secondary thrombocytopenia); 287.18 (thrombocytopenia, unspecified); 287.19 (thrombocytopenia); and 675.09 (other coagulopathies after childbirth); ICD 10 codes (from January 1, 1994): D69.3 (idiopathic thrombocytopenic purpura), D69.4 (other primary thrombocytopenia), D69.5 (secondary thrombocytopenia), D69.6 (thrombocytopenia, unspecified), and O72.3 (postpartum coagulation defects). The ICD 8 classification code 287.99 (hemorrhagic disease not otherwise specified) corresponding to unspecific bleeding tendency was included initially. After the observation that none of 180 patients corresponding to this code fulfilled the criteria for inclusion, this code and the corresponding ICD 10 code were subsequently omitted.
After a thorough review of the medical records of all patients found by the intial computer search, patients were included if they had a platelet count less than 100 × 109/L and did not show any signs of other hematological disorders, ie, leukemia, lymphoma, myelodysplastic syndrome, congenital thrombocytopenia, etc. Other reasons for exclusion were suspected or known chronic hepatic disease and/or alcohol abuse associated with slight or moderate thrombocytopenia, solid tumors (both with and without bone marrow involvement), systemic lupus erythematosus criteria fulfilled at the appearance of thrombocytopenia, disseminated intravascular coagulation, thrombotic thrombocytopenic purpura, pseudothrombocytopenia, drug-induced thrombocytopenia, human immunodeficiency virus (HIV)-associated thrombocytopenia, and transient gestational thrombocytopenia.
Thrombocytopenic patients who had a previous history of thrombocytopenia either before 15 years of age or before April 1, 1973 were included if they had a preceding unmaintained normal platelet count of at least 2 years in duration. A bone marrow examination was not a prerequisite for inclusion. In patients without a bone marrow study, at least 6 months of follow-up were required to exclude other hematological disorders. When performed, the bone marrow study should show a normal or increased amount of megakaryocytes.
With the purpose of searching ITP patients from the County of Funen that had been diagnosed in hospitals outside Funen, we also extracted data from the National Hospital Discharge Registry. This data extraction, which was based on the previously mentioned criteria and which covered all Danish hospitals and out-patient clinics outside the County of Funen, resulted in the inclusion of 1 further patient.
ITP patients diagnosed and treated outside the hospital system.
To get an estimate of the number of ITP patients that had been diagnosed and observed solely in the primary care system, all general practitioners, internists, and dermatologists of the county were questioned as to whether they remembered having diagnosed and possibly treated ITP patients without referring them within the past 2 years. In addition, they were asked if they would themselves treat symptomatic patients outside the hospital system.
Statistics.
Continuous independent variables were analyzed by parametric statistics (Student’s t-test). Normal distribution was confirmed with the Lilliefors test. Normality was rejected at P < .1. In these cases, lognormal distribution was tested after logarithmic transformation. In the remaining cases, nonparametric tests (Mann-Whitney and Kruskal-Wallis) were used. Categorical data were analyzed using the χ2 test with Yates’ continuity correction. Comparison of incidence rates was performed using the Poisson distribution. A general two-sided significance level of 5% was applied.
Ethics.
The study was approved by The Regional Scientific-Ethical Committee and by The Danish Data Protection Agency.
RESULTS
Incidence rates.
Seven hundred sixty-one patients fulfilled our primary inclusion criteria. Corresponding to these patients, 731 records were available. Eighteen of the 30 missing records had been destroyed 10 years after the death of the patients, according to the practice of some departments. The missing patients did not differ from the remaining patients regarding age or sex. Only 3 patients, 2 of whom were excluded, were found by searching hospitals outside the County of Funen. Altogether, 221 patients fulfilled our ITP criteria. Eleven patients had a previous history of ITP 2 to 26 years (median, 13 years) before the present episode. The median age of these patients at the time of the initial diagnosis was 13 years (range, 3 to 60 years).
The 221 patients comprise 139 women (63%) and 82 men (37%), yielding a female to male (F/M) ratio of 1.7. The median age of the entire population is 56.4 years (females, 55.6 years; males, 61.6 years). In patients more than 60 years of age, the F/M ratio is 1.3; in patients less than 60 years of age, the F/M ratio is 2.1. This difference is not significant.
The overall ITP incidence rate is 2.64/105/yr (95% confidence interval [CI], 2.29 to 2.98; women, 3.25 [95% CI, 2.71 to 3.79]; men, 2.00 [95% CI, 1.57 to 2.43]). Applying these observed rates to the total Danish population, we found an almost identical age- and sex-standardized overall incidence rate of 2.68/105/yr (95% CI, 2.33 to 3.03; women, 3.28 [95% CI, 2.74 to 3.82]; men, 2.06 [95% CI, 1.62 to 2.50]). The overall incidence rate of ITP with a platelet count less than 50 × 109/L at diagnosis is 2.25/105/yr (95% CI, 1.92 to 2.57; women, 2.71 [95% CI, 2.22 to 3.20]; men, 1.78 [95% CI, 1.37 to 2.19]).
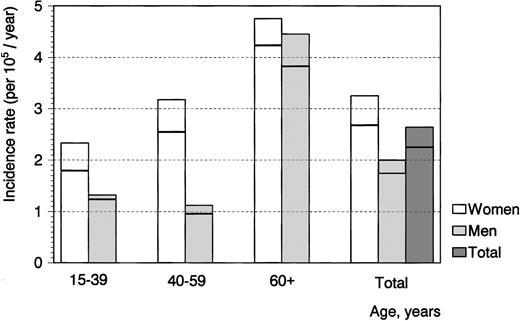
Figure 1 displays incidence rates in 3 age groups. It can be seen that the incidence rate increases with age, reaching 4.62/105/yr (95% CI, 3.72 to 5.52) in persons more than 60 years of age and 1.94/105/yr (95% CI, 0.59 to 2.29) in those less than 60 years of age. In addition, the sex difference is eliminated in individuals more than 60 years of age. It can further be seen that the modest reduction in incidence rate after the application of a cut-off point of 50 × 109/L applies to younger and middle-aged women in particular. Using this criterion, we found an annual incidence rate of 4.07 (95% CI, 3.22 to 4.92) in persons more than 60 years of age and of 1.61 (95% CI, 1.29 to 1.93) in those less than 60 years of age.
ITP incidence rates according to age and sex. The horizontal bars correspond to incidence rates using a platelet count cut-off point of 50 × 109/L.
ITP incidence rates according to age and sex. The horizontal bars correspond to incidence rates using a platelet count cut-off point of 50 × 109/L.
Platelet counts and bleeding symptoms.
The median platelet count at diagnosis was 12 × 109/L (range, 0 to 95 × 109/L). Approximately 45% of the patients had a platelet count less than 10 × 109/L, and 85% had a count less than 50 × 109/L. In patients with very low platelet counts, the difference in incidence between men and women is almost eliminated. In accordance with this, the initial median platelet count was 15 × 109/L in women and 8 × 109/L in men (P = .03). The corresponding counts in patients less than and more than 60 years of age were 16 × 109/L (women) and 8 × 109/L (men) and 11 × 109/L (women) and 7 × 109/L (men), respectively. Forty-six (21%) asymptomatic patients were diagnosed incidentally. Their median platelet count was 49 × 109/L (range, 3 to 92 × 109/L). In patients less than 60 years of age, 20% were asymptomatic; in patients more than 60 years of age, the corresponding fraction was 22%. Twenty-five patients (11%) experienced severe bleeding at diagnosis (10 patients <60 years of age and 15 patients ≥60 years of age). Severe mucosal bleeding was seen in 16 patients (6 patients <60 years of age and 10 patients ≥60 years of age), with 9 patients showing extensive cutaneous bleeding (3 patients <60 years of age and 6 patients ≥60 years of age). One patient less than 60 years of age showed a large intramuscular hematoma. The 2 age groups did not differ significantly regarding frequency of severe bleeding (P = .13) or mucosal bleeding per se (P = .09). The platelet count averaged 5.0 × 109/L in the 10 patients less than 60 years of age and 4.7 × 109/L in the 15 patients ≥60 years of age. A male patient who was 86 years of age died from intestinal hemorrhage 10 days after diagnosis with a platelet count of 12 × 109/L. Additionally, a woman 75 years of age died 5 months after the diagnosis from intestinal, pleural, and cerebral hemorrhage after a relapse (platelet count, 5 × 109/L). These fatalities occurred in the period from 1973 to 1974. Inclusion of the latter case yields a difference between the 2 age groups of borderline significance (severe bleeding as a whole:P = .09; severe mucosal bleeding: P = .06). Patients both less than and greater than 60 years of age were observed for a median of 26 months. No severe bleeding episodes were seen in 16 patients who had platelet counts persistingly less than 50 × 109/L and who were observed for a median of 24 months. In the patient group as a whole, 55 have died, with 53 of them dying from causes other than hemorrhage.
Bone marrow examination.
A bone marrow study was performed in 195 patients (88%). The proportion of patients who underwent this examination was constant during the period. The median age of the examined patients (57.2 years) differed significantly from that of the patients not examined (37.6 years; P = .03). The median platelet count at diagnosis was 10 × 109/L and 24 × 109/L in examined and nonexamined patients, respectively (P = .005). A bone marrow study was performed in 92% of patients more than 60 years of age and in 91% of patients with a platelet count less than 50 × 109/L at diagnosis.
Temporal variations.
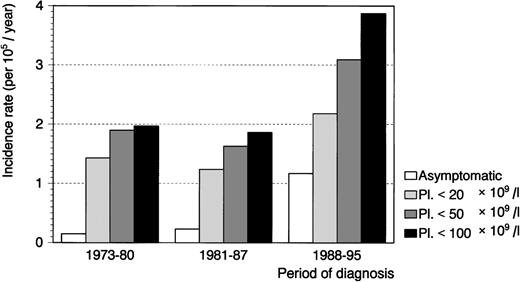
As shown in Fig 2, the number of patients increased during the study period. This increase, which started in the late 1980s, involved patients with high platelet counts in particular. Accordingly, the median platelet counts at diagnosis were 7 × 109/L, 10 × 109/L, and 16 × 109/L in 1973 to 1980, 1981 to 1987, and 1988 to 1995, respectively. Comparing the incidence rates before and after January 1, 1985 in various groups of patients and using 3 platelet count cut-off points gave the following results (incidence rates are expressed as the number per 105 persons per year; CIs are not shown). At less than 100 × 109/L, the values were as follows: overall before, 1.94, and overall after, 3.33 (P < .0001); women before, 2.30, and women after, 4.20 (P = .0004); men before, 1.56, and men after, 2.43 (P = .03); patients less than 60 years of age before, 1.58, and patients less than 60 years of age after, 2.27 (P = .01); patients ≥60 years of age before, 2.94, and patients ≥60 years of age after, 6.40 (P < .0001). At less than 50 × 109/L, the values were as follows: overall before, 1.84, and overall after, 2.67 (P = .007); women before, 2.16, and women after, 3.27 (P = .007); men before, 1.51, and men after, 2.04 (P = .09); patients less than 60 years of age before, 1.49, and patients less than 60 years of age after, 1.73 (P = .2); patients ≥60 years of age before, 2.85, and patients ≥60 years of age after 5.38 (P< .0001). At less than 20 × 109/L, the values were as follows: overall before, 1.43, and overall after, 1.86 (P = .07); women before, 1.64, and women after, 2.29 (P = .08); men before, 1.22, and men after, 1.41 (P = .3); patients less than 60 years of age before, 1.13, and patients less than 60 years of age after, 1.19 (0.4); patients ≥60 years of age before, 2.30, and patients ≥60 years of age after, 3.80 (P < .0001). The increasing number of patients applies to women of all ages and to old men. Accordingly, the age of the male patients changed from a median of 35.1 years in 1973 to 1980 to 45.8 years in 1981 to 1987 and 65.6 years in 1988 to 1995 (P = .01). The corresponding figures for women are 55.6, 55.6, and 54.2 years, respectively (P = .9). In symptomatic male patients, the median ages in the 3 periods were 33.3, 47.7, and 65.3 years, respectively (P = .01).
In accordance with the finding of increasing platelet counts, the number of asymptomatic patients increased in the study period. The incidence rates of symptomatic ITP before and after January 1, 1985 were 1.82/105/yr and 2.36/105/yr, respectively (P = .05). The corresponding incidence rates of asymptomatic patients were 0.12/105/yr and 0.98/105/yr (P < .0001).
Referral pattern.
The number of in-patients and out-patients was 196 and 25, respectively. Twenty-four of the 25 out-patients were seen in the specialized department. Twenty-two of these (92%) were seen from 1990 to 1995, ie, in the latter half of this department’s computerized out-patient data entry period.
The questionnaires forwarded to the general practitioners and practicing specialists resulted in a 94% response rate. From the answers it can be estimated that 2 ITP patients with platelet counts less than 50 × 109/L and 6 patients with platelet counts between 50 × 109/L and 100 × 109/L were diagnosed annually outside the hospital system in the County of Funen. It can also be concluded that presumably all symptomatic ITP patients would be referred to the hospital system. Provided that these estimates are valid, they result in an increase in the overall ITP incidence rate from 2.64/105/yr to 4.81/105/yr (95% CI, 4.34 to 5.28). If only platelet counts less than 50 × 109/L at diagnosis are considered, the incidence rate increases from 2.25/105/yr to 2.80/105/yr (95% CI, 2.44 to 3.16) in the study period as a whole and from 2.67 to 3.22 in the period from 1985 to 1995.
DISCUSSION
The fact that ITP remains a diagnosis of exclusion has made study of its epidemiologic and demographic aspects difficult. Consequently, firm data on its incidence are not available. Based on a literature review, George et al1 estimated an annual ITP incidence rate of 1.0 to 12.5 per 100,000 persons (children and adults). All investigators agree that there is a female preponderance, with an estimated F/M ratio of 2.6:1,1 and it is a general belief that ITP is typically a disease of young adults, with a peak of occurrence between 15 and 40 years of age and a decreasing rate of incidence with age.
In the present study, we have made a careful search for all adult ITP patients diagnosed during a 22.75-year period in a well-defined Danish health care region with a stable, representative population. Using a platelet concentration cut-off point of 100 × 109/L, we found an annual incidence rate of 2.64 per 100,000 persons. Considering only platelet counts less than 50 × 109/L, the incidence rate decreased to 2.25 per 100,000 persons. Our F/M ratio is 1.7, which is somewhat lower than that reported in previously published series.1 Besides, a remarkable and rather surprising finding is the median age of 56 years of our patient population. We found an increasing annual ITP incidence with age, reaching 4.6 per 100,000 persons more than 60 years of age. Furthermore, the sex difference was eliminated in this older group of patients. The validity of our finding is supported by the fact that the older patients did not differ from their younger counterparts as regards platelet concentration at diagnosis. Accordingly, lowering the platelet concentration threshold to 50 × 109/L and excluding asymptomatic patients does not affect our results. Considering the estimated low number of patients treated in the primary health care system, it is unlikely that the age composition of the patients is affected by referral bias. The high frequency of bone marrow examination, particularly in the older patients, makes erroneous inclusion of patients with myelodysplastic syndromes very unlikely. Accordingly, no ITP patient from the study period has so far been seen in the region’s specialized department of hematology with a subsequent diagnosis of myelodysplasia. It is also unlikely that drug-induced thrombocytopenia contributes to the high ITP incidence in the older patients, because the administration of candidate drugs was stopped in almost all patients.
It is of interest that an increased incidence with age has previously been described in hemolytic anemia4 and quite recently in systemic lupus erythematosus as well.5
Almost half of our patients are more than 60 years of age. Two patients, 75 and 86 years of age, died from excessive bleeding. Apart from this, it is remarkable that old and young patients with comparable platelet counts at diagnosis and subsequent follow-up periods seemed to show the same severity of bleeding. Even if we found a trend towards more cases of severe bleeding in the older age group, our results contrast with previous studies that have shown an increased risk of severe bleeding in aged patients with ITP.6 7 Selection bias and a rather low number of old patients in these studies may contribute to this discrepancy.
The temporal variation in the incidence pattern deserves special consideration. The annual incidence rate increased from 1.94 to 3.33 per 100,000 persons in the halves of the study period. A somewhat less pronounced increase, from 1.84 to 2.67, was seen if the 50 × 109/L platelet count criterion was applied. Accordingly, the number of asymptomatic patients increased considerably with time. Presumably, this can be ascribed to incidental finding of slightly lowered platelet counts during routinely performed platelet counting after the introduction of automated platelet counting.
It is remarkable that the conspicuously increased ITP incidence of older patients with time involved males in particular. This increase, the cause of which is not known, must be real in view of the fact that this trend was also found in symptomatic male patients.
It is likely that the vast majority of symptomatic patients are referred, ie, patients with platelet counts less than 50 × 109/L.8 Considering the ITP incidence in the second half of our study period and the result of our questionnaire study of the contribution from the primary care physicians, a realistic estimate of the annual ITP incidence in Danish adults, using a platelet concentration cut-off point of 50 × 109/L, is 3.2 per 100,000 persons. The corresponding estimate of 5.5 per 100,000 per year using a 100 × 109/L threshhold is subject to some uncertainty because of the lack of precise knowledge of the exact number of patients observed exclusively in the primary health care system and (not least) because of the unknown number of patients with asymptomatic ITP.
Supported by grants from the Dagmar Marshall’s Foundation, Denmark; the Family Hede Nielsen’s Foundation, Denmark; and the Asta og Peter Gøtz-Petersen’s Foundation, Denmark.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Kai Schmidt, MD, Department of Hematology, Odense University Hospital, DK-5000 Odense C, Denmark.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal