Basic fibroblast growth factor (bFGF) is a secreted multifunctional cytokine and a potent stimulator of angiogenesis in vivo. Elevated bFGF concentrations have been detected in the serum and urine of cancer patients. We measured bFGF by enzyme-linked immunosorbent assay from sera taken from 160 non-Hodgkin’s lymphoma (NHL) patients before treatment and stored at −20°C. The patients had been observed for at least 5 years or until death. Serum bFGF concentrations (S-bFGF) ranged from undetectable to 34.7 pg/mL (median, 3.3 pg/mL). S-bFGF was detectable with a similar frequency in all subtypes of NHL. A high pretreatment S-bFGF was associated with poor overall survival. The 5-year survival rate of the patients within the highest quartile of S-bFGF concentrations (S-bFGF = 5.5 pg/mL) was only 39%, in contrast to a 60% survival rate of the patients with lower S-bFGF (P = .019). A high S-bFGF (within the highest quartile) was associated with poor outcome also in large-cell diffuse and immunoblastic lymphomas (5-year survival rates of 28% v56%, respectively; P = .027), which was the largest histologic subgroup (n = 66) within the series. In multivariate analyses, S-bFGF was an independent prognostic factor, both when the highest quartile was used as a cut-off value (P = .0079) and when S-bFGF and the other parameters were entered into the model as continuous variables (P = .024). In the multivariate analyses, S-bFGF had a noticeably stronger prognostic value than serum lactate dehydrogenase and the number of extranodal tumor sites, both of which are currently included as components in the International Prognostic Index.
ANGIOGENESIS, THE sprouting of new capillaries from pre-existing ones, is an important component in many physiological and pathological processes (reviewed by Folkman1). In healthy adults, extensive angiogenesis occurs only in the female reproductive system. Angiogenesis also takes place in conditions such as wound healing, rheumatoid arthritis, psoriasis, and diabetic retinopathy. In cancer, active angiogenesis is a prerequisite for tumor growth beyond a few cubic millimeters in size. In addition, the dissemination of malignant tumors is dependent on angiogenesis. Analyses of metastatic colonies in mouse lungs have shown that the colonies must become neovascularized before they can grow larger than microscopic in size.2 3
Angiogenesis is regulated by a balance of various positive and negative angiogenic molecules (reviewed by Hanahan and Folkman4 and Iruela-Arispe and Dvorak5). During tumorigenesis, the vasculature becomes activated to grow new capillaries in response to appropriate stimuli. One such stimulus is basic fibroblast growth factor (bFGF), which is also called fibroblast growth factor-2 (FGF-2). bFGF is a 18- to 24-kD polypeptide that is expressed widely in cells of mesodermal and neuroectodermal origin and in a variety of malignant tumors and cancer cell lines (reviewed by Friesel and Maciag6 and Bikfalvi et al7). bFGF is a mitogen for endothelial cells and fibroblasts in vitro and a potent inducer of angiogenesis in vivo. In addition to stimulating the growth of blood vessels, bFGF has also been shown to inhibit the adhesion of activated natural killer cells to tumor vessel endothelium.8 This suggests that the presence of bFGF at the tumor site may provide protection to growing tumor vessels. In nude mouse transplanted with cancer cells, tumor growth could be suppressed by using immunoneutralizing monoclonal antibody against bFGF.9Similarly, the inhibition of bFGF-mediated signaling in human melanomas, using episomal vectors containing antisense-oriented bFGF cDNA, resulted in a complete arrest of the tumor growth or the tumors regressed as a result of blocked intratumoral angiogenesis and subsequent necrosis.10
Using a transgenic mouse model, Kandel et al11 found that the angiogenic swich in bovine papilloma virus-induced fibrosarcoma correlates with the export of bFGF from tumor cells. Abnormally elevated levels of bFGF have indeed been reported in serum12-17 and urine16,18-20 of patients with various types of cancer. A high serum concentration of bFGF (S-bFGF) has been shown to be associated with a large primary tumor size in head and neck cancer16 and with a short tumor volume doubling time in advanced colorectal cancer.13 Nevertheless, little is known about the clinical significance of S-bFGF, and there are no studies available on the prognostic value of S-bFGF in any type of human cancer. In the present study, we measured S-bFGF concentrations from lymphoma patients’ sera stored for years at −20°C and found that a high S-bFGF at diagnosis was associated with poor prognosis both in univariate and multivariate survival analyses.
MATERIALS AND METHODS
Patients.
S-bFGF concentration was measured in 160 randomly selected adult patients with non-Hodgkin’s lymphoma (NHL) diagnosed and treated in the Department of Oncology, Helsinki University Central Hospital (Helsinki, Finland), from 1981 to 1987, for whom frozen serum taken at the time of diagnosis but before lymphoma treatment was available. Thirty-eight lymphomas (24%) had been classified as low-grade, 80 (50%) as intermediate-grade, and 38 (24%) as high-grade lymphoma according to the Working Formulation Scheme21 by a pathologist with a special interest in lymphoma. Four cases (2%) were considered unclassifiable. The histologic types of lymphomas in the series according to the Working Formulation Scheme were small lymphocytic, consistent with chronic lymphocytic leukemia (CLL; n = 11; 7%); small lymphocytic, plasmocytoid (n = 2; 1%); follicular, predominantly small cleaved cell (n = 19; 12%); follicular, mixed small and large cell (n = 2; 1%); follicular, predominantly large cell (n = 2; 1%); diffuse, small cleaved cell (n = 11; 7%); diffuse, mixed small and large cell (n = 6; 4%); diffuse, large cell (n = 47; 29%); large cell immunoblastic (n = 19; 12%); lymphoblastic (n = 5; 3%); small noncleaved cell, non-Burkitt (n = 6; 4%); small noncleaved cell, Burkitt’s type (n = 2; 1%); mycosis fungoides (n = 1; 1%); other (n = 23; 14%); and unclassifiable (n = 4; 2%). Clinical staging was performed according to the Ann Arbor classification system. The examination of clinical status, chest x-ray, computerized tomography (CT) scans of the mediastinum and the abdomen, and a bone marrow biopsy were performed as staging examinations. Fifty-five (34%) of the patients had stage I, 40 (25%) stage II, 27 (17%) stage III, and 38 (24%) stage IV disease at diagnosis. Thirty patients (19%) had B-symptoms (weight loss, unexplained fever, or night sweats). The International Prognostic Index (IPI)22 could be determined in all cases.
A total of 113 patients were treated with combination chemotherapy. The patients with intermediate- or high-grade lymphoma and disseminated disease were treated usually with bleo-CHOP (bleomycin, cyclophosphamide, doxorubicin, vincristine, prednisone), M-BACOD (methotrexate, bleomycin, doxorubicin, cyclophosphamide, vincristine, dexamethasone), or another anthracycline-containing combination chemotherapy regimen. Low-grade lymphomas were usually treated with a single-agent chlorambucil if symptomatic. Fifty-four patients received megavoltage radiotherapy. All patients were regularly followed-up with intervals of a few months in an outpatient department. All patients were observed over 5 years or until death. The median follow-up time was 86 months (range, 62 to 136 months). Eighty patients died during the follow-up time.
Venous blood samples.
Peripheral venous blood samples were collected in sterile test tubes a few hours or a few days before starting lymphoma therapy, centrifuged at 2,000g for 10 minutes, and then stored at −20°C.
S-bFGF immunoassay.
S-bFGF concentrations were determined as S-bFGF immunoreactivity using a quantitative sandwich enzyme immunoassay technique (Quantikine High Sensitivity Human FGF basic Immunoassay; R&D Systems, Minneapolis, MN). The system uses a solid-phase monoclonal and an enzyme-linked polyclonal antibody raised against recombinant human bFGF. For each analysis, 100 μL of serum was used. All analyses and calibrations were performed in duplicate. The calibrations on each microtiter plate included recombinant human bFGF standards. Optical densities were determined by using a microtiter plate reader (Multiscan RC Type 351; Labsystems, Helsinki, Finland) at 490 nm. The blank was subtracted from the duplicate readings for each standard and sample. A standard curve was created using StatView 4.02 (Abacus Concepts Inc, Berkeley, CA) by plotting the logarithm of the mean absorbance of each standard versus the logarithm of the bFGF concentration. Concentrations are reported as picograms per milliliter. When 20 serum samples were measured twice in the same assay, the intra-assay variation ranged from 0.0 to 0.9 pg/mL. When 20 serum samples were assayed twice in 2 separate assays, the interassay variation ranged from 0.0 to 1.0 pg/mL. No correlation was observed between S-bFGF concentration and the duration of the storage (P > .1, the Mann-Whitney test). Thus, there was no evidence of loss of bFGF on storage at −20°C.
Statistical analysis.
Statistical analysis was performed using StatView 4.02 (Abacus Concepts Inc). All P values are 2-tailed. The Mann-Whitney test and Kruskall-Wallis test were used to compare S-bFGF concentrations in different groups. Cumulative survival was computed according to the product-limit method of Kaplan-Meier from the date of diagnosis. The Wilcoxon test was used to compare survival of the different subgroups of patients. The relative importance of different variables on survival was studied using the Weibull multivariate model. The prognostic factors introduced in the model are commonly accepted and have been previously reported by the International Non-Hodgkin’s Lymphoma Prognostic Factors Project on a large series of patients.22
RESULTS
S-bFGF in patients at diagnosis.
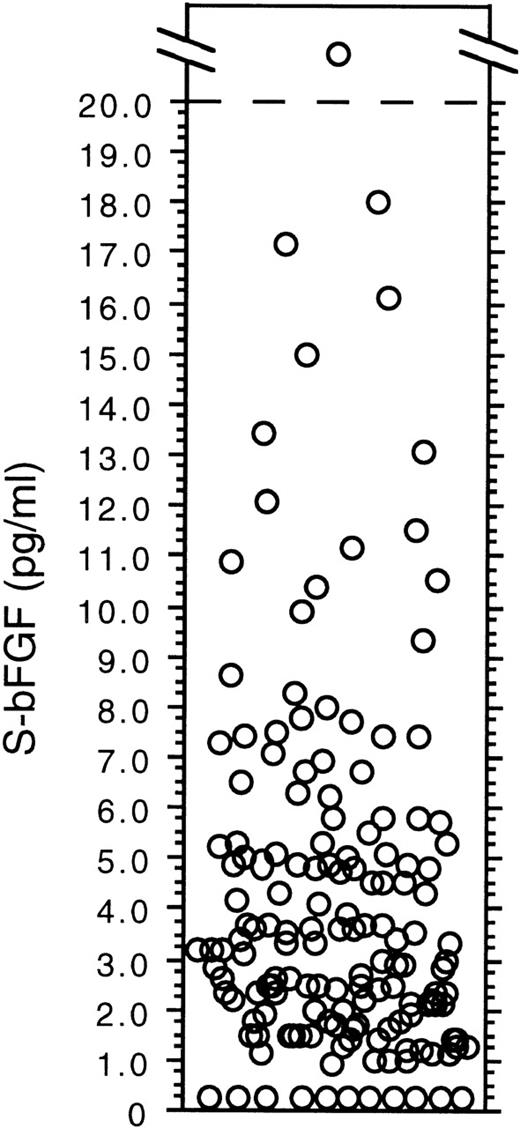
S-bFGF concentrations ranged from undetectable to 34.7 pg/mL (median, 3.3 pg/mL; mean, 4.3 pg/mL) among the 160 patients with NHL (Fig 1). One third of the patients had an S-bFGF of ≥4.8 pg/mL (the highest tertile), and one fourth had an S-bFGF of ≥5.5 pg/mL (the highest quartile).
Pretreatment serum concentrations of bFGF (in picograms per milliliter) in 160 patients with NHL.
Pretreatment serum concentrations of bFGF (in picograms per milliliter) in 160 patients with NHL.
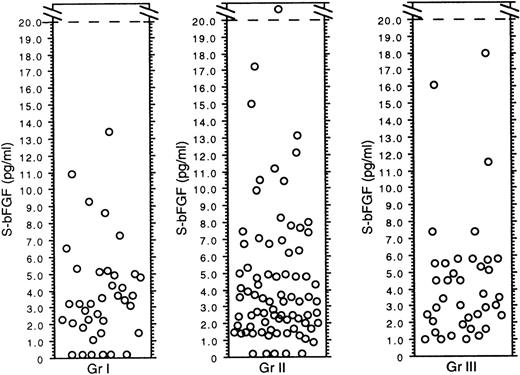
The serum concentrations of bFGF were comparable in the different histologic subtypes of NHL by the Working Formulation Scheme (P> .1 for all comparisons). There was no significant difference in the S-bFGF concentrations of patients with low-grade (median, 3.2 pg/mL; range, 0 to 13.4 pg/mL), intermediate-grade (median, 3.3 pg/mL; range, 0 to 34.7 pg/mL), or high-grade (median, 3.5 pg/mL; range, 1 to 18.0 pg/mL) lymphoma (tested I v II+III; P > .1; Fig 2). S-bFGF was not associated with age (tested > median ≤ 60 years of age), the World Health Organization (WHO) performance status (0-1 v 2-4), the serum lactate dehydrogenase (LDH) level measured at the time of the diagnosis (normalv abnormal), Ann Arbor stage (I-II v III-IV), the number of extranodal tumor sites (≤1 v >1), or the presence of B-symptoms (P > .1 for all comparisons). Because data from animal models suggest that the clearance of bFGF may take place through the kidney and the liver,23 24 we compared the patients’ S-bFGF levels with the results of kidney and liver function tests. However, the analyses of these data showed that S-bFGF levels were not elevated in the patients with high (>100 μmol/L) serum creatinine (median, 3.7 pg/mL [range, 0 to 18 pg/mL] v median, 3.0 pg/mL [range, 0 to 34.7 pg/mL] in patients with serum creatinine <100 μmol/L; P > .1). Similarly, patients with an elevated level of serum 5′-nucleotidase (>8 U/L) had S-bFGF concentrations comparable to those of the patients with normal serum 5′-nucleotidase (median, 3.7 pg/mL [range, 0 to 10.4 pg/mL]v median, 3.2 pg/mL [range, 0 to 34.7 pg/mL], respectively;P > .1).
Pretreatment serum concentrations of bFGF (in picograms per milliliter) in patients with NHL by the Working Formulation grade.
Pretreatment serum concentrations of bFGF (in picograms per milliliter) in patients with NHL by the Working Formulation grade.
S-bFGF and survival.
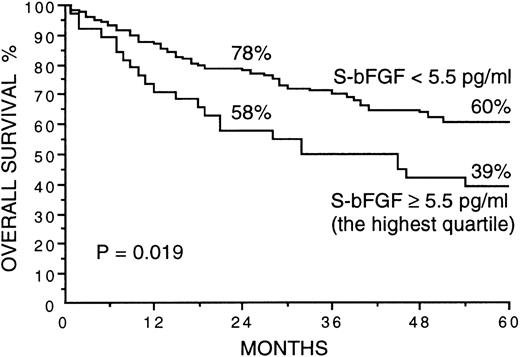
Several factors correlated strongly with overall survival in univariate survival analyses in the present series (Table 1). Patients with a high S-bFGF at diagnosis had inferior overall survival in comparison with those with lower pretreatment concentration of S-bFGF. The 2- and 5-year survival rates of the patients within the highest quartile of S-bFGF concentrations (S-bFGF ≥5.5 pg/mL) were only 58% and 39%, respectively, in contrast to the 78% and 60% 2- and 5-year survival rates of those patients with an S-bFGF concentration less than 5.5 pg/mL (P = .019; Fig 3 and Table1). Likewise, when other cut-off values were used, patients with higher S-bFGF concentrations had an inferior survival rate than those with lower S-bFGF. When the highest tertile (S-bFGF ≥4.8 pg/mL) and the median (3.3 pg/mL) of S-bFGF were used as cut-off values, the respective 5-year survival rates were 44% versus 60% (P = .068) and 49% versus 61% (P = .072; Table 1).
Prognostic Factors in Univariate Analyses
| Factor . | N . | 5-yr Survival (%) . | P . |
|---|---|---|---|
| Age at diagnosis (yr) | |||
| ≤60 | 85 | 67 | <.0001 |
| >60 | 75 | 41 | |
| WHO performance status | |||
| 0-1 | 132 | 63 | <.0001 |
| 2-4 | 28 | 14 | |
| Serum LDH at diagnosis | |||
| Normal | 115 | 64 | <.0001 |
| Abnormal | 45 | 33 | |
| Ann Arbor stage | |||
| I-II | 95 | 66 | .0001 |
| III-IV | 65 | 37 | |
| Presence of B-symptoms | |||
| No | 130 | 61 | .0001 |
| Yes | 30 | 23 | |
| No. of extranodal sites | |||
| 0-1 | 143 | 59 | .0036 |
| >1 | 17 | 29 | |
| Histologic grade | |||
| Low | 38 | 68 | .0067 |
| Intermediate or high | 118 | 52 | |
| S-bFGF at diagnosis | |||
| <5.5 pg/mL | 120 | 60 | .019 |
| ≥5.5 pg/mL (the highest quartile) | 40 | 39 | |
| <4.8 pg/mL | 107 | 60 | .068 |
| ≥4.8 pg/mL (the highest tertile) | 53 | 44 | |
| <3.3 5 pg/mL | 80 | 61 | .072 |
| ≥3.3 pg/mL (median) | 80 | 49 |
| Factor . | N . | 5-yr Survival (%) . | P . |
|---|---|---|---|
| Age at diagnosis (yr) | |||
| ≤60 | 85 | 67 | <.0001 |
| >60 | 75 | 41 | |
| WHO performance status | |||
| 0-1 | 132 | 63 | <.0001 |
| 2-4 | 28 | 14 | |
| Serum LDH at diagnosis | |||
| Normal | 115 | 64 | <.0001 |
| Abnormal | 45 | 33 | |
| Ann Arbor stage | |||
| I-II | 95 | 66 | .0001 |
| III-IV | 65 | 37 | |
| Presence of B-symptoms | |||
| No | 130 | 61 | .0001 |
| Yes | 30 | 23 | |
| No. of extranodal sites | |||
| 0-1 | 143 | 59 | .0036 |
| >1 | 17 | 29 | |
| Histologic grade | |||
| Low | 38 | 68 | .0067 |
| Intermediate or high | 118 | 52 | |
| S-bFGF at diagnosis | |||
| <5.5 pg/mL | 120 | 60 | .019 |
| ≥5.5 pg/mL (the highest quartile) | 40 | 39 | |
| <4.8 pg/mL | 107 | 60 | .068 |
| ≥4.8 pg/mL (the highest tertile) | 53 | 44 | |
| <3.3 5 pg/mL | 80 | 61 | .072 |
| ≥3.3 pg/mL (median) | 80 | 49 |
Overall survival of 160 patients with NHL by the pretreatment S-bFGF concentration. The highest quartile (5.5 pg/mL) was used as the cut-off value. Survival rates at 24 and 60 months are given.
Overall survival of 160 patients with NHL by the pretreatment S-bFGF concentration. The highest quartile (5.5 pg/mL) was used as the cut-off value. Survival rates at 24 and 60 months are given.
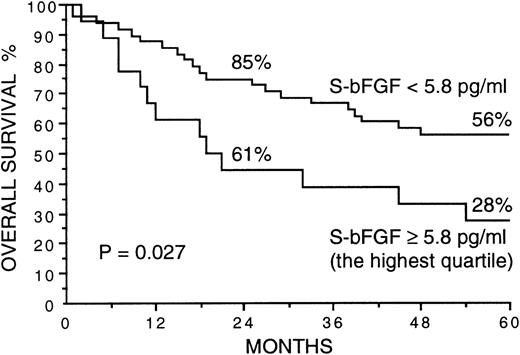
In patients with intermediate- or high-grade lymphoma (n = 118), the 2- and 5-year survival rates of the patients within the highest quartile of S-bFGF concentrations (S-bFGF ≥5.7 pg/mL) were only 50% and 37%, respectively, in contrast to the 73% and 57% 2- and 5-year survival rates of those patients with S-bFGF lower than the highest quartile (P = .033). Also, in the patients with a low-grade lymphoma (n = 38), the patients within the highest quartile of S-bFGF concentrations (S-bFGF ≥5.1 pg/mL) had an inferior survival rate in comparison with those with lower S-bFGF concentration (2- and 5-year survival rates of 89% and 56% v 97% and 72%, respectively), but the difference was not statistically significant (P > .1). The association between S-bFGF and survival was also studied separately in the subgroup of large-cell diffuse and immunoblastic lymphomas. This was the largest histologic subgroup (n = 66) within the present series. In the Revised European-American Classification of Lymphoid Neoplasms (REAL),25 the probable immunophenotypic equivalent of this group is the disease entity of diffuse large B-cell lymphomas. A high pretreatment serum concentration of bFGF was associated with poor overall survival also in the subgroup of large-cell diffuse and immunoblastic lymphomas. When the highest quartile of S-bFGF within the subgroup (S-bFGF ≥5.8 pg/mL) was used as the cut-off value, the patients within the highest quartile of S-bFGF had 2- and 5-year survival rates of 61% and 28%, respectively, in comparison to the 85% and 56% 2- and 5-year survival rates of patients with an S-bFGF less than 5.8 pg/mL (P = .027; Fig 4).
Overall survival of 66 patients with large-cell diffuse or immunoblastic lymphoma by the pretreatment S-bFGF concentration. The highest quartile (5.8 pg/mL) was used as the cut-off value. Survival rates at 24 and 60 months are given.
Overall survival of 66 patients with large-cell diffuse or immunoblastic lymphoma by the pretreatment S-bFGF concentration. The highest quartile (5.8 pg/mL) was used as the cut-off value. Survival rates at 24 and 60 months are given.
To find out if S-bFGF has an independent influence on survival, S-bFGF was entered to multivariate analyses together with the components of the IPI. First, the parameters were introduced in the multivariate model as discontinuous variables: S-bFGF (<5.5 v ≥5.5 pg/mL; the highest quartile), age (≤60 v >60), the WHO performance status (≤1 v >1), Ann Arbor stage (I-IIv III-IV), the number of extranodal tumor sites (≤1 v>1), and serum LDH at diagnosis (normal v abnormal). In addition, the parameters were also entered to the multivariate model as continuous variables. Multivariate analyses showed that S-bFGF was an independent prognostic factor, both when the highest quartile (5.5 pg/mL) was used as a cut-off value (P = .0079; relative risk, 2.0; 95% confidence interval [CI], 1.2 to 3.4) and when S-bFGF and the other parameters were entered to the model as continuous variables (P = .024; Table 2). In both of the multivariate analyses, S-bFGF had a stronger prognostic value than serum LDH at diagnosis and the number of extranodal tumor sites, which are currently included as components in the IPI (Table 2).
S-bFGF and the Components of the IPI in Multivariate Analyses
| Factor . | P . | β . | SE . | RR (eβ) . | 95% CI for RR . |
|---|---|---|---|---|---|
| WHO performance status | |||||
| 0-1v 2-4 | <.0001 | 1.21 | 0.29 | 3.35 | 1.92-5.87 |
| Continuous | <.0001 | ||||
| Age at diagnosis (yr) | |||||
| ≤60v >60 | <.0001 | 1.02 | 0.25 | 2.79 | 1.14-4.58 |
| Continuous | .0009 | ||||
| Ann Arbor stage | |||||
| I-IIv III-IV | .0019 | 0.80 | 0.26 | 2.23 | 1.33-3.72 |
| Continuous | .0028 | ||||
| S-bFGF at diagnosis | |||||
| <5.5v ≥5.5 pg/mL (the highest quartile) | .0079 | 0.70 | 0.27 | 2.02 | 1.20-3.42 |
| Continuous | .024 | ||||
| Serum LDH at diagnosis | |||||
| Normal v abnormal | .014 | 0.65 | 0.27 | 1.92 | 1.14-3.25 |
| Continuous | .74 | ||||
| No. of extranodal tumor sites | |||||
| ≤1 v >1 | .039 | 0.71 | 0.35 | 2.04 | 1.04-4.01 |
| Continuous | .35 |
| Factor . | P . | β . | SE . | RR (eβ) . | 95% CI for RR . |
|---|---|---|---|---|---|
| WHO performance status | |||||
| 0-1v 2-4 | <.0001 | 1.21 | 0.29 | 3.35 | 1.92-5.87 |
| Continuous | <.0001 | ||||
| Age at diagnosis (yr) | |||||
| ≤60v >60 | <.0001 | 1.02 | 0.25 | 2.79 | 1.14-4.58 |
| Continuous | .0009 | ||||
| Ann Arbor stage | |||||
| I-IIv III-IV | .0019 | 0.80 | 0.26 | 2.23 | 1.33-3.72 |
| Continuous | .0028 | ||||
| S-bFGF at diagnosis | |||||
| <5.5v ≥5.5 pg/mL (the highest quartile) | .0079 | 0.70 | 0.27 | 2.02 | 1.20-3.42 |
| Continuous | .024 | ||||
| Serum LDH at diagnosis | |||||
| Normal v abnormal | .014 | 0.65 | 0.27 | 1.92 | 1.14-3.25 |
| Continuous | .74 | ||||
| No. of extranodal tumor sites | |||||
| ≤1 v >1 | .039 | 0.71 | 0.35 | 2.04 | 1.04-4.01 |
| Continuous | .35 |
Abbreviations: β, estimated coefficient of the hazard function; SE, standard error; RR, relative risk.
DISCUSSION
It has been shown that solid tumors progress in concert with an induction of tumor angiogenesis. Recent data suggest that similar phenomenon occurs also in hematologic malignancies. When bone marrow biopsies from children with newly diagnosed, untreated acute lymphoblastic leukemia and from controls were evaluated, the biopsies from children with leukemia showed significantly higher microvessel densities, suggesting that leukemia cells induce angiogenesis in the bone marrow and that leukemia might be angiogenesis dependent.26 In NHLs, significantly higher microvesel counts have been found in high-grade lymphomas than in low-grade lymphomas, implying that angiogenesis occurring in NHLs increases with tumor progression.27,28 NHLs have been also found to express angiogenic molecules, including vascular endothelial growth factor (VEGF) and VEGF-C.29 30
In the present study, we could detect bFGF in the serum samples of most patients with NHL. A high pretreatment S-bFGF concentration was associated with poor overall survival. The 5-year survival rate of the patients within the highest quartile of S-bFGF concentrations (S-bFGF ≥5.5 pg/mL) was only 39%, in contrast to the 60% survival rate of the patients with a lower S-bFGF at diagnosis. Furthermore, S-bFGF concentration was an independent prognostic factor in multivariate analyses. In line with this, we found no associations between S-bFGF and any other clinicopathological variable studied. It should be noted that, in multivariate analyses, S-bFGF had a stronger prognostic value than the number of extranodal tumor sites and serum LDH at diagnosis, which both are currently included as components, together with stage, age, and the WHO performance status, in the IPI. Although first designed for aggressive NHLs, the IPI has subsequently been shown to be useful in all grades of lymphoma.31
The source of the elevated levels of bFGF in the serum samples of our patients remains unknown. Various lymphoblastoid and leukemic cell lines have been shown to secrete bFGF.32,33 In CLL, elevated intracellular levels of bFGF were found in the CLL cells, and a high intracellular bFGF level in the CLL cells was associated with a high stage of the disease.34 Peripheral blood mononuclear cells,35 T cells,36,37macrophages,38 and granulocytes39 also have the capacity to produce bFGF. In addition, the endothelial cells of blood vessels express bFGF.40 Consequently, it is possible that bFGF in sera of lymphoma patients is released mainly by malignant cells or by a combination of cancer cells and normal cells, including the endothelial cells and peripheral blood cells. S-bFGF may alternatively be produced by normal cells under deregulated stimulation by malignant cells. In a transgenic mouse fibrosarcoma model, there is a change in the localization of bFGF from its normal cell-associated state to extracellular release in the later stages of the multistep development of fibrosarcoma. This change was concomitant with the neovascularization seen in vivo. Thus, in this multistep tumorigenesis pathway, there appears to be a discrete switch to the angiogenic phenotype that correlates with the export of bFGF.11Interestingly, in a tumor-bearing mouse model, the origin of elevated bFGF levels in the urine was found to be almost exclusively from tumor cells.24 In agreement with this finding, intravenously administered bFGF has been found to be distributed preferentially to the kidneys and the liver.23
Angiogenic molecules other than bFGF have also been detected in the sera of cancer patients. Elevated serum concentrations of VEGF have been found to be associated with various unfavorable clinical parameters, including extensive disease17,41,42 and poor patient survival.43-45 In a series of 82 patients with NHL, patients with lower than the median serum concentration of VEGF (S-VEGF) at diagnosis had a 71% 5-year survival rate, in comparison to only 49% among those with an S-VEGF greater than the median (P= .01).43 Interestingly, a circulating form of human endostatin was recently identified,46 suggesting that various endogenous inhibitors of angiogenesis may also be found in the bloodstream. Furthermore, Sasaki et al47 found that the concentrations of soluble endostatin measured in serum samples of healthy human donors were similar to the concentrations that efficiently inhibit endothelial cell proliferation in vitro,48 suggesting that circulating forms of endostatin may be involved in the homeostatic control of angiogenesis. In the future, it might be possible to obtain an angiogenic profile of a blood sample by measuring the concentrations of several circulating stimulators and inhibitors of angiogenesis. The use of such an angogenic profile could perhaps be used as a monitor of cancer therapy or as a predictor of outcome after cancer has been diagnosed.
In conclusion, the results of the present study indicate that S-bFGF is elevated in a subgroup of patients with NHL and correlates with a poor outcome. Notably, the pretreatment S-bFGF surfaced as an independent prognostic variable in multivariate analyses, having a stronger predictive value than 2 of the components of the IPI. A high S-bFGF content may reflect active angiogenesis and lymphoma growth, and it is possible that similar associations with unfavorable survival can be found in other types of human cancer as well. Studies are now needed to find out if lymphoma therapy can be monitored by measuring bFGF concentrations in consecutive serum samples. It will be of particular interest to study if the clinical significance of S-bFGF could be further improved using an angiogenic profile obtained by measuring the serum concentrations of several circulating angiogenic and antiangiogenic molecules.
ACKNOWLEDGMENT
The authors thank Kati Konola for technical assistance.
Supported by grants from the Finnish Academy of Sciences, the Finnish Cancer Foundation, and the Helsinki University Central Hospital Research Funds.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. section 1734 solely to indicate this fact.
REFERENCES
Author notes
Address reprint requests to Petri Salven, MD, PhD, Department of Oncology, Helsinki University Central Hospital, PO Box 180, FIN-000290 HYKS, Finland; e-mail: petri.salven@helsinki.fi.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal