Abstract
The immunoglobulin on the surface of B-cell lymphomas can be a tumor-specific target for monoclonal antibody therapy. Between 1981 and 1993, 45 individuals with low grade B-cell lymphoma were treated with 52 courses of custom-made anti-idiotype antibodies. The antibodies were used either alone or in combination with -interferon, chlorambucil, or interleukin-2 (IL-2). The majority of these patients responded to treatment, with a 66% overall and 18% complete response rate. Six patients (13%) experienced prolonged complete remissions, five of which are ongoing from 4 to 10 years after therapy and are the subject of this report. We asked whether residual lymphoma could be found in these patients with prolonged remissions. We performed enzyme-linked immunosorbent assay (ELISA) assays for idiotype protein or anti-idiotype antibodies in serum. Blood and bone marrow samples were examined by flow cytometry for idiotype positive cells, and by polymerase chain reaction (PCR) for clonal gene rearrangements of immunoglobulin CDR3 sequences or t(14;18) translocations. Using these sensitive and specific tests it was possible to detect very low levels of residual lymphoma in five of these patients who had been in clinical remission for 3 to 8 years before this evaluation. These five have continued without recurrence for up to 3 years since. Thus, we have found a pattern of residual inactive disease in patients treated with anti-idiotype antibodies. The biology of follicular lymphoma evidently includes the potential for tumor dormancy after therapies with varied mechanisms of action, resulting in clinical inactivity for many years. Thus, long-term control of the disease is possible at a clinical level despite persistence of the malignant clone.
© 1998 by The American Society of Hematology.
MOST HUMAN LYMPHOMAS are derived from B lymphocytes, which express a cell surface immunoglobulin molecule.1 The immunoglobulin of each B cell is unique, containing two variable regions that normally serve as recognition sites for foreign antigens. These variable regions are formed by the rearrangement of the germ line immunoglobulin genes. This genetic rearrangement allows for the tremendous diversity of human immunoglobulins, a critical feature of the immune system. When a B cell undergoes malignant transformation, it creates a clonal population of cells, each of which expresses the same unique receptor,2or “idiotype”. Antibodies can be produced, which target the unique idiotype of each malignant clone (anti-idiotype antibodies).3 Soon after the introduction of hybridoma technology, we developed mouse monoclonal antibodies against the idiotypes expressed by B-cell lymphomas and used these antibodies in therapeutic trials. We have previously reported the results of these trials, where such monoclonal anti-idiotype antibodies were used alone or in combination with α-interferon, chlorambucil, or interleukin-2 (IL-2) as therapy for patients with B-cell lymphoma.1 4-7
In four different trials, 45 patients were treated with 52 courses of anti-idiotype monoclonal antibodies. Eight patients experienced complete tumor regression after therapy, and in six patients, these complete responses have lasted for prolonged periods. Because advanced stage low grade lymphomas are considered incurable, we wondered whether these patients with long-term remissions had detectable disease despite prolonged disease inactivity. Both the original tumor and idiotype specific monoclonal antibodies were available, and we developed assays for persistent disease using several different methodologies: (1) enzyme-linked immunosorbent assay (ELISA) for detection of circulating idiotype proteins or anti-idiotype antibodies; (2) flow cytometric analysis to identify clonal or idiotype expressing B cells; and (3) polymerase chain reaction (PCR) detection of either a t(14,18) translocation (where the bcl-2 proto-oncogene is juxtaposed with the immunoglobulin heavy chain) or a tumor-specific DNA sequence for the immunoglobulin receptor hypervariable region of the malignant clone (the third complementarity determining region, or CDR3). Over a span of 2 years, all six patients were seen and in five their complete responses were ongoing, confirmed repeatedly with radiographic scanning. All patients agreed to undergo bone marrow biopsy and aspiration and peripheral blood was collected.
In this report, we present an overview of the clinical trials and present our data on persistence of the malignant clone in the long-term responding patients. Our results suggest that these patients harbor low numbers of tumor cells identical to the original malignant clone, presumably persisting in a dormant state.
MATERIALS AND METHODS
Anti-Idiotype Monoclonal Antibody Therapy
Anti-idiotype antibodies were produced by methods previously described involving “rescue fusion” of malignant cells with a nonsecreting heterohybridoma (K6H6-B5), isolation of the rescued tumor-derived immunoglobulin, and production of rodent monoclonal antibodies.3 8 Therapeutic doses of these anti-idiotype antibodies were infused three times weekly over 2 to 6 weeks. Patients were treated with varying doses of antibody (ranging from 400 to 15,500 mg) dependent on availability of the therapeutic agents and clinical circumstances. In different trials patients received either anti-idiotypic antibody as a single agent or therapeutic combinations of antibody and immunomodulatory or chemotherapeutic agents.
Interferon.
Patients received α-interferon (12 × 106U/m2 intramuscularly) 2 hours before each antibody infusion. Dosing three times weekly continued after completion of all antibody infusions for a total of 8 weeks.4
Chlorambucil.
Patients received two courses of anti-idiotype antibody separated by 4 weeks. A single 5-day course of chemotherapy with chlorambucil (16 mg/m2/day) was given at the start of the second course of antibody.6
IL-2.
A continuous intravenous (IV) infusion of IL-2 (6 × 106 IU/m2/day) was given during the third week of a single course of anti-idiotype antibody.
Tumor Detection
Before evaluation for this study, all six patients who had experienced durable complete remissions as defined by radiologic procedures and marrow biopsies underwent repeat staging to confirm their remission status. To collect samples for this analysis, peripheral blood and bone marrow was collected at a single time point ranging from 3 to 14 years postantibody therapy for the following analyses. Further peripheral blood samples were collected and analyzed on subsequent visits, but bone marrow biopsies were not repeated. Sensitivities for each detection method were determined using sequential dilutions of malignant cells into normal lymphocytes from spleen or blood.
ELISA
Serum was assayed by ELISA both for tumor idiotype protein and anti-idiotype antibodies.5 For the detection of circulating idiotype, a sandwich ELISA was designed. Microtiter plates were coated with the available anti-idiotype antibodies. These were the same antibodies that had been used therapeutically. Sequential pretreatment and posttreatment serum samples were serially diluted into the precoated wells. Biotin-conjugated anti-idiotype antibodies were added after washing, and detection was performed using streptavidin-horseradish peroxidase (HRP) and 2,2′-Azino-di-[3-äthyl-benzthiazolinsulfonat (6)] (ABTS; Boehringer Mannheim, Indianapolis, IN). To assay for anti-idiotype antibodies, plates were coated with idiotype protein and sequential pretreatment and posttreatment serum samples were serially diluted into the precoated wells. For idiotype proteins with IgM constant regions, detection was performed with HRP-labeled goat antihuman IgG F(ab’)2 fragments (Southern Biotechnology Associates, Birmingham, AL). For IgG isotype idiotype proteins, detection was performed with both HRP-labeled goat antihuman IgM F(ab’)2 fragments (Southern Biotechnology Associates) and HRP-labeled goat antihuman kappa or lambda F(ab’)2 fragments (Biosource International, Inc, Camarillo, CA), specific for the alternate light chain from that present in the tumor idiotype. Plates were read on a Kinetic Microplate Reader (Molecular Devices, Menlo Park, CA) and an increase over baseline of at least two dilutions was required for positivity.
Mononuclear cells were isolated from peripheral blood and bone marrow aspirates by ficoll/hypaque centrifugation and the following analyses were performed.
Flow Cytometry
Cells from both peripheral blood and marrow were stained in two colors with the following fluorochrome conjugated reagents; goat antimouse gamma1 and gamma2 (negative controls), anti-LeuM3 and anti-LeuM9 (monocytes, macrophages, eosinophils, and granulocytes), anti-CD45 (total leukocytes), anti-CD3(T cells), anti-CD20 (B cells), anti-CD4 and CD8 (T cell subtypes), (all from Becton Dickinson Immunocytometry Systems, San Jose, CA); and antilambda and kappa Fab’2 fragments (Southern Biotechnology Associates). A two-step stain was performed with the anti-idiotype antibodies specific for each patient or an irrelevant anti-idiotype antibody, followed by phycoerythrin (PE)-labeled goat antimouse IgG (Southern Biotechnology Associates), and a second stain with fluorescein isothiocyanate (FITC)-labeled B1 (anti-CD20; Coulter Corp, Miami, FL).
Samples were analyzed using the Becton-Dickinson FACScan. Lymphocyte populations were characterized, including assessment for any possible clonality of B-cell immunoglobulins. Separate duplicate samples were analyzed gating for CD-20 positive cells (B cells), and 20 to 50,000 gated events were collected. These were then analyzed for anti-idiotype positivity, defined as a 1% increase over background binding of an irrelevent anti-idiotype antibody.
Chromosomal t(14,18) Translocation
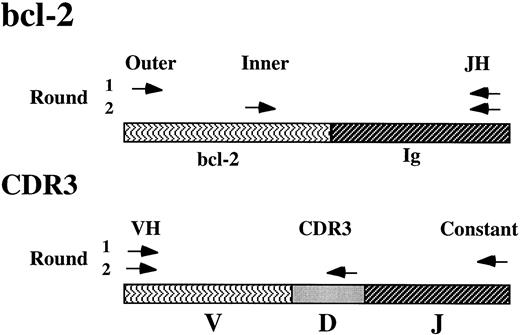
Genomic DNA was extracted from 1 × 107 cells using phenol/chloroform extraction and ethanol precipitation. DNA aliquots of 0.5 μg were used in a seminested PCR amplification using taqpolymerase (Gibco BRL, Gaithersburg, MD) and the following buffering conditions; 0.2 mmol/L deoxynucleotide triphosphates (dNTP), 1.5 mmol/L MgCl2, 20 mmol/L Tris-HCl (pH 8.4), and 50 mmol/L KCl. The first stage incorporated outer bcl-2 5′ primers from both major and minor breakpoint regions11,12 and a consensus J region 3′ primer amplified for 50 cycles (94°C for 45 seconds, 56°C for 45 seconds, and 72°C for 1 minute). A volume of 2.5 μL of the product was then subjected to a second 30 cycle amplification using the same cycling conditions and inner bcl-2 5′ primers from both major and minor breakpoint regions and the same consensus J region 3′ primer.11 12 Amplification products were identified after electrophoretic separation in 2% agarose containing ethidium bromide. DNA samples from the original malignant lymph node and normal peripheral blood lymphocytes were run as simultaneous controls. Clonal bands were sequenced to confirm the bcl-2 component. Each sample was run in six separate reactions to confirm results.
CDR3-Primed PCR Amplification
By sequencing cDNA of the immunoglobulin heavy chain gene from the six patients’ original tumor biopsies, the specific CDR3 sequence in the tumor immunoglobulin heavy chain gene was identified. A specific antisense CDR3 primer was synthesized. cDNA was made from 1 × 107 cells using RNAzol total RNA purification (TEL test “B”, Inc, Friendswood, TX), random hexamer priming and reverse transcriptase (Superscript II; Gibco BRL), and 5% by volume was taken for a seminested amplification using taqpolymerase (Gibco BRL) with buffering conditions optimized for each reaction (Opti-Prime, Stratagene, La Jolla, CA). VH leader and constant region primers were selected to recognize the immunoglobulin heavy chain gene from the malignant clone in the original lymph node biopsy. An initial 40-cycle amplification was performed using these primers and thermocycling conditions of 94°C, 56°C, and 72°C for 30 seconds each. A volume of 2.5 μL of the product was then subjected to a second 40-cycle amplification using the same VH leader 5′ primer and the specific CDR3 3′ primer. Buffer and annealing conditions for each set of primers were optimized for best amplification. Amplification products were identified after electrophoretic separation in 2% agarose containing ethidium bromide. DNA samples from the original malignant lymph node, blood mononuclear cells from normal subjects, and class-matched control tumors were run as simultaneous controls. Clonal bands were sequenced to confirm identity of the hypervariable regions. Each sample was run in six separate reactions to confirm results.13-15 A simultaneous amplification with β2-microglobulin primers was performed to confirm the quality of the cDNA preparation, and the reagent solution was amplified separately without template to detect possible contamination.
RESULTS
Anti-Idiotype Antibody Therapy and Clinical Outcome
Rodent monoclonal antibodies were custom-made against the idiotype expressed by each patient’s tumor. These antibodies were exquisitely specific, each of them failing to react with the idiotypes of several hundred unrelated lymphomas. The antibodies were infused intravenously, generally on a three times weekly schedule, in doses that were escalated within each patient to achieve sustained levels in serum of greater than 25 μg/mL. At this level of antibody, tissue penetration was documented to occur within lymph node and splenic sites. The cumulative doses ranged between 400 and 15,500 mg.
Several different trials were performed including: (1) antibody given alone3,7; (2) antibody together with α-interferon4; (3) antibody together with a single, short course of chlorambucil6; and (4) antibody together with IL-2 (unpublished results). All patients had progressive and evaluable disease at the time of antibody therapy. The initial clinical results of most of these trials have been described previously.4-6The treatments were well tolerated and no secondary or long-term toxicities have been identified.
The long-term results of these trials are summarized in Table 1. The different treatment regimens produced an overall response rate of 66% with 18% complete responses. The median survival from the time of treatment for all patients was 4.5 years. The average time from diagnosis to the beginning of antibody treatment was 5.6 years. The median survival from the time of original diagnosis is 11 years. Eight of the 52 treatments resulted in complete remissions after anti-idiotype antibody therapy. These complete remissions were documented by radiographic studies and bone marrow biopsies. Six of these eight responses have been durable (lasting more than 4 years), five are ongoing, and three patients have been in continuous remission for over 8 years. The clinical characteristics of all patients achieving complete remissions are described in Table 2. Patients are identified in chronological order of treatment. Tumor histologies cross a spectrum of low grade follicular lymphomas. All subjects had advanced stage disease, some with B symptoms. Durable responses occured after treatment with all treatment combinations.
Results of Therapeutic Trials Using Anti-Idiotype Antibodies
| Therapy . | Patients Treated . | PR . | CR . | CR Durations (years) . |
|---|---|---|---|---|
| Anti-Id | 18 | 8 | 4 | 1.5, 4+, 7,-150 9.5+ |
| Anti-Id + IFN | 12 | 7 | 2 | 9.5+, 10+ |
| Anti-Id + Chl | 13 | 8 | 1 | 2.5 |
| Anti-Id + IL-2 | 9 | 2 | 1 | 4.5 |
| Totals | 52 | 25 | 8 |
| Therapy . | Patients Treated . | PR . | CR . | CR Durations (years) . |
|---|---|---|---|---|
| Anti-Id | 18 | 8 | 4 | 1.5, 4+, 7,-150 9.5+ |
| Anti-Id + IFN | 12 | 7 | 2 | 9.5+, 10+ |
| Anti-Id + Chl | 13 | 8 | 1 | 2.5 |
| Anti-Id + IL-2 | 9 | 2 | 1 | 4.5 |
| Totals | 52 | 25 | 8 |
Antibodies were given either alone or in combination with other agents: IFN, alpha interferon; Chl, chlorambucil; IL-2, interleukin-2.
Abbreviations: PR, partial remission; CR, complete remission.
Patient 1 received local XRT after a local relapse at 7 years and subsequently has been in continuous and ongoing remission for an additional 9 years.
Characteristics of Patients Experiencing Complete Remission After Therapy With Anti-Idiotype Antibodies
| Patient . | Tumor Histology . | Stage . | Prior Therapy (Courses) . | Duration of Prior Remission (months) . | Treatment Regimens . | Dose (mg) . | Time Until Achievement of Best Response (months) . | DFS (years) . |
|---|---|---|---|---|---|---|---|---|
| 1 | FSC | IVB | IFN × 3 | 12 | Anti-id | 400 | 3 | 7* |
| CVP/B × 2 | XRT | |||||||
| 13 | FSC | IVB | Splenectomy | NA | Anti-id + IFN | 4,200 | 18 | 10+ |
| 14 | FSC | IVA | CVP × 2 | 4 | Anti-id + IFN | 8,030 | 8 | 9.5+ |
| Chl | ||||||||
| CVbP | ||||||||
| 17 | FM | IIIA | None | NA | Anti-id | 6,908 | 23 | 9.5+ |
| 24 | FSC | IVA | Chl × 2 | 4 | Anti-id + Chl | 3,840 | 17 | 2.5 |
| 34 | FSC | IVA | Chl | 4 | Anti-id + IL-2 | 7,792 | 3 | 4.5 |
| CVP | ||||||||
| 44 | F + DSC | IVA | CVP × 2 | 12 | Anti-id | 6,500 | 12 | 4.0+ |
| 45 | F + DM | IVA | CVP | 29 | Anti-id | 8,200 | 11 | 1.5 |
| Patient . | Tumor Histology . | Stage . | Prior Therapy (Courses) . | Duration of Prior Remission (months) . | Treatment Regimens . | Dose (mg) . | Time Until Achievement of Best Response (months) . | DFS (years) . |
|---|---|---|---|---|---|---|---|---|
| 1 | FSC | IVB | IFN × 3 | 12 | Anti-id | 400 | 3 | 7* |
| CVP/B × 2 | XRT | |||||||
| 13 | FSC | IVB | Splenectomy | NA | Anti-id + IFN | 4,200 | 18 | 10+ |
| 14 | FSC | IVA | CVP × 2 | 4 | Anti-id + IFN | 8,030 | 8 | 9.5+ |
| Chl | ||||||||
| CVbP | ||||||||
| 17 | FM | IIIA | None | NA | Anti-id | 6,908 | 23 | 9.5+ |
| 24 | FSC | IVA | Chl × 2 | 4 | Anti-id + Chl | 3,840 | 17 | 2.5 |
| 34 | FSC | IVA | Chl | 4 | Anti-id + IL-2 | 7,792 | 3 | 4.5 |
| CVP | ||||||||
| 44 | F + DSC | IVA | CVP × 2 | 12 | Anti-id | 6,500 | 12 | 4.0+ |
| 45 | F + DM | IVA | CVP | 29 | Anti-id | 8,200 | 11 | 1.5 |
The Disease Free Survival (DFS) is listed in the final column, with ongoing remissions printed in bold-faced type and notated with a + sign.
Abbreviations: Histologies: FSC, follicular small cleaved; FM, follicular mixed; F + DM, follicular and diffuse mixed; F + DSC, follicular and diffuse small cleaved; Therapies: IFN, alpha interferon; Chl, chlorambucil; C, cyclophosphamide; V, vincristine; Vb, vinblastine; P, prednisone; B, bleomycin; NA, these patients did not receive systemic therapy before trial entry.
Patient 1 received local XRT after a local relapse at 7 years and subsequently has been in continuous and ongoing remission for an additional 9 years.
Several of the case histories are particularly interesting.
Patient no. 1 was initially treated with anti-idiotype antibodies in 1981 for stage IV disease.3 He experienced complete regression of all tumor, even though pretreatment disease included bone marrow involvement, extensive lymphadenopathy, and hepatosplenomegaly with individual retroperitoneal masses measuring up to 4 cm. He continued without evidence of disease for 7 years, at which time he required coronary artery bypass grafting for atherosclerotic heart disease. A localized skin recurrence of his lymphoma was identified after an infection at the saphenous vein harvest site. A small field, which included his ankle and distal lower leg, was treated with local irradiation and no systemic therapy was given. He has been in continuous remission for an additional 9 years.
Patient no. 14 was treated with a monoclonal anti-idiotype antibody that bound to 100% of malignant cells in the original lymph node biopsy. He had a good initial response to treatment, but developed tumor regrowth after 3 months. The relapsed malignant cells were no longer recognized by the primary antibody. A second anti-idiotype antibody bound to 85% of the relapsed tumor and was given in a second therapeutic course. He responded with complete regression of all lymphoma and has been in continuous remission for over 10 years.
Tumor Detection in Patients With Long-Term Remissions
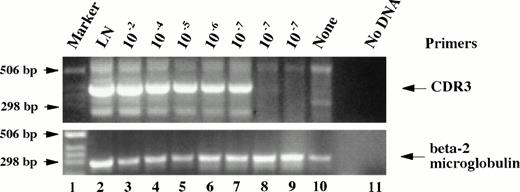
We performed an analysis for residual disease in the patients who have experienced long-term complete remissions. Several different tests were performed to detect the presence of tumor cells. The tests and their sensitivities are shown in Table 3. PCR analysis is known to be exquisitely sensitive. We performed two different seminested PCR amplification assays to determine whether tumor-specific DNA sequences were present in the collected samples. The seminested strategy is described in Fig 1. The bcl-2 assay, which is performed on genomic DNA, can detect 1 rearranged genome in 105 normal cells.11,16,17 The CDR3 assay we performed uses cDNA as its initial template. Thus, multiple copies of the targeted message may be present in each malignant cell, allowing for even greater sensitivity.18 Results of the CDR3-primed amplification performed on serially diluted samples of tumor cells in normal peripheral blood lymphocytes are shown in Fig 2, lanes 7, 8, and 9 and represent three separate cDNA preparations at the greatest dilution (one malignant cell in 107 lymphocytes). One sample shows amplification, indicating the limit of detection. Separate dilution curves were performed for the other patients’ tumors with similar results, suggesting that with multiple sample runs we could reliably detect one malignant cell in 107 normal cells. It should be noted that in this assay, identity of residual tumor with the pretreatment biopsy is confirmed by binding of the CDR3 primer and by sequencing of the remaining heavy chain variable region. The sequence of the CDR3 region in the amplified residual tumor is defined by the primers used in the amplification and not by the actual CDR3 sequence of the residual lymphoma.
Sensitivies of Detection Assays Used to Identify Residual Tumor
| Detection Method . | Sample Source . | Sensitivity . |
|---|---|---|
| Histology | Bone marrow biopsy | 1 in 20 cells |
| ELISA | Serum | 0.1 μg/mL |
| FACS | PBL and BM | 1 in 104 cells |
| Genomic PCR (bcl-2) | PBL and BM | 1 in 105 cells |
| RT-PCR (CDR3) | PBL and BM | 1 in 107 cells |
| Detection Method . | Sample Source . | Sensitivity . |
|---|---|---|
| Histology | Bone marrow biopsy | 1 in 20 cells |
| ELISA | Serum | 0.1 μg/mL |
| FACS | PBL and BM | 1 in 104 cells |
| Genomic PCR (bcl-2) | PBL and BM | 1 in 105 cells |
| RT-PCR (CDR3) | PBL and BM | 1 in 107 cells |
Abbreviations: PBL, peripheral blood lymphocytes; BM, bone marrow.
An agarose gel showing the calibration of sensitivity for the seminested CDR3 PCR amplification. The amplification product has a length of approximately 350 bp. Cells from the malignant lymph node (which contained 80% tumor cells) were serially diluted into normal spleen cells down to 1 abnormal cell in 107 splenocytes. Three separate dilutions of 1 in 107 were tested. Normal spleen and no DNA controls are included. At the bottom are shown the same cDNA preparations amplified with beta-2 microglobulin primers as a control for quality of the cDNA and for gel loading.
An agarose gel showing the calibration of sensitivity for the seminested CDR3 PCR amplification. The amplification product has a length of approximately 350 bp. Cells from the malignant lymph node (which contained 80% tumor cells) were serially diluted into normal spleen cells down to 1 abnormal cell in 107 splenocytes. Three separate dilutions of 1 in 107 were tested. Normal spleen and no DNA controls are included. At the bottom are shown the same cDNA preparations amplified with beta-2 microglobulin primers as a control for quality of the cDNA and for gel loading.
The combined results of the tumor detection assays are summarized in Table 4. None of the patients had tumor detectable by ELISA or flow cytometry. Patient no. 34 was the only patient with a complete response to antibody therapy who relapsed during the course of this analysis. The bone marrow biopsy performed for this analysis contained lymphoid aggregates suspicious for lymphoma. A bone marrow biopsy performed 4 years before, at the initial confirmation of complete response, had been negative. The PCR analyses of both blood and bone marrow from this patient had detectable tumor-specific sequences. This patient has subsequently developed progressive but indolent lymphadenopathy at 4.5 years postantibody treatment.
Results of Detection Assays for Residual Lymphoma
| Patient . | BM Histology . | ELISA . | FACS . | bcl-2 . | CDR3 . |
|---|---|---|---|---|---|
| 1 | − | − | − | BM | BM + PB |
| 13 | − | − | − | BM + PB | BM |
| 14 | − | − | − | — | BM + PB |
| 17 | − | − | − | BM | PB |
| 34 | + | − | − | BM + PB | PB |
| 44 | − | − | − | NA | — |
| Patient . | BM Histology . | ELISA . | FACS . | bcl-2 . | CDR3 . |
|---|---|---|---|---|---|
| 1 | − | − | − | BM | BM + PB |
| 13 | − | − | − | BM + PB | BM |
| 14 | − | − | − | — | BM + PB |
| 17 | − | − | − | BM | PB |
| 34 | + | − | − | BM + PB | PB |
| 44 | − | − | − | NA | — |
Positive results identified by: BM, bone marrow; PB, peripheral blood.
Abbreviation: NA, this assay is not applicable to this patient.
Patient no. 1, the patient furthest out from anti-idiotypic antibody treatment, had residual tumor detectable by PCR analysis, in marrow by bcl-2, and both marrow and peripheral blood by CDR3 amplification. Patient no. 13 also had disease detectable by molecular methods in both peripheral blood and marrow. Patient no. 14 had disease detectable in both marrow and blood only by the most sensitive CDR3 assay. Patient no. 17 had PCR detectable disease in bone marrow by bcl-2 and peripheral blood by CDR3. We were unable to identify residual disease by any tests in patient no. 44. However, this patient’s original tumor did not contain an amplifiable bcl-2 translocation, making this PCR assay inapplicable. All PCR products, which implied residual disease, were subjected to nucleic acid sequencing and confirmed to have identity with the original tumor (either containing an identical breakpoint for the bcl-2 rearrangement or expressing the same variable region in the immunoglobulin heavy chain gene).
All together, five of the six patients had detectable residual tumor sequences using the sensitive and specific PCR tests. In all five cases, the tumor was found in both peripheral blood and bone marrow. These patients have all been followed for over 2 years since identification of residual disease and, with the exception of patient no. 34, all have continued in remission without any further therapy.
DISCUSSION
Throughout the 14-year time span during which these clinical trials were performed, it was apparent that a significant subpopulation of patients achieved marked reduction in tumor burden after infusions of anti-idiotype antibodies. Some of these responses were quite dramatic. The mechanism of this effect most likely involves the ability of anti-idiotypic antibodies to cross-link tumor immunoglobulin receptors. It has been shown that this cross-linking results in increased tyrosine phosphorylation,19 a preliminary step in a cascade of events that leads to cell death.20-23 This form of activation-induced cell death can also be triggered by cross-linking surface immunoglobulin molecules by multivalent surrogate peptide antigens.24 The ability of the anti-idiotype antibodies to stimulate tyrosine phosphorylation within tumor samples was shown to correlate with their ability to induce tumor regression.6
In six of the 45 patients treated on these protocols, a durable disease-free remission was precipitated by the antibody therapy. All had experienced significant disease growth before the antibody treatments. The duration of these six responses remains unexplained. A cascade of signal transduction leading to apoptosis may explain their initial responses, but remissions lasting for years after this induction event require other explanations. For patients who experienced complete tumor regression, the time until they achieved a disease-free status ranged from 3 to 23 months. This slow tumor involution is not consistent with simultaneous apoptosis of all malignant cells. Dormancy of lymphomas has been described in animal models after immune therapy. Uhr et al25 have documented that idiotypic vaccines can halt tumor cell cycling, possibly through an autologous anti-idiotypic antibody mechanism.26-29 Their model suggests that this is mediated through surface immunoglobulin cross-linking,26,27,30 the same mechanism of action implicated in our clinical results. However, in their model, the continued presence of anti-idiotype antibodies is required for the maintenance of tumor dormancy. Early relapses may occur because the tumor becomes resistant to the effects of the antibody, but once the antibodies are cleared from the animal, the tumor recurs in most of their animals.29 Clearly, this mechanism cannot fully explain the continuing remissions in our patients, which can last over 10 years, long after all of the xenotypic antibodies were cleared from their bodies. Moreover, we were unable to identify any endogenous humoral anti-idiotype response in these six patients.
Several discrepancies in our results are revealing with respect to the accuracy of the molecular tests. In patient no. 17, the most sensitive test, the CDR3-primed PCR amplification, was positive only in peripheral blood and not in the bone marrow. It might have been expected that marrow samples would always be positive if the blood were positive, considering that low grade lymphoma is often identified microscopically in marrow without identifiable malignant cells circulating in peripheral blood, and that marrow aspirates often contain peripheral blood cells.17 This may represent the sampling error inherent in bone marrow biopsy and aspiration, as the disease is present in a patchy distribution. The analysis of patient no. 34 showed histologic evidence of lymphoma in bone marrow, but it is notable that his marrow did not have tumor cells detectable by fluorescence-activated cell sorting (FACS) analysis with fluorescent-labeled anti-idiotype antibodies. He did have tumor recognized by the specific CDR3 cDNA primer in his peripheral blood, but it is possible that the tumor in his marrow had mutated its idiotype to such a degree that it was no longer recognized by the anti-idiotype antibodies used in the FACS assay or our CDR3 primer. Tumor cells circulating in peripheral blood still contained a CDR3 region that annealed with our specific primer. His case exemplifies the fact that detectable residual disease can be followed by disease progression.
The different analyses defined in Table 3 serve to provide a quantitative analysis for residual disease in each patient. With the exception of patient no. 34, who had microscopic disease, no patient had detectable tumor by tests with sensitivities of up to 1 malignant cell in 104 normal cells. Four of the remaining five patients did have disease detectable by assays with sensitivities of up to 1 in 107 normal cells, confirming that the tumor burden in these patients is extremely low.
Four of five patients with ongoing complete remissions had molecular evidence of residual disease despite having shown no sign of clinical disease activity for up to 10 years. Within this time frame one would expect some sign of progressive disease if the tumor clone were proliferating. Other investigators have been able to correlate persistent disease, as identified by molecular detection, with poorer prognosis and worse treatment outcomes after standard and aggressive interventions including high-dose therapy requiring stem cell rescue.31 A correlation between more intensive intervention and higher molecular remission rates has been found.32 By contrast, other studies have shown that persistent tumor-related DNA sequences from indolent low grade lymphomas and aggressive acute leukemias may be detectable for prolonged periods without evidence of clinical relapse after a variety of therapies including chemotherapy, local and total lymphatic irradiation, and high-dose therapy with stem cell rescue.16,33-35 The prognostic relevence of the PCR assay for bcl-2 rearrangements has further been questioned by the finding that normal subjects have rare cells harboring such rearrangements in tonsil36 or in peripheral blood.37 38
The immunoglobulin heavy chain variable region cDNA sequences obtained from our CDR3 assay showed clonal relatedness with the parental tumors, but also reflected the expected point mutations that are seen over time in B-cell malignancies.39 The average point mutation rate was 2.7% in variable region fragments comparing pretreatment and residual posttreatment sequences. This is consistent with the expected mutation rate and argues against assay contamination of residual tumor cDNA by pretreatment tumor immunoglobulin cDNA.
It must be noted that the PCR-based tests are actually detecting tumor-related DNA sequences, and it is possible that the assays identify a “premalignant” cell that contains the genomic rearrangements present in the fully malignant lymphoma. The exact point at which a B cell becomes malignant has not been defined, and it is quite possible that cells containing a specific bcl-2 rearrangement or CDR3 sequence could persist, but do not have the ability to form tumors.
Because it is difficult to find accurate and timely endpoints in studies evaluating new therapies for low grade lymphoma, there is currently an interest in the use of these extremely sensitive PCR tests as surrogate endpoints in clinical trials. Conversion to molecular negativity may certainly support a profound reduction in tumor burden, but as others have shown and we confirm here, persistent positivity may still be followed by prolonged remission. We conclude, therefore, that such highly sensitive tests cannot replace clinical outcome in the analysis of new therapies for low grade B-cell lymphomas.
The tenuous nature of dormancy in low grade lymphomas is well documented in the disease course described for patient no. 1. Seven years after systemic therapy with anti-idiotypic antibodies, he experienced a localized disease recurrence precipitated by cardiac surgery and a localized infection. With control of this infection and localized therapy, his disease regressed completely and has been dormant since. The growth of lymphoma can be affected by infection, or cytokines released as a consequence of infection. The underlying mechanism is not understood.
The overall results from the anti-idiotypic antibody trials remain positive on long-term follow-up, but the practical limitations of producing individual therapeutic monoclonal anti-idiotype antibodies for each patient using hybridoma technology are prohibitive. It is conceivable that newer technologies such as phage display antibody or peptide libraries would make this therapy feasible. As an alternative approach, which still targets the unique receptor on each tumor, we have immunized patients against their own receptors.40-42One advantage is that smaller quantities of material are adequate to stimulate an active immune response, which may similarly result in dormant tumor or eliminate the malignant clone. Moreover, this vaccine approach results in the stimulation of an immune response against multiple epitopes of the idiotype molecule, therefore reducing the chance of mutational escape. Once an immune response is triggered, prolonged immunity may be achieved. The advantage of using a target which is absolutely tumor specific remains appealing, even though the approach requires a customized product for each patient. We anticipate that the beneficial effects in patients41 42 will motivate further innovations in technology.
Supported in part by Grant No. CA33399 from the National Institutes of Health, Bethesda, MD. T.A.D. was a Lymphoma Research Foundation Award recipient and is supported by a Clinical Associate Physician Award from the General Clinical Research Centers of the National Institutes of Health. R.L. is an American Cancer Society Clinical Research Professor.
Address reprint requests to Ronald Levy, MD, Stanford University, Department of Medicine, Division of Oncology, SUMC M207, Stanford, CA 94305-5306.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal