Abstract
Src family kinases play a key role in mitogenesis. The exquisitely tissue-specific distribution of different Src family members suggests that a fine tuning of their expression might be a key prerequisite for cell homeostasis. We tested B cells from patients affected by B-cell chronic lymphocytic leukemia (B-CLL) for expression of Src family kinases. The T-cell–specific tyrosine kinase Lck was found to be expressed at significant levels in CLL B-cells. This finding could be accounted for either by ectopic expression of Lck in B-CLL or by specific expression of this kinase in normal B-1 cells, which are believed to be the normal counterpart of CLL B cells. To answer this question B cells from different sources, characterized by a different size of the B-1 subpopulation, were tested for Lck expression. The results show that Lck expression is a feature of CD5+, B-1 cells, suggesting a potential role for Lck in the self-renewal capacity of this B-cell subpopulation and supporting the notion that B-1 cells are the subset undergoing oncogenic transformation in B-CLL. Furthermore, we show that the CD5−, B-2 subpopulation, while normally lacking Lck expression, acquires the capacity to express Lck ectopically upon transformation by EBV.
B-CELL CHRONIC lymphocytic leukemia (B-CLL) is the most common form of leukemia in white adults in Western countries, where it accounts for about 9% of all cancers and for about 30% of all leukemias.1 A characteristic feature of CLL B cells is the expression of CD5, a 67-kD antigen formerly considered an antigen restricted to T cells, which is also found on a limited subset of normal B cells.2,3 These normal CD5+ B cells, designated B-1,4 represent a self-replenishing population arising early in ontogeny in both mice and humans and are normally present in fetal tissue, whereas their distribution in the adult is limited essentially to the peritoneal cavity and to the mantle zone of lymph nodes.2-4 Although conventional B cells (B-2) can be induced to express CD5 in response to activation,5evidence accumulated primarily in mice strongly supports the notion that B-1 and B-2 cells are derived from separate lineages of progenitor cells.6,7 In addition to surface marker expression, B-1 cells indeed display unique features as compared to B-2 cells, including the capacity of self-renewal and a restricted antibody repertoire, with a bias toward the production of polyreactive, low-affinity autoantibodies.8 Furthermore, constitutive nuclear expression of STAT3 was recently shown to be a distinctive feature of B-1 cells.9
Because of their surface expression of CD5, CLL B cells are believed to be the tumoral counterpart of normal B-1 cells. However, although some unifying features can be found between normal B-1 cells and CLL B cells, such as the production of polyreactive autoantibodies, the ability to form rosettes with mouse erythrocytes and the expression of myelomonocytic antigens,10 the differences are too significant to unambiguously mark B-1 cells as the target of the transforming events leading to B-CLL. For example, as opposed to normal B-1 cells, CLL B cells accumulate in the G0 phase of the cell cycle and express low to undetectable levels of surface immunoglobulins.10 Furthermore, they are characterized by a defective signal transduction in response to B-cell antigen receptor triggering, resulting in a reduced proliferative response.10-13 Thus, the precise relationship of the CLL B-cell to normal B-cell ontogeny is still incompletely understood.
Src family protein tyrosine kinases (PTK) play a key role in cell homeostasis. Although the mode of regulation is identical for different family members, the tissue distribution is remarkably specific,14 suggesting that an altered balance in the levels of Src family kinases, either qualitative or quantitative, might have profound effects on cell proliferation and survival. While the outcome of ectopic expression of Src family PTKs has to date not been investigated, dramatic effects of the overexpression of specific family members have been reported. In this respect, the best-characterized Src family PTK is Lck, which is normally specifically expressed in the T-cell lineage.15 When overexpressed in thymocytes, Lck induces thymic tumorigenesis.16
This report shows that Lck is expressed in both B-CLL and normal B-1 cells but not in conventional, B-2 cells. This result supports the hypothesis of separate B-1 and B-2 cell lineages in humans and provides evidence toward the concept of B-1 cells as the target of the transforming event leading to B-CLL. Furthermore, it suggests a role for Lck in B-1 cells. We also show that, although undetectable in peripheral blood B cells from healthy donors, Lck is expressed in B-2 cells from the same individuals following transformation by Epstein-Barr virus (EBV), suggesting that induction of ectopic Lck expression in B-2 cells by EBV might play a role in transformation.
MATERIALS AND METHODS
Patients, purification of lymphocyte populations, and flow cytometry.
Blood samples were obtained from 33 patients who satisfied diagnostic criteria for B-CLL,1 as well as from two patients diagnosed for hairy cell leukemia (HCL) and two patients diagnosed as having non-Hodgkin's lymphoma (NHL) in the leukemic phase. The patients had not received any treatment for at least 6 months before blood sampling. Two independent samples were taken from most patients. Peripheral blood from healthy donors was used as a control. Cord blood and peripheral blood mononuclear cells were isolated from whole blood by density centrifugation on Ficoll-Paque (Pharmacia, Uppsala, Sweden). After removal of macrophages by adherence to plastic, B cells were purified by a double step of rosetting with sheep erythrocytes. Lymphocytes from adenoid and spleen were recovered by disaggregation, followed by rosetting as described above. The purity of B-cell and T-cell populations was checked by flow cytometry using fluorochrome-conjugated monoclonal antibodies (MoAbs) to CD19 and CD3, respectively (Becton Dickinson, San Jose, CA). Purification of the CD5− and CD5+ subpopulations from cord blood B cells was carried out by fluorescence-activated cell sorter (FACS) sorting using fluorochrome-conjugated anti-CD19 MoAbs (Becton Dickinson) and the anti-CD5 MoAb B36.1,17 followed by a fluorochrome-conjugated anti-mouse Ig. Alternatively, the CD5− and CD5+ subpopulations from cord blood B cells were purified by immunomagnetic sorting using anti-CD5 MoAb and magnetic beads conjugated with anti-mouse Ig (Dynal Corp., Oslo, Norway). The purity of these populations was checked by flow cytometry, using the same anti-CD5 MoAb, followed by FITC-conjugated anti-mouse Ig (Life Technologies Italia srl, Milan, Italy). B-cell activation was carried out by incubating purified B cells on plastic wells precoated with anti-human μ chain antibodies (Cappel Laboratories, Durham, NC) for 12, 24, 48, or 72 hours. The activation was checked by a [3H]-TdR proliferation assay on a sample of the same B-cell population activated in the same conditions for 48 hours. Flow cytometric analysis of CD5 expression in these activated B cells showed that, beginning at 24 hours after activation, the proportion of CD5+ B cells was increased on the average by a factor of 1.5. The tumor cell lines, all obtained from American Type Culture Collection (ATCC) (Rockville, MD), included the EBNA+ B-cell lines Daudi, Raji, and RPMI-1788, the epidermoid line A431, the neuronal line PC12 and the monocytic line THP-1. EBV lymphoblastoid B-cell lines were obtained from peripheral blood B cells of healthy donors by transformation with EBV, using standard procedures.
Immunoblots and in vitro kinase assays.
When required cells were activated by treatment with the anti-CD5 MoAb B36.117 as described.18 Purified B cells and T cells were lysed at about 106 cells/10 μL in 1% Nonidet P-40 in 20 mmol/L Tris, pH 8, 150 mmol/L NaCl in the presence of 0.2 mg/mL Na orthovanadate, 1 μg/mL leupeptin, aprotinin, and pepstatin and 10 mmol/L phenyl methyl sulfonyl fluoride (PMSF) (Boehringer, Mannheim, Germany). The concentration of total proteins in postnuclear supernatants was determined using a kit from Pierce (Rockford, IL) and albumin as a standard. Equal amounts of proteins were subjected to sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) on 12% gels, transferred to nitrocellulose filters, and probed by immunoblot using the following MoAbs: anti-Lck, anti-Lyn, and anti-Fyn (Transduction Laboratories, Mamhead, UK), and anti-β-tubulin (Amersham, Buckinghamshire, UK). Peroxidase-labeled secondary antibodies were revealed by chemiluminescence using reagents from Pierce. To rule out a cross-reaction of the anti-Lck MoAb with other known members of the Src family tyrosine kinases expressed in lymphocytes, lysates of Jurkat T cells and of EBV transformed B cells were tested by immunoblot with MoAbs to Fyn and Lyn. While an Lck immunoreactive band could be detected in both types of cells, Fyn expression was restricted to T cells, whereas Lyn expression was restricted to B cells. Furthermore, no cross-reaction could be detected in a Fyn-specific immunoprecipitate probed by Western blot with the anti-Lck MoAb (Fig 1 and data not shown).
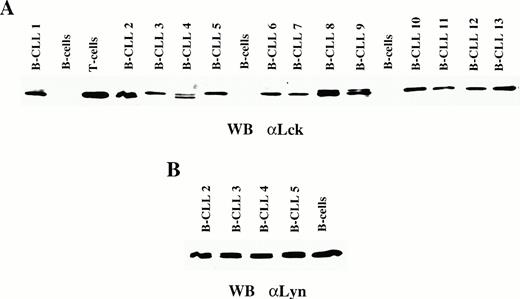
Expression of Lck in B-CLL. (A) Immunoblot analysis using an anti-Lck MoAb of peripheral blood B-cell lysates from healthy controls and from representative B-CLL patients. A lysate from normal T cells is included as a positive control. (B) Immunoblot analysis using an anti-Lyn MoAb of peripheral blood B-cell lysates from a healthy control and from representative B-CLL patients.
Expression of Lck in B-CLL. (A) Immunoblot analysis using an anti-Lck MoAb of peripheral blood B-cell lysates from healthy controls and from representative B-CLL patients. A lysate from normal T cells is included as a positive control. (B) Immunoblot analysis using an anti-Lyn MoAb of peripheral blood B-cell lysates from a healthy control and from representative B-CLL patients.
Lck was immunoprecipitated from postnuclear supernatants of 106 cells, using a polyclonal anti-Lck antiserum (Upstate Biotechnology, Lake Placid, NY) and protein A-Sepharose (Pharmacia) as described.18 Lck-specific immunoprecipitates were washed three times in lysis buffer and resuspended in 1× kinase buffer containing 20 mmol/L Tris pH 7.2, 10 mmol/L MgCl2, 10 mmol/L MnCl2, 5 μmol/L ATP, 10 μg acid-denatured enolase, and 10 μCi [32P]-γATP per sample.32P-labeled proteins were resolved by SDS-PAGE and visualized and quantitated using a Phosphorimager (Molecular Dynamics, Sunnyvale, CA). Titration of the levels of Lck recovered from increasing amounts of a control Jurkat T-cell lysate by immunoprecipitation with a fixed amount of the anti-Lck polyclonal antiserum was carried out by Western blot, using the anti-Lck MoAb. The results showed that Lck was quantitatively recovered in these conditions (data not shown).
Reverse transcriptase-polymerase chain reaction.
Total RNA was extracted in guanidinium isothiocyanate from 107 CLL B cells, or from the same number of EBV-transformed B cells. Jurkat T-cell RNA was used as a control. mRNA was affinity-purified from 30 μg total RNA, using oligo-dT cellulose (Boehringer), and an Lck specific first-strand cDNA was generated using an oligonucleotide complementary to positions 1563 to 1578 of human Lck mRNA (5′-AGGCTGAGGCTGGTA-3′) and AMV reverse transcriptase (Boehringer), according to the manufacturer's instructions. A 570-bp fragment spanning positions 55 to 624 of human Lck mRNA was amplified by polymerase chain reaction (PCR) in an Eppendorf Mastercycler 5330 temperature cycler using Taq polymerase (Boehringer) with the following primers: 5′-GGCTGTGGCTGCAGC-3′ and 5′-CCACCACCTCTCCCTG-3′. Positive controls included the product of a reverse transcriptase (RT)-PCR carried out on mRNA from Jurkat T cells, as well as the product of a PCR reaction carried out on Lck cDNA cloned in a plasmid vector. A negative control reaction was set up using mRNA extracted from the monocytic line THP-1. The amplification products were separated by electrophoresis on 2% agarose gels and subsequently transferred to nitrocellulose and hybridized with a 32P-labeled human Lck probe prepared by random priming from a pGEX-Lck plasmid construct (M. Boncristiano and C.T. Baldari, unpublished). The 1-kB-ladder molecular weight marker was purchased from Life Technologies Italia srl.
RESULTS
Expression of Lck in B cells from B-CLL patients.
Src family kinases play a key role in mitogenesis.14,15 As opposed to the broad distribution of Src, other members of this family of PTKs show a distinct cell type specificity. In lymphocytes, Lck and Fyn are specifically expressed in T cells, whereas Lyn is found predominantly in B cells.14 We hypothesized that ectopic expression of an Src family kinase could underlie the acquisition of an altered proliferative potential in leukemia. To test this possibility, we analyzed B cells from 33 B-CLL patients for the presence of Lck. Lysates of purified B cells from peripheral blood of B-CLL patients, as well as of control peripheral blood B cells from healthy donors, were subjected to immunoblot analysis using an anti-Lck MoAb. The results of 13 representative patients are presented in Fig 1. While no Lck could be detected in normal peripheral blood B cells, significant amounts of Lck were found in B cells from all B-CLL patients (Fig 1A and data not shown). The levels of Lck were variable; however, they were always lower as compared to control T cells (Fig 1A). These differences were confirmed by reprobing the stripped filters with an anti-tubulin MoAb (data not shown). In some patients, an Lck immunoreactive band characterized by a slower electrophoretic mobility could be detected (Fig 1A). In T cells this difference has been correlated with phosphorylation of Lck on serine residues following exposure to activating signals.19 CLL B cells and control B cells expressed similar levels of the B-cell–specific Src family PTK Lyn (Fig 1B). As opposed to B cells, no difference in the levels of Lck could be detected in peripheral blood T cells from the patients as compared to control T cells from healthy donors (data not shown).
Although the anti-Lck MoAb did not cross-react with other known lymphocyte-specific Src family PTKs (see Materials and Methods), a potential cross-reaction with an as yet unidentified new family member could not be ruled out. mRNA purified from CLL B cells was therefore tested by RT-PCR for the presence of an Lck specific transcript. A primer complementary to the 3′ end of the coding region of Lck was used to generate the first strand by retrotranscription. A fragment spanning 570 bp at the 5′ end of the Lck coding region was then amplified by PCR. This region is the least conserved among the sequences encoding Src family kinases. The results from two representative B-CLL patients are shown in Fig 2A. A fragment of the expected size was obtained, which comigrated with the fragment obtained from the positive controls. The specificity of the fragment for Lck sequences was confirmed by Southern blot analysis of the same samples, using a 32P-labeled human Lck cDNA probe (Fig 2B).
RT-PCR analysis of Lck expression in B-CLL. (A) Ethidium bromide staining of the amplification products of an Lck-specific first-strand cDNA retrotranscribed from the mRNA from either CLL B cells (lanes 3 and 4) or control T cells (lane 2) or THP-1 cells (lane 6). PCR amplification of the same region of the Lck coding sequence from a pGEX-Lck construct is shown (lane 1). Lane 2, molecular-weight marker. (B) Phosphorimager print of a Southern blot hybridization of the same samples with 32P-labeled Lck cDNA.
RT-PCR analysis of Lck expression in B-CLL. (A) Ethidium bromide staining of the amplification products of an Lck-specific first-strand cDNA retrotranscribed from the mRNA from either CLL B cells (lanes 3 and 4) or control T cells (lane 2) or THP-1 cells (lane 6). PCR amplification of the same region of the Lck coding sequence from a pGEX-Lck construct is shown (lane 1). Lane 2, molecular-weight marker. (B) Phosphorimager print of a Southern blot hybridization of the same samples with 32P-labeled Lck cDNA.
While the data show that Lck is expressed in B cells from B-CLL patients, they do not provide any information about Lck activity in these cells. To understand whether Lck from CLL B cells is functional, Lck-specific immunoprecipitates were subjected to in vitro kinase assays using enolase as exogenous substrate. As shown in Fig3, a significant phosphorylation of enolase could be detected in in vitro kinase assays of Lck-specific immunoprecipitates from CLL B cells, showing that Lck expressed in B cells from B-CLL patients is functional. The levels of Lck activity correlated with the levels of protein (Fig 3), suggesting that Lck is not hyperactive in CLL B cells.
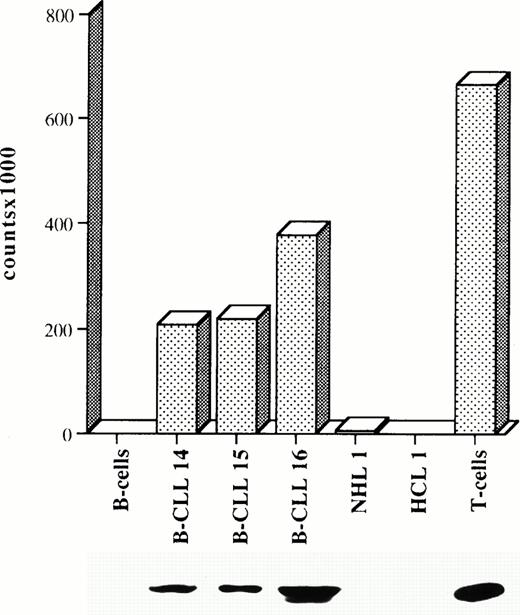
Lck is functional in CLL B cells. Quantitation of32P labeling of enolase by Lck in in vitro kinase assays of lysates of either normal peripheral blood B cells or B cells from three representative B-CLL patients (B-CLL), a hairy cell leukemia (HCL) patient, a patient with non-Hodgkin's lymphoma (NHL) in the leukemic phase, or normal T cells. Equal amounts of proteins for each lysate were used for Lck immunoprecipitation. An anti-Lck immunoblot of the same samples is shown below the graph. Each kinase assay was repeated at least twice.
Lck is functional in CLL B cells. Quantitation of32P labeling of enolase by Lck in in vitro kinase assays of lysates of either normal peripheral blood B cells or B cells from three representative B-CLL patients (B-CLL), a hairy cell leukemia (HCL) patient, a patient with non-Hodgkin's lymphoma (NHL) in the leukemic phase, or normal T cells. Equal amounts of proteins for each lysate were used for Lck immunoprecipitation. An anti-Lck immunoblot of the same samples is shown below the graph. Each kinase assay was repeated at least twice.
To understand whether Lck expression is restricted to B-CLL, we tested different leukemic B cells for expression of Lck. They included B cells isolated from two patients with HCL and two patients with NHL in the leukemic phase. As expected, B cells from both types of leukemias lacked CD5 expression (data not shown). In addition, three tumor lines derived from different cell types (ie, the monocytic line THP-1, the neuronal line PC12, and the epidermoid line A431) were analyzed. Neither THP-1 nor PC12 nor A431 cells expressed Lck (data not shown). Furthermore, no Lck could be detected in B cells from either HCL or NHL in the leukemic phase (Fig 3 and data not shown). This result was confirmed in in vitro kinase assays of Lck-specific immunoprecipitates (Fig 3). Thus Lck expression is a distinctive feature of CLL B cells.
Expression of Lck in normal CD5+ B-1 cells.
Two alternative explanations could account for the expression of Lck in B-CLL. One possibility is that Lck is ectopically expressed in B cells from this type of leukemia but not in normal B cells. In this case Lck might potentially be involved in the development of B-CLL, as alterations in the levels of Lck expression, even in the absence of an activating mutation, have been shown to result in thymic tumorigenesis in genetically engineered mouse models.16 The other possibility is that Lck expression is a feature of normal B-1 cells and that uncontrolled expansion of this B-cell population would account for the relatively high levels of Lck found in B cells from B-CLL patients. To address this question we analyzed lysates of normal B cells from different lymphoid organs characterized by different ratios of CD5−/CD5+ B cells.
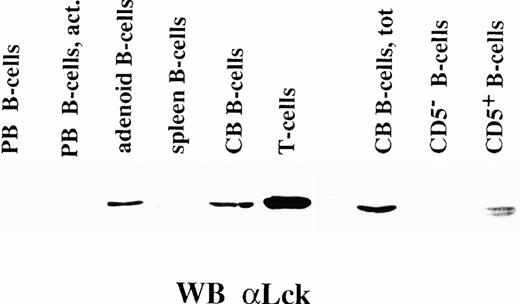
B cells were purified from peripheral blood, spleen, adenoid, and cord blood and the relative numbers of CD5− and CD5+ B cells were determined by flow cytometry. The mean proportions of CD5+ B cells in these organs were 11.8%, 17.3%, 28.8%, and 57.2% of total B cells, respectively. Lysates of unfractionated B cells from these sources were analyzed by immunoblot for the presence of Lck. The results are presented in Fig4. No Lck was detectable in B cells purified either from adult peripheral blood or from spleen, which were mostly CD5 negative. No induction of Lck expression was observed, even following activation of peripheral blood B cells by surface IgM cross-linking (Fig 4). By contrast, B cells from both adenoid and cord blood expressed relatively high levels of Lck, albeit not comparable to the levels found in T cells (Fig 4). Thus Lck can be found in B-cell preparations that include a significant CD5+ B-cell subpopulation, suggesting that Lck is expressed specifically by CD5+, B-1 cells. To confirm this point, CD5−and CD5+ cells were separated from purified cord blood B cells by FACS sorting and tested by immunoblot for the presence of Lck. As shown in Fig 4, Lck could only be detected in CD5+ B cells. Thus, Lck is expressed in normal B-1 cells, and its presence in B cells from B-CLL patients is likely due to the selective expansion of the B-1 cell subpopulation.
Expression of Lck in normal CD5+ B cells. Immunoblot analysis using an anti-Lck MoAb of lysates from normal B cells from different lymphoid organs. On the right is shown a similar immunoblot of lysates of total cord blood B cells (CB), as well as of the purified CD5− and CD5+ B-cell populations from the same cord blood sample. A lysate from normal T cells is included as a positive control. PB, resting peripheral blood B cells; PB act, peripheral blood B cells activated by surface IgM cross-linking; spleen, B cells purified from spleen; adenoid, B-cells purified from adenoid, CB, cord blood B cells.
Expression of Lck in normal CD5+ B cells. Immunoblot analysis using an anti-Lck MoAb of lysates from normal B cells from different lymphoid organs. On the right is shown a similar immunoblot of lysates of total cord blood B cells (CB), as well as of the purified CD5− and CD5+ B-cell populations from the same cord blood sample. A lysate from normal T cells is included as a positive control. PB, resting peripheral blood B cells; PB act, peripheral blood B cells activated by surface IgM cross-linking; spleen, B cells purified from spleen; adenoid, B-cells purified from adenoid, CB, cord blood B cells.
CD5− B-2 cells acquire Lck expression after transformation by EBV.
Our data show that CD5− B-2 cells, the major subset of normal B cells, fail to express Lck, even following in vitro activation by surface IgM cross-linking. An interesting question is whether the gene encoding Lck in B-2 cells is irreversibly switched off or, conversely, B-2 cells could acquire the capacity to express Lck ectopically in anomalous settings, ie, following transformation. As shown in Fig 3, CD5− B cells freshly isolated from two types of B-cell malignancy, HCL and NHL, lack Lck expression, suggesting that Lck is not a general marker of transformed B cells. We then tested chronically activated CD5−, EBV-transformed B cells for Lck expression. Fifteen lymphoblastoid B-cell lines were derived from B cells of healthy donors by transformation with EBV. Two B-cell lines derived from Burkitt's lymphoma (Daudi and Raji) and the EBV+ B-cell line RPMI-1788 were also assessed for Lck expression. With the exception of two of the EBV-transformed lines, all other lines were CD5− (data not shown). The results of a representative immunoblot experiment with anti-Lck MoAb are shown in Fig 5A. Significant levels of Lck expression were consistently found in all EBV transformed B-cell lines derived from healthy donors, as well as in Daudi, Raji, and RPMI-1788 cells, independently of CD5 expression. In all these cell lines, two Lck immunoreactive species could be detected, with a high ratio of the species migrating with a slower electrophoretic mobility (Fig 5A). The identity of Lck was confirmed by RT-PCR on mRNA purified from EBV-transformed B-cells (data not shown). Thus, while B-1 cells normally express Lck, B-2 cells ectopically express Lck following EBV transformation.
Expression of Lck in EBV-transformed B cells. (A) Immunoblot analysis using an anti-Lck MoAb of lysates from EBV-transformed lymphoblastoid B-cell lines, or Daudi, Raji, and RPMI-1788 B-cell lines. A lysate from normal T cells is included as a positive control, as well as a lysate from normal peripheral blood B cells as a negative control (PB). (B) Immunoblot analysis using an anti-Lck MoAb of lysates from either freshly isolated peripheral B cells from healthy controls (PB1, PB2) or EBV-transformed lymphoblastoid B-cell lines from the same controls (B-EBV1, B-EBV2). A lysate from normal T cells is included as a positive control.
Expression of Lck in EBV-transformed B cells. (A) Immunoblot analysis using an anti-Lck MoAb of lysates from EBV-transformed lymphoblastoid B-cell lines, or Daudi, Raji, and RPMI-1788 B-cell lines. A lysate from normal T cells is included as a positive control, as well as a lysate from normal peripheral blood B cells as a negative control (PB). (B) Immunoblot analysis using an anti-Lck MoAb of lysates from either freshly isolated peripheral B cells from healthy controls (PB1, PB2) or EBV-transformed lymphoblastoid B-cell lines from the same controls (B-EBV1, B-EBV2). A lysate from normal T cells is included as a positive control.
The finding that Lck is present not only in EBV-transformed lymphoblastoid B-cell lines, but also in Daudi, Raji, and RPMI-1788 cells, which are all positive for EBV nuclear antigens, suggests the possibility that Lck expression might be induced by B-cell transformation by EBV. To test this hypothesis we probed peripheral blood B cells from healthy donors from which EBV-transformed lymphoblastoid, Lck positive, B-cell lines were derived. As shown in Fig 5B, Lck could be detected in B cells from healthy donors only after EBV transformation, strongly supporting the notion that Lck expression in these B-cell lines is a consequence of EBV transformation.
Lck is functionally coupled to CD5 in CLL B cells.
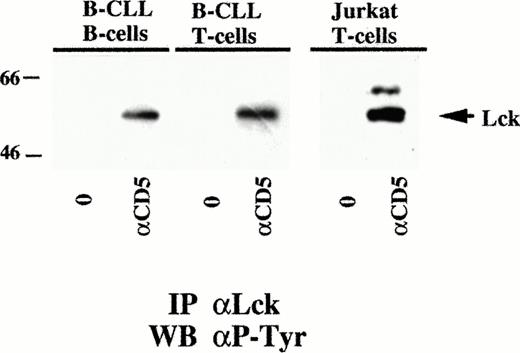
In T cells, Lck has been shown to bind to the cytoplasmic domain of CD5.20 Although this interaction is significantly weaker than the one involving CD4, it is sufficient to functionally couple CD5 to Lck, as CD5 triggering results in Lck activation.20 We asked whether CD5 engagement on either CLL B cells or EBV-transformed B-cells could initiate a signaling pathway involving Lck activation. Purified CLL B cells, as well as purified T cells, from three different patients were triggered with anti-CD5 MoAb. Lck-specific immunoprecipitates from these cells were then analyzed by immunoblot using an anti-phosphotyrosine MoAb. As a positive control, we used the leukemic T-cell line Jurkat, shown by flow cytometry to express high levels of CD5 (data not shown). The results obtained with a representative patient are presented in Fig 6. A significant induction of tyrosine phosphorylation of Lck in response to CD5 triggering could be detected in CLL B cells, at levels comparable to those detected in T cells from the same patients. Thus, CD5 is functionally coupled to Lck in CLL B cells.
Lck is functionally coupled to CD5 in CLL B cells. Immunoblot analysis using anti-phosphotyrosine MoAb of Lck-specific immunoprecipitates from lysates of either purified B and T cells from a representative B-CLL patient or from control Jurkat T cells. The migration of Lck, as revealed by immunoblot with an anti-Lck MoAb of a control Jurkat T-cell lysate on the same gel, is indicated.
Lck is functionally coupled to CD5 in CLL B cells. Immunoblot analysis using anti-phosphotyrosine MoAb of Lck-specific immunoprecipitates from lysates of either purified B and T cells from a representative B-CLL patient or from control Jurkat T cells. The migration of Lck, as revealed by immunoblot with an anti-Lck MoAb of a control Jurkat T-cell lysate on the same gel, is indicated.
DISCUSSION
Our data shed light on two controversial questions regarding B-cell biology, on the one hand mature B-cell lineage, and on the other the identity of the B-cell population, which is the target for the transforming events underlying B-CLL. The CD5+ B-cell subset, designated B-1, can be distinguished from conventional B cells by a number of features such as anatomic localization, functional characteristics, and gene expression.1-3 In contrast to conventional B cells, B-1 cells maintain their number by self-replenishment and exert a feedback regulation on de novo production of B-1 cells from progenitors. Furthermore, their antibody repertoire is built on a restricted set of V genes and is highly enriched in autoreactive antibodies,1-3 suggesting the potential implication of this B-cell subset in autoimmune diseases. Strong evidence of the independent origin of B-1 and conventional B cells from different lineages of progenitor cells has been obtained in mouse.6,7 In humans, the origin of B-1 cells from a distinct lineage, rather than from a modification of phenotypical and functional features of B-2 cells, is still under debate. Taken together with the recent demonstration of a constitutive STAT3 activity restricted to B-1 cells,9 our finding of a differential expression of Lck in B-1 cells, but not conventional B cells, supports the existence of separate B-cell lineages of progenitor cells in man. Given the key role of Lck in thymocyte mitogenesis,16 21this differential expression of Lck might underlie the unique capacity of self-renewal of B-1 cells.
The second question focuses on the cellular origin of B-CLL. Since this type of leukemia is characterized by the accumulation of CD5+ B cells, B-1 cells have been proposed as the normal counterpart of CLL B cells. A number of similarities between normal CD5+ B cells and CLL B cells have been highlighted, particularly concerning their production of polyreactive, low-affinity autoantibodies in the absence of extensive somatic hypermutation.10 However, normal and malignant CD5+ B cells differ significantly in a number of features. In contrast to normal CD5+ B cells, CLL CD5+ B cells express very low levels of surface immunoglobulins11and show a reduced proliferative response to B-cell antigen receptor cross-linking,22 which correlates with a reduced induction of protein tyrosine kinase activity and a defective mobilization of intracellular Ca2+.11,13 Furthermore, they accumulate in the G0 phase of the cell cycle, as documented both by kinetic studies and by the lack of c-mycexpression.10 The latter property, combined with Bcl-2 overexpression,23,24 is likely to play a major role in the accumulation of CLL B cells. Our finding of Lck expression as a common feature of both normal CD5+ B cells and CLL B cells provides strong evidence in favor of B-1 cells being the target of the transforming events leading to B-CLL. It should be noted that, in addition to mitogenesis, Lck has been implicated in cell survival.25 Thus the outcome of Lck expression might be proliferation or survival, dependent on the different cellular context of the normal and malignant B-1 cell, respectively. Since CD5 is functionally coupled to Lck, an important factor in normal and malignant cell fate determination might be the encounter with B cells expressing the CD5 counterreceptor CD72.26
Our data suggest that the expression of Lck in CLL B cells and in EBV-transformed B cells could have two different meanings. Lck expression in B-CLL could be accounted for by the selective expansion of malignant B-1 cells and would not be as such directly involved in neoplastic transformation. By contrast, Lck expression appears to be an anomalous feature of CD5 negative, B-2 cells, acquired following transformation by EBV. Although our data do not rule out the possibility that Lck might be expressed in other types of B-cell malignancies, the lack of Lck expression in HCL and NHL B cells shows that Lck is not a common feature of transformed CD5− B cells. The presence of Lck in EBV-transformed B cells, but not in normal peripheral B cells of the same donor, suggests that EBV nuclear antigens, which have been shown to interfere with normal gene expression,27-29 might contribute to the activation of the Lck gene promoter, resulting in ectopic Lck expression in CD5− B cells. As opposed to B-CLL, this event might play a role in B-cell transformation by EBV. The crucial role of Lck both in thymocyte development and in T-cell activation has been clearly demonstrated.21,30 The levels of Lck expression in T cells must be strictly controlled, as shown by the dramatic alterations associated with Lck overexpression. Even in the absence of an oncogenic mutation, Lck overexpression in the thymus results in thymic tumorigenesis.16 Furthermore, the gene encoding Lck was first cloned from the mouse thymoma line LSTRA, which is characterized by abnormally high levels of wild-type Lck.31 Thus, an alteration in the protein tyrosine kinase balance produced by the ectopic expression of Lck is likely to have profound effects on the proliferative potential of the B cell.
ACKNOWLEDGMENT
The authors thank Sonia Grassini for skilled technical assistance and Leonardo Gamberucci for photographic assistance. They also thank B. Perussia for the generous gift of the B36.1 hybridoma, M. Ferrarini and P. Ghiara for their kind gift of cell lines, and S. Plyte for critical reading of the manuscript.
Supported by the Italian Association for Cancer Research (AIRC). The contribution of the Regione Toscana (Ricerca Sanitaria Finalizzata) and the MURST (quota 60%) is also acknowledged. M.B.M. is the recipient of an FIRC fellowship.
Address reprint requests to Cosima T. Baldari, PhD, Department of Evolutionary Biology, University of Siena, Via Mattioli 4, 53100 Siena, Italy.
The publication costs of this article were defrayed in part by page charge payment. This article must therefore be hereby marked "advertisement" is accordance with 18 U.S.C. section 1734 solely to indicate this fact.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal