To the Editor:
In a recent article in BLOOD, Sergeyeva et al1 describe a secondary form of congenital polycythemia that appears to be particularly frequent in Chuvasia, a region in the central part of European Russia. This erythrocytosis is transmitted as an autosomal recessive trait and generally becomes clinically manifest in the second decade of life. Because these individuals have elevated erythropoietin (Epo) levels with no abnormality in hemoglobin (Hb) dissociation curve or red blood cell 2,3-diphosphoglycerate, Sergeyeva and coworkers1 conclude that the excessive Epo production likely reflects an abnormal oxygen sensing mechanism.
We studied a 17-year-old girl with a history of intermittent headache and progressive appearance of plethora. One year before admission a blood cell count showed Hb 19.4 g/dL, hematocrit 65.6%, red blood cell 7.65 × 1012/L, white blood cell 4.15 × 109/L, and platelet 130 × 109/L. Her parents and a sister had normal blood counts. Spleen size was normal and arterial saturation was 96.6%. Serum Epo (sEpo) was increased (107 mU/mL), and there was no evidence of in vitro spontaneous burst-forming unit–erythroid growth from peripheral blood. Because Hb increased to over 20 g/dL, in the months preceding admission to our department the patient underwent regular phlebotomies to maintain levels around 16 g/dL.
We first excluded abnormalities in oxygen unloading of hemoglobin by measuring Hb P50 using the Hemox-Analyzer (TCS Medical Products Division, Southampton, PA). The oxyhemoglobin dissociation curve was normal and P50 was 24.5 mmHg (normal values range from 23 to 27.5 mm Hg).
Serum Epo was determined using venous blood sampled without anticoagulant by means of an enzyme-linked immunosorbent assay (ELISA) (CLINIGEN, Amgen Diagnostic, Thousand Oaks, CA); values in normal reference individuals range from 6 to 20 mU/mL. Serum transferrin receptor (sTfR), the level of which provides an estimate of erythroid marrow activity,2 was also measured by an ELISA (CLINIGEN); values in normal reference individuals range from 1.47 to 3.4 mg/L.
Basal sEpo was 204 mU/mL with a Hb level of 16.6 g/dL, a value 10 times the upper normal limit. At the same time sTfR was 9.7 mg/L, ie, four times the mean normal level. It should be noted that in this case the elevated sTfR level was likely a result of both increased erythroid marrow activity and iron deficient erythropoiesis. In fact, transferrin saturation was 11%, and defective iron supply to erythropoiesis increases both the expression of transferrin receptors on erythroid cells and sTfR level.2 In any case, the above findings indicated an inappropriately elevated endogenous Epo production with secondary expansion of erythroid marrow activity. Computed tomography scans of the chest and the abdomen, ultrasonography of the abdomen, and magnetic resonance imaging of the brain excluded Epo-producing tumors and/or renal disorders. In addition, sEpo appeared to be normally influenced by oxygen-mediated feedback (107 mU/mL at a Hb level of 19.4 g/dL v 204 mU/mL at 16.6 g/dL).
We therefore concluded for a congenital form of polycythemia, transmitted with an autosomal recessive pattern of inheritance and caused by an upregulated oxygen sensing mechanism.3 This condition appears to be very similar to the Chuvash polycythemia.1
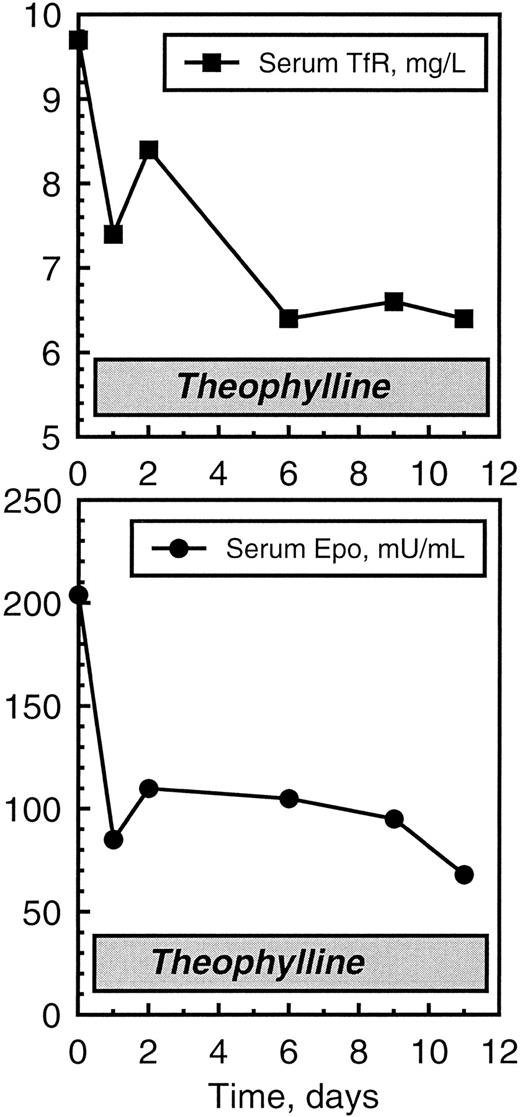
To further investigate the regulation of Epo production, we evaluated whether Epo synthesis was normally modulated by adenosine as a second messenger. Adenosine receptor antagonists like theophylline, in fact, attenuate the production of Epo in both normal subjects and patients with erythrocytosis after renal transplantation.4 5 We therefore tested the effect of theophylline on sEpo and sTfR levels. The patient was given intravenous theophylline, 240 mg two times a day for 2 days; subsequently she took a long-acting preparation of theophylline (7 mg per kg of body weight per day). The time course of sEpo and sTfR under theophylline treatment is reported in Fig1. There was a definite decrease in both endogenous erythropoietin production and erythroid marrow activity within a few days, although after 11 days values remained still elevated. Treatment was continued with oral administration of theophylline. Hb level declined to about 15 g/dL and remained stable around this value for several months.
Effects of theophylline on serum Epo and serum transferrin receptor (TfR) in the 17-year-old girl with erythropoietin-dependent erythrocytosis. Theophylline was given intravenously in the first 2 days and then orally (see text for details).
Effects of theophylline on serum Epo and serum transferrin receptor (TfR) in the 17-year-old girl with erythropoietin-dependent erythrocytosis. Theophylline was given intravenously in the first 2 days and then orally (see text for details).
In conclusion, we suggest to evaluate the effect of theophylline on endogenous Epo production in Chuvash polycythemia. This may allow to gain a deeper insight into the pathophysiology of this disorder and to try a potentially useful therapeutic tool.
ACKNOWLEDGMENT
This study has been supported by IRCCS (Istituto di Ricovero e Cura a Carattere Scientifico) Policlinico S. Matteo and the Ferrata Storti Foundation, Pavia, Italy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal