To the Editor:
In a recent report we showed the clinical relevance of point mutations in the cytoplasmic domain of the granulocyte colony-stimulating factor receptor (G-CSFR) gene in patients with severe congenital neutropenia.1 Here we document that the point mutations in the G-CSFR mRNA do not lead to the expression of a truncated G-CSFR protein at the cell surface.
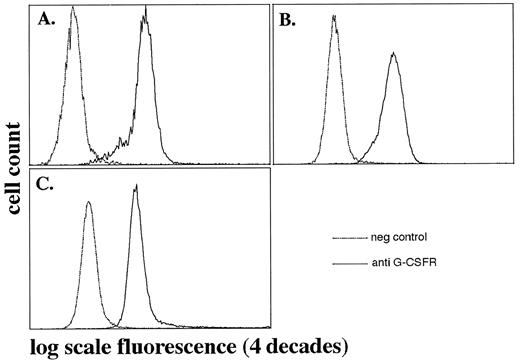
Detection of the G-CSFR in flow cytometry analyses. Expression of the G-CSFR on peripheral blood neutrophils from patients with SCN and a healthy control were determined using anti-G-CSFR antibody (MoAb 129; IgG1) and FITC-conjugated rabbit-antimouse IgG. The x-axis shows log scale fluorescence, the y-axis cell number. Two overlapping open histogramms of cells incubated with or without anti–G-CSFR antibody are shown. (A and B) Patients with severe congenital neutropenia, with point mutations in the cytoplasmic domain of the G-CSFR gene. (C) Healthy control (Table 1).
Detection of the G-CSFR in flow cytometry analyses. Expression of the G-CSFR on peripheral blood neutrophils from patients with SCN and a healthy control were determined using anti-G-CSFR antibody (MoAb 129; IgG1) and FITC-conjugated rabbit-antimouse IgG. The x-axis shows log scale fluorescence, the y-axis cell number. Two overlapping open histogramms of cells incubated with or without anti–G-CSFR antibody are shown. (A and B) Patients with severe congenital neutropenia, with point mutations in the cytoplasmic domain of the G-CSFR gene. (C) Healthy control (Table 1).
Severe congenital neutropenia (SCN) or Kostmann-syndrome, first described by Kostmann in 1956,2 is an autosomal recessive disorder of myelopoiesis characterized by severe neutropenia with absolute neutrophil counts (ANC) below 200/μL in peripheral blood due to an impairment of myeloid differentiation on the level of promyelocytes.3 Daily subcutaneous administration of pharmacological dosages of G-CSF (1 to 120 μg/kg/d) in these patients leads to an increase in neutrophil counts to above 1,000 neutrophils/μL, and is associated with a dramatic clinical improvement.3 A defect in the G-CSFR molecule or in the G-CSF–mediated signal pathways might be responsible for this defective response. Recent findings showed that in those patients with severe congenital neutropenia who developed subsequently myeloid leukemias, point mutations in the cytoplasmic region of the G-CSFR mRNA were identified.1,4,5 In one allele of the G-CSFR gene, the nucleotide cytosine was substituted by a thymine (CAG to TAG) at nucleotide 2429, 2390, or 2384, respectively1 (numbering of the nucleotides refers to Fukunaga et al6 ), which resulted in a change from the amino acid glutamine to a stop codon. The critical region of the G-CSFR cytoplasmic domain, where all the mutations could be detected so far, is located between nucleotide 2384 and 2429.1 However, the majority of SCN patients does not demonstrate mutations in this critical region of the cytoplasmic domain of the G-CSFR. In this study we investigated whether the mutated G-CSFR mRNA is translated into a truncated G-CSFR protein in patients with point mutations in the cytoplasmic domain of the G-CSFR mRNA.
On the basis of recent reports7,8 documenting that the G-CSFR protein is expressed on myeloid precursors and mature neutrophilic granulocytes, we investigated the G-CSFR protein expression on myeloid precursors, mature neutrophilic granulocytes, and monocytes from these patients using flow cytometry analyses. In addition, we examined whole cell lysates from neutrophilic granulocytes in Western blot analyses for the determination of the molecular mass of the G-CSFR protein. Using a monoclonal antibody (MoAb) against an epitope of the extracellular domain of the G-CSFR protein produced in our laboratory (MoAb 129; IgG1),9 we investigated G-CSFR protein expression in two patients with severe congenital neutropenia with point mutations in the cytoplasmic domain of the G-CSFR gene (Fig 1A and B), and one healthy individual (Fig 1C). In Fig 1 it is shown that the G-CSFR protein was expressed on neutrophilic granulocytes from all patients investigated, as well as from the healthy control (Table 1).
Characteristics of the Presented Patients and Healthy Control (BK)
| Patient . | Sex . | Age (yr) . | SCN . | Mutation in the Cytoplasmic Domain . | AML . |
|---|---|---|---|---|---|
| BP | Female | 17 | Yes | Yes (nt 2384, 2390) | No |
| PB | Female | 15 | Yes | Yes (nt 2429) | No |
| BK | Female | 35 | No | Not done | No |
| Patient . | Sex . | Age (yr) . | SCN . | Mutation in the Cytoplasmic Domain . | AML . |
|---|---|---|---|---|---|
| BP | Female | 17 | Yes | Yes (nt 2384, 2390) | No |
| PB | Female | 15 | Yes | Yes (nt 2429) | No |
| BK | Female | 35 | No | Not done | No |
Abbreviations: AML, acute myeloid leukemia; nt, nucleotide.
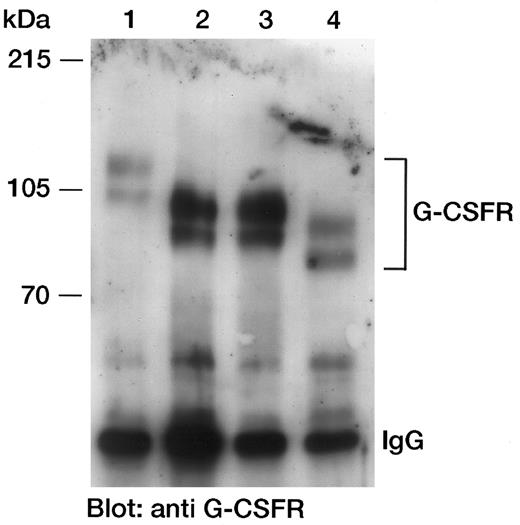
The mutations in the G-CSFR mRNA detected in SCN patients would lead to a stop codon and truncation of the G-CSFR protein. To investigate whether a truncated G-CSFR protein is expressed on the cell surface, we transfected a murine fibroblast cell line (C243) with the human wild-type G-CSFR (813 amino acids [aa]), and three deletion mutants (D1, aa 1-670; D2, aa 1-685; and D3, aa 1-634), to verify that we were able to detect the truncated receptor proteins. The MoAb 129 (IgG1) detects two proteins with molecular masses of 130 kD and 100 kD in the wild-type G-CSFR–transfected cells. We suggest that the 130-kD protein is the glycosylated form of the receptor and that the 100-kD protein is an only partially glycosylated receptor protein. In Fig 2 the wild-type G-CSFR, with a molecular mass of 130/100 kD, and the three deletion mutants with estimated molecular masses of 106/90 kD (D1, D2) and 96/81 kD (D3), respectively, are shown. These data show that the deletion mutants are expressed also as truncated membrane receptor protein.
Detection of the G-CSFR protein in Western blot analyses. In each case, 2 × 107 C243 cells stably transfected with the human wild-type G-CSFR or different deletion mutants (D1-D3) were lysed. The G-CSF receptors were immunoprecipitated with MoAb 129, separated by SDS-PAGE using an 8% wt/vol polyacrylamide gel, and blotted onto nitrocellulose membranes. Detection was performed with anti–G-CSFR antibody (MoAb 129; IgG1) and horseradish peroxidase (HRP)-conjugated goat-antimouse IgG. The immunoblot was developed by the enhanced chemiluminescence method following the manufacturer's guidelines (ECL; Amersham, Braunschweig, Germany). Lane 1, wild-type G-CSFR (aa 1-813); lane 2, deletion mutant D1 (aa 1-670); lane 3, deletion mutant D2 (aa 1-685); lane 4, deletion mutant D3 (aa 1-634).
Detection of the G-CSFR protein in Western blot analyses. In each case, 2 × 107 C243 cells stably transfected with the human wild-type G-CSFR or different deletion mutants (D1-D3) were lysed. The G-CSF receptors were immunoprecipitated with MoAb 129, separated by SDS-PAGE using an 8% wt/vol polyacrylamide gel, and blotted onto nitrocellulose membranes. Detection was performed with anti–G-CSFR antibody (MoAb 129; IgG1) and horseradish peroxidase (HRP)-conjugated goat-antimouse IgG. The immunoblot was developed by the enhanced chemiluminescence method following the manufacturer's guidelines (ECL; Amersham, Braunschweig, Germany). Lane 1, wild-type G-CSFR (aa 1-813); lane 2, deletion mutant D1 (aa 1-670); lane 3, deletion mutant D2 (aa 1-685); lane 4, deletion mutant D3 (aa 1-634).
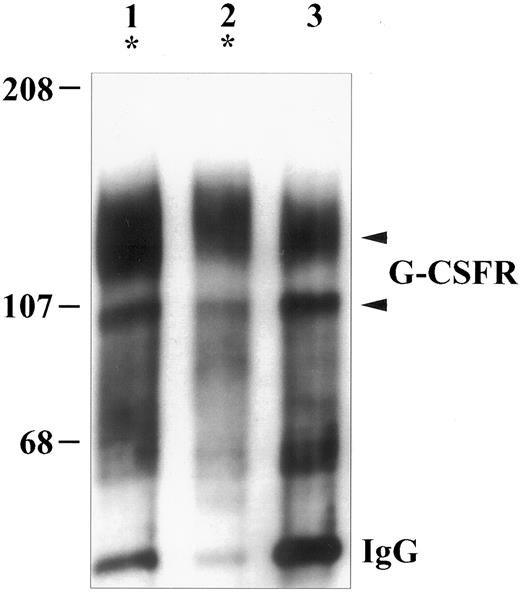
To examine whether the truncated G-CSFR protein is also expressed in patients with G-CSFR mutations, we investigated lysates from neutrophilic granulocytes from SCN patients BP and PB (Table 1) in Western blot analyses. In patient BP and patient PB, patients with severe congenital neutropenia, the receptor mutations could be detected in November 1995 and in November 1992, respectively, for the first time. In cells obtained in later points in time, the receptor mutations continued to be present, but there were no signs of myelodysplastic syndrome/acute myeloid leukemia (MDS/AML) in patient BP and patient PB so far. In patients BP and PB (Fig 3, lanes 1 and 2), and the healthy control (Fig 3, lane 3) the G-CSFR protein could be detected in neutrophilic granulocytes from peripheral blood with a similar molecular mass (130 kD/100 kD). Lanes 1 and 2 in Fig 3 show the patients with point mutations in the cytoplasmic domain of the G-CSFR mRNA. However, the molecular mass of the G-CSFR proteins in these two patients was comparable to patients without G-CSFR mutations (data not shown) and the healthy control (Fig 3). This is in contrast to our data obtained in G-CSFR–transfected murine fibroblasts (Fig 2). This is also in contrast to experiments in which the mutated cDNA was transfected into murine L-GM cells in vitro.5 These cells did not differentiate to mature neutrophilic granulocytes.5 The molecular reasons for this discrepancy between mRNA and protein expression in cell lines and in SCN patients with G-CSFR mutations remains to be identified. Our hypothesis is that, in contrast to the cell lines, in SCN patients the mutated mRNA is recognized by control and/or repair systems and might not be translated into a protein or the processed truncated protein would be degraded or deleted (eg, by chaperones) before its expression at the cell surface. The expression of functional normal G-CSFR proteins is also supported by the fact that patients BP and PB respond to treatment with G-CSF in vivo1 to the same dosage of G-CSF as they did before they acquired the G-CSFR mutations.
Detection of the G-CSFR protein in Western blot analyses. 1 × 107 neutrophils were lysed. The G-CSFRs were immunoprecipitated with MoAb 129, separated by SDS-PAGE using an 8% wt/vol polyacrylamide gel, and blotted onto nitrocellulose membranes. Detection was performed with anti–G-CSFR antibody (MoAb 129; IgG1) and HRP-conjugated goat-antimouse IgG. The immunoblot was developed by the enhanced chemiluminescence method following the manufacturer's guidelines (ECL; Amersham). Lanes 1 and 2, patients with severe congenital neutropenia (patients with point mutations in the cytoplasmic domain of the G-CSFR mRNA). Lane 3, Healthy control. The arrows point out the G-CSFR proteins.
Detection of the G-CSFR protein in Western blot analyses. 1 × 107 neutrophils were lysed. The G-CSFRs were immunoprecipitated with MoAb 129, separated by SDS-PAGE using an 8% wt/vol polyacrylamide gel, and blotted onto nitrocellulose membranes. Detection was performed with anti–G-CSFR antibody (MoAb 129; IgG1) and HRP-conjugated goat-antimouse IgG. The immunoblot was developed by the enhanced chemiluminescence method following the manufacturer's guidelines (ECL; Amersham). Lanes 1 and 2, patients with severe congenital neutropenia (patients with point mutations in the cytoplasmic domain of the G-CSFR mRNA). Lane 3, Healthy control. The arrows point out the G-CSFR proteins.
The majority of patients with severe congenital neutropenia does not demonstrate mutations in this critical region of the cytoplasmic domain of the G-CSFR. Therefore, we suggest that patients with severe congenital neutropenia who acquire a point mutation in the cytoplasmic domain of the G-CSFR may represent the subgroup of patients in whom the neutropenia is a preleukemic disorder. However, the molecular mechanisms for the leukemogenesis between the point in time when G-CSFR mutations occur and overt leukemia remains to be investigated. Other genetic aberations such as loss of chromosome 7 (monosomy 7) or mutations in oncogenes, eg, ras-mutations,10 might be subsequent steps in the development of leukemia.
ACKNOWLEDGMENT
Supported in part by Grant No. We 942/4-2 from the Deutsche Forschungsgemeinschaft, and from AMGEN Inc, Thousand Oaks, CA.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal