To the Editor:
Mycosis fungoides (MF ) is a chronic CD4+ T-cell lymphoma of unknown etiology. Several cases have presented with either dry skin or lichenification, while also demonstrating hyperpigmentation and itching as the disease expands. When the infiltration becomes exacerbated, the histopathology demonstrates a marked degree of acanthosis. To answer the question as to whether these clinical and histological features are related to the function of mast cells, we studied the role of mast cells and their growth factor, stem cell factor (SCF ), in two cases of tumor-stage MF (case 1: a 48-year-old man, and case 2: a 53-year-old woman) who showed diffuse hyperpigmentation and itching. We histologically observed a large number of mast cells in the upper dermis, some of which had migrated into the epidermis, while SCF expression was detected on the tumor cells.
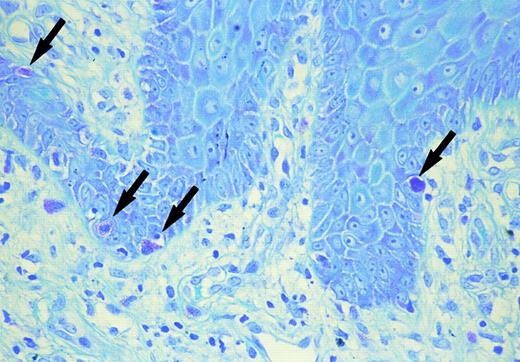
Skin biopsy specimens were fixed with 10% formalin solution and were stained with hematoxylin-eosin and toluidine blue at a pH of 2.5, 4.1, and 7.0 to identify mast cells. Mast cells containing metachromatic granules were counted under high magnification of the ×400 power-fields of a light microscope. As the mast cells were most numerous in the papillary dermis or upper dermis of the MF lesion, the number of metachromatic cells was counted in 10 fields in this layer. Immunohistochemistry was performed with a standard avidine-biotin peroxidase technique (Nichirei Co, Tokyo Japan) using recombinant anti-SCF monoclonal antibody (Genzyme, Cambridge, MA) (dilution at a final concentration of 1:50). The sections were developed with 3-amino-9-ethylcarbazole as chromogen, counterstained with hematoxylin, dehydrated, cleared, and mounted. Negative controls were prepared by omitting of the specific antibody. SCF concentration in the serum before systemic chemotherapy was determined with a sandwich enzyme-linked immunosorbent assay (ELISA) kit (Amersham, UK). As controls, serum was obtained from 3 patients with infiltrative stage MF without either diffuse pigmentation or itching, and from 10 normal volunteers (5 males and 5 females; age range, from 44 to 60 years). Increased number of mast cells were observed in the upper dermis. The number of mast cells in the upper dermis (133.2 ± 15.6/mm2 in case 1, and 113.4 ± 10.1/mm2 in case 2) was significantly higher than that of either 3 infiltrative stage MF (44.6 ± 7.8/mm2 ) (P < .005) or normal healthy skin (38.5 ± 9.1/mm2 ) (P < .005 in case 1 and P < .005 in case 2). In both cases, intra-epidermal mast cells were shown by toluidine blue staining in a specimen from thigh in case 1 and from buttock in case 2 (Fig 1). Clinically, both lesions showed marked infiltration or lichenification. Double staining of toluidine blue and Periodic acid-Schiff (PAS) staining showed mast cells to be above the basal membrane. Immunohistochemistry demonstrated positive perinuclear staining in a cytoplasmic pattern for SCF on tumor cells, mast cells, endothelial cells, and keratinocytes in the acanthotic epidermis in both cases. The serum SCF concentration was increased (1,640 pg/mL in case 1 and 1,250 pg/mL in case 2) as compared with that in the 3 patients with MF, but without any diffuse pigmentation or itching (863 ± 145 pg/mL) as well as the normal volunteers (748 ± 256 pg/mL).
Mast cells in the basal layer of the epidermis (arrow) (toluidine blue).
These two cases of MF showed similar clinical and laboratory features such as diffuse pigmentation with itching, and an elevated level of serum IgE (1,400 U/mL in case 1 and 2,800 U/mL in case 2, normal: <250 U/mL). Both cases showed diffuse pigmentation before being treated by Psoralen-ultraviolet light A (PUVA) therapy. Other cases of MF lacking diffuse pigmentation, pruritus, or an elevated serum IgE did not show an increased number of mast cells as did those two cases. Hyperpigmentation associated with MF is relatively rare, and hyperpigmentation has been seen in pigmented purpura-like eruptions, diffuse hyperpigmented macules, poikiloderma atrophicans vasculare, and in the course of treatment including PUVA or cytostatic agents. Most reported cases with hyperpigmentation also have pruritus, which may thus suggest that the pathogenesis of itching and hyperpigmentation share a common mechanism. Those two cases showed an elevated level of plasma histamine which was determined by the radio-immunoassay (RIA) method (0.57 ng/mL in case 1 and 0.45 ng/mL, normal: <0.2 ng/mL). The main sources of histamine in the skin are mast cells which both synthesize and store histamine. Katayama et al1 reported that mast cell–derived mediators appear to play a role in epidermal hyperplasia in atopic dermatitis (AD). Imayama et al2 recently reported epidermal mast cells in AD which had not been observed in the epidermis; however, epidermal mast cells were found in non-involved skin specimens. Whether or not epidermal mast cells exist in the involved, lichenificated lesional skin in AD remains unknown. In our two cases, a large number of lesions were histologically examined and both sections showing intra-epidermal mast cells were biopsied from lichenificated skin lesions. Thus, we presume that mast cells appear to be involved in the induction of itching, hyperpigmentation, and lichenification, which later develop into acanthosis of the epidermis. Other possibilities must also be considered. That is, some mast cell growth-inducing factors may be released from lymphoid tumor cells or activated keratinocytes, and chemokines for mast cells might also be released from epidermal cells. Recently, SCF, which is a cytokine and the ligand for the protein product of the c-kit proto-oncogene, has been reported to be produced by fibroblasts, keratinocytes, mast cells or endothelial cells in the skin. The increased pigmentation of MF may be caused by SCF, which also stimulates the production of melanin by melanocytes.3 The supernatant of cultured mast cells has been shown to have a growth stimulatory effect on keratinocytes.1 The onset of acanthosis may thus be induced by mast cell–derived factors, which may in part be related to SCF. Furthermore, increased levels of interleukin-4 (IL-4) and IL-5 produced by not only tumor cells but also by mast cells may account for the elevated levels of serum IgE. In both cases, chemotherapy reduced the itching and serum IgE level in parallel, which may suggest that degranulation of mast cells was interrupted. It is of interest that epidermal ‘epidermotropic’ mast cells were found to be present in the biopsied specimens and showed marked acanthosis in both cases. Thus, we concluded that mast cells play a crucial role in the induction of diffuse pigmentation and itching in MF and intra-epidermal mast cells may play a role in the formation of marked acanthosis.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal