THE TERM CHRONIC myelogenous leukemia (CML) belies the insidious, unsparing course of this lethal hematopoietic malignancy. In CML, the malignant transformation of a hematopoietic stem cell results in a vast expansion of progenitor, precursor, and mature hematopoietic cells of malignant clonal origin and their premature release from the marrow into the blood. Although the clinical manifestation of these processes may be minimal at presentation, after a variable period of time, the disease inevitably progresses from a stable chronic phase easily controlled by conventional cytotoxic agent therapy to a blast crisis characterized by flooding of marrow and blood with immature cells and resulting in death. Malignant CML cells contain the Philadelphia chromosome (Ph) resulting from a translocation between chromosomes 9 and 22 [t(9; 22)(q34; q11)].1,2 This is reflected, at the molecular level, by the translocation of a portion of the c-ABL gene from chromosome 9 to the breakpoint cluster region (BCR) on chromosome 22 leading to the formation of an abnormal BCR-ABL hybrid gene.3 The BCR-ABL oncogene appears to play a critical role in the pathogenesis of CML.4 5
Allogeneic transplantation therapy for CML.At present, allogeneic bone marrow transplantation (BMT) remains the gold standard as aggressive therapy for CML. Chronic-phase patients receiving HLA-matched sibling donor transplants have a 45% to 70% probability of long-term disease-free survival, whereas patients transplanted with more advanced disease have a 15% to 40% probability of long-term survival.6 The efficacy of unrelated donor transplant therapy for CML has also been shown,7 and development of methodologies to improve donor-recipient MHC matching may expand the donor pool and improve outcome.8,9 In addition, the use of alternative sources of allogeneic stem cells for transplantation, including peripheral blood progenitor cells and umbilical cord blood cells, is being explored.10,11 Unfortunately, allogeneic transplantation has its limitations. A large proportion of CML patients may not be eligible for allogeneic transplantation because a suitably matched related or unrelated donor cannot be located or because of advanced patient age. Allogeneic transplantation, especially with an unrelated donor, may be associated with life-threatening infections, acute and chronic graft-versus-host disease (GVHD), costly delays in hospital discharge, prolonged convalescence, requirement for chronic antimicrobial and immunosuppressive therapy, and death. Evidence of molecular, cytogenetic, and even clinical relapses sometimes occurring as late as 5 to 10 years after transplantation12 is being recognized in recipients of either T-lymphocyte–depleted or unmanipulated grafts.13-15
Interferon-α (IFN-α) therapy for CML.Therapy of CML with the biological agent recombinant IFN-α can markedly alter the course of the disease in some patients.16 First-line therapy with IFN-α therapy in newly diagnosed chronic-phase CML patients has resulted in complete or partial hematologic remissions in 31% to 81% of cases, a major cytogenetic response (>65% Ph−) in 10% to 38% of cases, and complete cytogenetic responses (100% Ph−) in 7% to 26% of cases.16-22 Virtually all studies show that chronic-phase CML patients experiencing a complete or major cytogenetic response have a significant survival advantage over those who do not.18 Patients with major cytogenetic responses who remain on therapy have a suvival rate of greater than 80% at 5 to 7 years.16 However, therapy with IFN-α does not appear to be curative. Examination of Ph− marrow samples from complete cytogenetic responders with sensitive molecular genetic techniques invariably uncovers the BCR-ABL gene abnormality,23 and dormant Ph+ progenitors are present in the marrow of cytogenetic complete responders.24 Drawbacks to IFN-α therapy include a high incidence of side effects, which requires discontinuation of therapy in 15% to 25% of patients and dose reductions in 30% to 50% of patients.16 Approximately 50% of patients in cytogenetic remission on IFN-α at 4 years reported serious side effects (World Health Organization [WHO] grade IV) in one large trial.19 Despite these drawbacks, IFN-α has become an important therapeutic option.
Autologous transplantation therapy for CML.Although allogeneic BMT and IFN-α have undoubtedly changed the natural history of CML, there is still a need for alternative therapies because only a small proportion of patients can anticipate prolonged survival with IFN-α and because most patients do not qualify for allogeneic transplantation. Autologous transplantation has been effective in the therapy of other malignancies and is generating increasing clinical interest as another mode of therapy for CML. In this review, we will recapitulate the experience with autografting for CML, evaluate its efficacy, consider strategies to improve outcomes, and finally discuss the role of autografting amongst the spectrum of therapeutic options for CML.
Benign hematopoietic progenitors in CML marrow.The knowledge that benign hematopoietic progenitors coexist with their malignant counterparts in the marrow of some CML patients has tantalized proponents of autologous transplantation for many years. Transient Ph− hematopoiesis has been observed in CML patients after treatment with busulfan or with high-dose combination chemotherapy as well as in early autotransplantation studies.25-29 More recently, IFN-α treatment has resulted in complete cytogenetic remissions with restoration of Ph− hematopoiesis in some patients.30 In addition to this clinical experience, experimental evidence also supports the presence of benign progenitors in CML marrow. Both Ph+ and Ph− colonies were observed after in vitro culture of marrow from selected patients with Ph+ CML.31 More recently, Ph−, nonclonal, and therefore presumably normal primitive progenitors were obtained after ex vivo culture of CML marrow in Dexter-type long-term BM culture.32,33 In addition, selection of benign progenitors on the basis of cell surface phenotype has been reported.34-36 These observations strengthen the hypothesis that benign progenitors suitable for reconstitution of hematopoiesis after autologous transplantation can be recovered from the marrow or peripheral blood of at least some CML patients.
CLINICAL EXPERIENCE WITH AUTOLOGOUS TRANSPLANTATION FOR CML
Autologous Transplantation With Unselected Cells
The first autologous transplants for CML were performed on blast crisis patients who received high-dose chemotherapy alone or combined with total body irradiation followed by infusion of marrow or peripheral blood cryopreserved during chronic phase.37 38 It was observed that, although chronic-phase CML was reestablished in most patients, it was usually short-lived, with recurrence of advanced disease and death in 6 months to 1 year. Some patients with relatively long durations of remissions from blast crisis were treated with second transplants either as consolidation or after recurrence of blast crisis and appeared to achieve a longer survival compared with patients transplanted only once. Ph− metaphases were observed transiently after transplantation in a few patients. These studies showed the feasibility of using cryopreserved marrow or blood as a source of stem cells for autologous transplantation for CML.
These results led to studies evaluating the efficacy of autologous transplantation for patients before the onset of transformation. The Hammersmith group transplanted 21 chronic-phase CML patients between 1984 and 1992 with unmanipulated autologous peripheral blood mononuclear cells (PBMNC).39 The 5-year survival of the autografted patients (56%) was significantly higher compared with 636 age-matched controls treated with conventional chemotherapy (28%). Nine patients achieved some degree of Ph− hematopoiesis, including two patients who achieved complete Ph− hematopoiesis late (1 year and 3 years) after transplantation. Reiffers et al40 analyzed the results of 49 patients autografted for CML in chronic phase between 1989 and 1991 entered in the European Bone Marrow Transplant registry. Engraftment occurred in 45 patients and was significantly faster after PBMNC (30 patients) than marrow (19 patients) transplantation. Fifteen of 34 evaluable patients had a major cytogenetic response (>65% Ph−), 10 of whom had a complete cytogenetic response lasting 6 to 36 months after transplantation. The actuarial survival at 3 years was 81.5% ± 15%.
These studies (summarized in Table 1) suggest that autografting with unpurged autologous marrow or blood may extend survival for CML patients, particularly those transplanted in chronic phase, and may be an option for patients who cannot undergo allogeneic transplantation. The mechanism by which autografting with unpurged marrow could lead to Ph− hematopoiesis and could extend patient survival is not understood, although these effects may be related to a reduction in the size of the leukemic stem cell population by the transplant conditioning regimen. Alternatively, malignant CML progenitors could have a disadvantage in engraftment compared with their normal counterparts, which could favor engraftment with benign progenitors after transplantation.
Results of Autologous Transplantation for CML With or Without Ex Vivo Purging of Autografts
| Study . | Purging Method . | Stem Cell Source . | Patients Transplanted . | Cytogenetic Response . | Median Survival (range) . | |
|---|---|---|---|---|---|---|
| . | . | . | . | CR . | PR (%PH−) . | in Months . |
| Without purging | ||||||
| Blast crisis | ||||||
| Haines37 (Hammersmith) | None | PB | 51 | 0 | 3 (14-67) | 26 (0.5-35) |
| Reiffers38 (Bordeaux) | None | PB | 47 | 0 | 14 (>10) | 24 (4-49) |
| Chronic phase | ||||||
| Hoyle39 (Hammersmith) | None | PB | 21 | 2 | 9 (not defined) | 82 (9-105) |
| Reiffers40 (EBMTR) | None | PB + BM | 49 | 10 | 5 (>65) | — |
| 81% survival at 3 yr | ||||||
| With ex vivo purging | ||||||
| Carlo-Stella42 (Parma) | Mafosfamide | BM | 10* | 6 | 1 (75%) | — |
| McGlave43 (Minnesota) | IFN-γ | BM | 44 | 10 | 12 (15-95%) | — |
| CP 71% survival at 3 yr | ||||||
| AP 15% survival at 3 yr | ||||||
| Barnett44 (Vancouver) | Marrow culture | BM | 22† | 13 | 3 (>75%) | — |
| CP 81% survival at 5 yr | ||||||
| AP 50% survival at 4 yr | ||||||
| Study . | Purging Method . | Stem Cell Source . | Patients Transplanted . | Cytogenetic Response . | Median Survival (range) . | |
|---|---|---|---|---|---|---|
| . | . | . | . | CR . | PR (%PH−) . | in Months . |
| Without purging | ||||||
| Blast crisis | ||||||
| Haines37 (Hammersmith) | None | PB | 51 | 0 | 3 (14-67) | 26 (0.5-35) |
| Reiffers38 (Bordeaux) | None | PB | 47 | 0 | 14 (>10) | 24 (4-49) |
| Chronic phase | ||||||
| Hoyle39 (Hammersmith) | None | PB | 21 | 2 | 9 (not defined) | 82 (9-105) |
| Reiffers40 (EBMTR) | None | PB + BM | 49 | 10 | 5 (>65) | — |
| 81% survival at 3 yr | ||||||
| With ex vivo purging | ||||||
| Carlo-Stella42 (Parma) | Mafosfamide | BM | 10* | 6 | 1 (75%) | — |
| McGlave43 (Minnesota) | IFN-γ | BM | 44 | 10 | 12 (15-95%) | — |
| CP 71% survival at 3 yr | ||||||
| AP 15% survival at 3 yr | ||||||
| Barnett44 (Vancouver) | Marrow culture | BM | 22† | 13 | 3 (>75%) | — |
| CP 81% survival at 5 yr | ||||||
| AP 50% survival at 4 yr | ||||||
Abbreviations: CP, chronic phase; AP, advanced phase.
Ten of 25 patients achieving a significant response to ex vivo purging were transplanted.
Twenty-two of 87 patients achieving a significant response to ex vivo purging were transplanted.
Autologous Transplantation After Ex Vivo Purging of Malignant Progenitors
Several investigators reasoned that long-term cytogenetic remissions or cures after autologous transplantation therapy would require purging, or negative selection, of resting marrow with agents known to exert an antileukemia effect in CML. The following approaches to purging autologous marrow grafts have been evaluated in pilot clinical trials.
4-Hydroxyperoxycyclophosphamide (4-HC). Rizzoli's group showed that in vitro purging of resting marrow with cyclophosphamide derivatives such as 4-HC or mafosfamide exerted a selective killing effect on Ph+ progenitors and enriched Ph− stroma-adherent progenitors in a fraction of patients with CML.41 This group recently showed successful engraftment of autologous marrow cells treated ex vivo with mafosfamide in 10 patients (5 in chronic phase and 5 in advanced phase) selected by in vitro testing. Recovering marrow metaphases were 100% Ph− in 6 of 9 evaluable patients. Unfortunately, cytogenetic remissions were transient with a median duration of 6.5 months. Only one patient remains Ph−, whereas evolution to blast crisis has occurred in five patients during a relatively short median follow-up of 16 months.42
γ-IFN.The Minnesota group performed autologous transplantation with marrow cultured for 36 hours ex vivo in the presence of 1,000 U/mL γ-IFN in 22 chronic-phase and 22 advanced-phase CML patients.43 Regenerating marrow metaphases were 100% Ph− in 10 of 39 (26%) of evaluable cases and 11% to 95% Ph− in an additional 12 cases (32%). However, in all but 3 evaluable cases, the percentage of Ph− marrow metaphases had decreased to 10% or less within 12 months of transplantation. The projected 3-year survival for chronic-phase patients is 71% and for advanced-phase CML patients is 15%. Of note, 15 patients experienced delayed or partial engraftment requiring infusion of untreated, cryopreserved backup peripheral blood cells obtained before transplantation.
Ex vivo marrow culture.The Vancouver group made the exciting observation that growth of steady-state CML marrow progenitors in long-term liquid culture causes a selective loss of primitive Ph+ progenitors and enrichment of Ph− nonclonal, presumably benign committed and primitive progenitors.32 They followed-up on this observation by performing autologous transplantation using CML marrow cultivated in long-term liquid culture conditions for 10 days. Of interest, ex vivo screening studies showed sufficient yield of benign progenitors in only 36 to 87 patients (41%).44 Twenty-two of these 36 patients underwent transplantation with autologous ex vivo cultured marrow between November 1987 and March 1992, 16 of whom were in chronic phase and 6 with advanced disease. Thirteen of 16 evaluable patients became 100% Ph−, whereas 3 patients became partially Ph− (75% to 94%). However, in all but 1 case, Ph+ metaphases have reappeared in patients experiencing complete cytogenetic remission 4 to 36 months after transplantation. Thirteen of 16 chronic phase patients and 3 of 6 advanced-disease patients are alive from 1 to 5.7 years from transplant. Four of seven patients treated with low-dose IFN-α were returned to complete cytogenetic remission. Of concern, 5 patients experienced delayed or partial engraftment requiring infusion of untreated backup cells. This raises the concern that ex vivo manipulation may damage or deplete stem cells. Elimination of the malignant clone after ex vivo culture, attainable in only 40% of patients, may be an important factor in the induction of cytogenetic remissions posttransplantation. Brion et al45 autografted 2 patients with ex vivo cultured marrow that contained residual BCR/ABL+ cells after culture in both cases. Neither patient obtained cytogenetic remission posttransplantation.45
These results suggest that use of a graft purged ex vivo to enrich for Ph− progenitors, rather than an unpurged graft, may result in an increased frequency of cytogenetic remission posttransplantation. Consideration needs to be given to the possible contribution of patient selection to the favorable outcome of this group of patients. However, even in this selected group, cytogenetic remissions are of relatively short duration. These observations raise the possibility that purging of malignant progenitors may be incomplete. Furthermore, as expected from syngeneic and T-lymphocyte–depleted allogeneic studies, malignant clones may persist in the patients and recur quickly in the absence of ongoing immunologic or pharmacologic antileukemia activity. This indicates the need for both improved methods for purging of the autograft and better posttransplant antileukemia therapy to maintain remissions. It is significant that 20 of 75 patients autografted with marrow treated ex vivo experienced delayed or partial engraftment, indicating that the purging process may be associated with loss or damage of viable stem cells.
Autologous Transplantation After In Vivo Selection by Priming and Mobilization
The observation that treatment of chronic-phase CML with combination high-dose chemotherapy similar to that used in remission induction therapy of acute leukemia resulted in transient cytogenetic remissions in up to 50% of patients suggested that prior high-dose chemotherapy might provide a marrow or peripheral blood inoculum enriched for benign progenitors.26,27 In an early study, Korbling at al46 collected peripheral blood cells from a CML chronic-phase patient after chemotherapy at a time when the patient's marrow was 100% Ph− and used these for autografting when the patient's disease subsequently transformed to blast crisis. This patient had 100% Ph− hematopoiesis on recovery.46 Recently, Carella et al47 have pioneered the use of a similar approach to autotransplantation of CML patients based on the expectation that Ph− progenitors could be collected from the peripheral blood of CML patients early in recovery phase after intensive combination chemotherapy with idarubicin, cytarabine, and etoposide (ICE).47 Apheresis products of 12 of 24 chronic-phase (50%) and 5 of 22 advanced-phase (23%) patients were 100% Ph− on routine cytogenetics and were more than 50% Ph− in an additional 3 chronic-phase and 3 advanced-phase patients. Sixty-four percent of patients treated within the first year from diagnosis had 100% Ph− apheresis collections. Thirteen of 16 patients receiving a Ph− autologous inoculum after intensive chemoradiotherapy are engrafted and alive, with 5 patients remaining Ph− 5 to 29 months after transplantation. Hematopoiesis was polyclonal in all four female recipients tested by evaluation of X-chromosome inactivation patterns.48
The MD Anderson group collected peripheral blood and marrow progenitor in 21 CML patients recovering from combination chemotherapy and subsequently infused the CD34+ fraction after autologous transplant preparation with high-dose chemoradiotherapy.49 Inocula were completely Ph− in 3 of 21 cases and partially Ph− in an additional 7 cases. After transplantation, complete cytogenetic remission was observed in 5 of 10 chronic-phase patients, but in none of 11 advanced-phase patients. Of note, there was a direct correlation between the level of Ph− cells in the inoculum and the percentage of Ph− marrow cells recovered 17 to 55 weeks after autologous transplantation. These results suggest that the chances of achieving cytogenetic remissions after transplantation depend on the ability to generate a cytogenetic response with pretransplant treatment. It is not clear whether this effect is a result of the reduced leukemic burden resulting from effective purging of the autograft or whether a good response to conventional chemotherapy preselects those patients who are likely to respond well to the more intensive chemo-radiotherapy used in transplant preparative regimens.
At the University of Minnesota, 15 patients have undergone autologous transplantation with marrow collected after Cytoxan and granulocyte-macrophage colony-stimulating factor (GM-CSF ) treatment and 13 patients with peripheral blood progenitor cells collected after Mitoxantrone, Ara-C, and cyclophosphamide (MAC) combination chemotherapy and granulocyte colony-stimulating factor (G-CSF ) treatment. With both regimens, fewer Ph+ metaphases were observed in peripheral blood progenitor collections compared with marrow harvests performed at the time of recovery of counts. Seven of 13 patients receiving the combination chemotherapy regimen achieved a major cytogenetic response (>66% Ph− metaphases) in their peripheral blood progenitor collections, compared with 5 of 15 patients receiving Cytoxan alone. Only 1 of 15 patients had more than 66% Ph− cells in their marrow collections after Cytoxan treatment, compared with 2 of 7 patients in whom marrow was available for evaluation after combination chemotherapy. Combination chemotherapy was associated with increased toxicity compared with Cytoxan–GM-CSF, including 1 pretransplant death. In addition, in 3 patients, use of the combination chemotherapy regimen resulted in insufficient progenitor yield to allow transplantation. Five of 15 patients transplanted with marrow harvested after Cytoxan–GM-CSF therapy and 3 of 9 patients transplanted with peripheral blood progenitors harvested after combination chemotherapy achieved major cytogenetic responses.
Several other trials have explored the use of chemotherapy to induce Ph− hematopoiesis before harvesting marrow or peripheral blood for autografting,50-54 as shown in Table 2. The Swedish CML group,55 using a somewhat different approach, treated CML patients with sequential remission inducing therapies until a complete cytogenetic response was induced, after which marrow was harvested for autotransplantation. Ninety-seven newly diagnosed CML patients, without a donor for allogeneic transplant, were treated with Hydroxyurea and IFN-α for at least 6 months. Those who did not achieve a complete cytogenetic remission were treated with one to three courses of different intensive combination chemotherapies. Remissions were eventually achieved in the marrow of 23 of 97 patients. Fifteen patients were autografted in complete cytogenetic remission and 3 in partial remission. Nine of 16 evaluable patients are Ph− 1 to 32 months from transplantation. These results again suggest that intensive treatment reduces the Ph+ clone in CML and that autografting of these patients results in Ph− hematopoiesis after transplantation.
Results of Autologous Transplantation for CML After In Vivo Purging
| Study . | In Vivo Purging . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Chemotherapy . | Patients Studied . | Cytogenetic . | Autologous Transplantation . | ||||||
| . | Regimen . | . | Response . | Patients Transplanted . | Stem Cell Source . | Cytogenetic Response . | Survival (mo) . | . | ||
| . | . | . | CR . | PR (%Ph−) . | . | . | CR . | PR (%Ph−) . | . | . |
| Carella48 (Genoa) | ICE | 46 | 17 | 6 (>50%) | 16 | PB | 5 | NA | 15-29 | |
| Talpaz49 (MD Anderson) | DC/FMC/ICE | 21 | 3 | 7 (30-92%) | 21 | PB/BM | 5 | 5 (26-90%) | 1-21 | |
| McGlave (Minnesota) | Cy | 15 | 0 (BM) | 1 (BM) | 15 | BM | 2 | 3 | 12-26 | |
| 1 (PB) | 4 (PB) | |||||||||
| MACy | 13 | 1 (PB) | 6 (>66%) | 9 | PB | 0 | 3 | 2-12 | ||
| Tringali50 (Palermo) | Cy | 6 | 0 | 1 (NA) | 6 | PB/BM | 1 | 1 (>60%) | 14-26 | |
| O'Brien51 (Hammersmith) | ICE | 9 | NA | NA | 6 | PB | 0 | 3 (NA) | 0.6-11 | |
| Chalmers52 (Glasgow) | I, C | 25 | 11 | 2 (>50%) | 8 | PB | 1 | 1 (>50%) | NA | |
| Durrant53 (Australia) | ICE | 15 | 3 | 4 (>65%) | 5 | PB | 4 | NA | NA | |
| Sureda54 (Barcelona) | ICE | 3 | 1 | 1 (>33%) | 2 | PB | NA | NA | NA | |
| Simonsson55 (Sweden) | Hu/Ifn, DC MEA, AmA | 97 | 23 | NA | 18 | BM | 13 | 2 (>65%) | 13-32 | |
| Study . | In Vivo Purging . | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | Chemotherapy . | Patients Studied . | Cytogenetic . | Autologous Transplantation . | ||||||
| . | Regimen . | . | Response . | Patients Transplanted . | Stem Cell Source . | Cytogenetic Response . | Survival (mo) . | . | ||
| . | . | . | CR . | PR (%Ph−) . | . | . | CR . | PR (%Ph−) . | . | . |
| Carella48 (Genoa) | ICE | 46 | 17 | 6 (>50%) | 16 | PB | 5 | NA | 15-29 | |
| Talpaz49 (MD Anderson) | DC/FMC/ICE | 21 | 3 | 7 (30-92%) | 21 | PB/BM | 5 | 5 (26-90%) | 1-21 | |
| McGlave (Minnesota) | Cy | 15 | 0 (BM) | 1 (BM) | 15 | BM | 2 | 3 | 12-26 | |
| 1 (PB) | 4 (PB) | |||||||||
| MACy | 13 | 1 (PB) | 6 (>66%) | 9 | PB | 0 | 3 | 2-12 | ||
| Tringali50 (Palermo) | Cy | 6 | 0 | 1 (NA) | 6 | PB/BM | 1 | 1 (>60%) | 14-26 | |
| O'Brien51 (Hammersmith) | ICE | 9 | NA | NA | 6 | PB | 0 | 3 (NA) | 0.6-11 | |
| Chalmers52 (Glasgow) | I, C | 25 | 11 | 2 (>50%) | 8 | PB | 1 | 1 (>50%) | NA | |
| Durrant53 (Australia) | ICE | 15 | 3 | 4 (>65%) | 5 | PB | 4 | NA | NA | |
| Sureda54 (Barcelona) | ICE | 3 | 1 | 1 (>33%) | 2 | PB | NA | NA | NA | |
| Simonsson55 (Sweden) | Hu/Ifn, DC MEA, AmA | 97 | 23 | NA | 18 | BM | 13 | 2 (>65%) | 13-32 | |
Abbreviations: CP, chronic phase; AP, accelerated phase; BC, blast crisis; I, Idarubicin; C, ARA-C; E, Etposide; D, Daunorubicin; F, Fludarabine; M, Mitoxantrone; Hu, Hydroxyurea; Ifn, IFN-α; Am, Amsacrine; Ara-C; Cy, high-dose Cytoxan.
Although there is considerable variability in the results from different centers, it appears that in vivo selection may reduce the leukemic load in the autograft in selected patients, which in turn may be associated with superior achievement of Ph− hematopoiesis posttransplantation. However, BCR/ABL-expressing cells can usually be detected by using more sensitive techniques even in cytogenetic complete responders, indicating that these procedures do not eliminate all leukemic cells. Further investigation will determine whether strategies combining in vivo and ex vivo selection lead to further reduction in malignant cells and improve the incidence of cytogenetic remission and, of most importance, whether cytogenetic responses in autologous recipients are associated with improved survival.
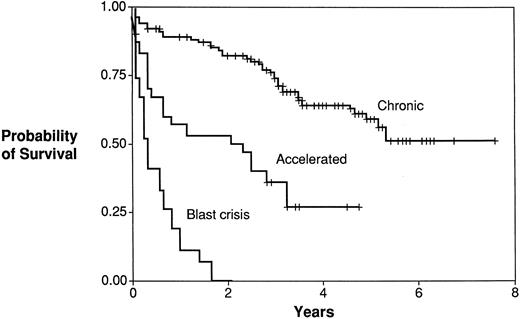
Effect of Autologous Transplantation on Survival
Single institution reports suggest that autologous transplant may be associated with prolonged survival, especially in chronic-phase patients, when compared with patients receiving conventional therapy. Recently, results of 200 consecutive autologous transplants performed with purged or unpurged marrow or blood at eight different transplant centers in Europe and North America between June 1984 and January 1992 were reported.56 This was the first multicenter report on autologous transplant for CML and included the largest number of autotransplanted CML patients studied to date. Of the 200 patients studied, 125 were alive at the end of the study (median follow-up of 42 months; range, 1 to 91 months). The median survival time of 142 patients with chronic-phase CML was not reached, was 35.9 months for 30 patients with accelerated phase (AP), and 4.1 months for 28 patients in blast crisis or second chronic phase after blast crisis. The survival probability for chronic-phase patients was 58%, suggesting that autotransplantation may result in improved survival compared with conventional chemotherapy. Aside from the disease phase at transplantation, no other patient characteristics predicted survival, including marrow or peripheral blood cell source or ex vivo purging methods. These results confirmed those from several smaller studies mentioned earlier, many of which were included in this analysis. An updated survival analysis of 198 patients (141 in chronic phase, 30 in accelerated phase, and 27 in blast crisis) from this series is presented with permission of the contributing investigators (Fig 1). The current analysis shows a 0.66 ± 0.09 probability of survival at 4 years in the chronic-phase group (Fig 1). Survival of chronic-phase patients is significantly better than that of patients in accelerated phase or in blast crisis. Mortality in the first year is 0.1 ± 0.06, which may be superior to that associated with either related donor or unrelated donor transplant and rivals that of newly diagnosed chronic-phase patients receiving initial therapy with IFN-α. Multivariate analysis suggests that younger recipient age (P = .04) and shorter interval from diagnosis to transplantation (P = .08) were independently associated with improved outcome. However, the majority of surviving autologous transplant recipients have evidence of cytogenetic or hematologic relapse, indicating that the procedure is not curative in this first generation of autologous transplant recipients and that their improved survival cannot be attributed to elimination of malignant progenitors after autografting. This suggests that the beneficial effect of autografting may be related to reduction rather than elimination of the leukemic cell load after myeloablative therapy, and again raises the possibility that reduction of the malignant clone in the patient before harvest by improved in vivo purging, more effective removal of residual malignant clones from the inoculum by improved ex vivo purging, and improved posttransplant antileukemia therapy may further improve results of autotransplantation. Although these results are encouraging, they need to be interpreted cautiously, because these trials were uncontrolled and patient selection may have influenced the results. In addition, the analysis included a heterogenous group of patients from eight transplant centers. Controlled clinical trials will be required to definitively demonstrate a survival benefit for autotransplantation compared with other therapeutic modalities for CML.
Autologous transplantation for CML. Survival by disease stage. Survival for patients receiving autologous transplantation. Chronio phase (Chronic; n = 141); accelerated phase (Accelerated; n = 30); blast crisis (BC; n = 27).
Autologous transplantation for CML. Survival by disease stage. Survival for patients receiving autologous transplantation. Chronio phase (Chronic; n = 141); accelerated phase (Accelerated; n = 30); blast crisis (BC; n = 27).
STRATEGIES TO IMPROVE OUTCOMES FOR AUTOLOGOUS TRANSPLANTATION IN CML
Reasons for Relapse After Autologous Transplantation
Cytogenetic remissions after autologous transplant are often incomplete and may not be durable. The above-mentioned results show that, although autografting may result in a transient Ph− state, Ph+ cells can usually be detected within the first year after transplantation. Relapse may be due either to persistence of leukemic cells in the autologous inoculum used to restore hematopoiesis or to persistence of leukemic cells in systemic tissue after intensive preparative therapy for the transplant. This issue may be resolved by retroviral marking of the autograft before transplantation, which would allow the contribution of transplanted malignant stem cells to posttransplant relapse to be assessed. After preclinical studies demonstrating that marrow from CML patients could be marked efficiently, Etkin et al57 used safety-modified retroviruses containing the NEO resistance gene to mark a portion of CD34+ marrow cells obtained from CML patients recovering from high-dose chemotherapy and subsequently used these cells for autografting. Using a PCR assay, the investigators were able to detect retrovirus in both normal and CML cells for at least 280 days after transplantation.58 These studies verified the feasibility of retroviral marking as a method for studying relapse in therapy of CML. The studies also showed unequivocally that sufficient malignant cells can remain in the inoculum to contribute to systemic relapse and indicate the need for improved methods for purging the autograft of malignant stem cells. The ability of autografting to achieve durable disease-free survival in future will depend on the development of improved methods for graft purging as well as improved antileukemia therapy that can be delivered to patients after transplantation. Several such approaches are being tested or are under consideration and will be discussed below.
Improved Methods for Purging the Graft
Antisense oligodeoxynucleotides directed against BCR/ABL.The BCR-ABL oncogene plays a critical role in malignant transformation in CML.4,5 It therefore appears to be a logical target for antileukemic therapies directed towards purging malignant cells from autografts. BCR/ABL-induced transformation is dependent on both its enhanced tyrosine kinase activity as well as its actin-binding properties.59,60 These properties allow the BCR/ABL protein to bind and phosphorylate a variety of signalling and cytoskeletal proteins that may lead to the transformed phenotype in CML, including abnormal circulation and unregulated proliferation of malignant progenitors. One attractive approach to the selection of a benign inoculum in CML is therefore the use of antisense oligonucleotides (AS-ODNs) targeting the BCR/ABL gene as purging agents. There is experimental evidence that AS-ODNs directed at the breakpoint junction of BCR-ABL mRNA inhibit expression of the abnormal p210 BCR-ABL fusion protein, inhibit proliferation of BCR-ABL containing cell lines and of blast crisis-CML hematopoietic progenitors, and prevent the development of tumor in experimental animals after the injection of blast crisis-CML marrow.61,62 Recently, de Fabritiis et al63 used marrow treated with BCR-ABL AS-ODNs to perform an autologous transplant in an advanced-phase CML patient. This patient was engrafted with marrow cells that were 10% Ph− at 9 months after transplantation.
Attempts at purging CML autografts with AS-ODNs directed at specific BCR-ABL mRNA breakpoints may not be effective for several reasons. Phosphodiester AS-ODN are easily inactivated by nuclease digestion, whereas phosphorothioate AS-ODNs may have reduced penetration into the target cells unless targeted using vehicles such as liposomes. The targeted sequence may be rendered inaccessible by steric configurations. Inhibition of BCR/ABL by AS-ODNs may result from nonspecific interactions with nontargeted mRNA or proteins.64 Some studies suggest that a fraction of malignant primitive progenitors may not express BCR-ABL mRNA and may therefore not be affected by AS-ODNs.65 Furthermore, specific inhibition of BCR-ABL after a brief exposure to AS-ODNs to BCR-ABL may not by itself eliminate chronic-phase CML progenitors. The efficacy of AS-ODN purging of CML marrow may be enhanced by combination with additional modalities such as cytotoxic agent purging.66 An alternative approach is retrovirus mediated insertion of a BCR-ABL AS-ODNs producing gene into marrow progenitor and stem cells, which would allow expression of the AS sequence in the cell of interest.67 In addition, extended exposure of CML progenitors to the antisense sequences could inhibit the BCR-ABL–mediated growth advantage of CML cells, enhance susceptibility to apoptosis, and possibly prevent transformation.
Ribozymes.Specific RNA sequences, termed ribozymes, have the ability to cleave other RNA molecules in a catalytic manner and have been adapted to create antisense molecules that specifically bind and cleave RNA molecules.68 Such ribozymes have been shown to inhibit BCR-ABL gene expression under various culture conditions.69 However, as observed with BCR/ABL AS-ODNs, reduction in BCR-ABL mRNA with single-unit ribozymes is variable and dependent on ribozyme activity and intracellular levels.68 More recently Leopold et al70 have developed multiunit (hammerhead) ribozymes that bind to BCR-ABL mRNA and cleave all three sites that lie in close proximity to the junction points that, when transfected into BCR-ABL transformed murine myeloblasts, dramatically reduced, but did not eradicate, BCR-ABL mRNA levels.
AS-ODNs directed against c-MYB.Calabretta et al71 have explored the use of AS-ODNs to the protooncogene c-MYB, rather than BCR-ABL, for the purging of CML marrow. In laboratory studies, they show that marrow treated with AS-ODNs to c-MYB and plated in progenitor cultures resulted in colonies that did not contain BCR-ABL mRNA assessed by reverse transcriptase-polymerase chain reaction (RT-PCR). This group recently showed partial cytogenetic remission in 2 CML patients receiving an autotransplant with CD34+ cells treated with c-MYB AS-ODNs.72
The antisense and ribozyme approaches, although attractive because of their potential specificity for malignant progenitors in CML, are fraught with problems. The ultimate success of these approaches will depend on whether malignant progenitor cells can be targeted in a specific manner over a period of time.
Tyrosine kinase inhibitors.The enhanced and promiscuous tyrosine kinase activity of the BCR-ABL oncogene plays a critical role in BCR-ABL–mediated transformation. BCR-ABL–containing cell lines and CML progenitors appear to be more susceptible to the tyrosine kinase inhibitor herbimycin A than their nontransformed counterparts.73 However, herbimycin A inhibits a variety of tyrosine kinases other than p210BCR-ABL and is therefore likely to exert effects on a variety of cellular functions unrelated to BCR-ABL–induced transformation. Recently agents with activity that is more specific for the p210BCR-ABL kinase have been described and are undergoing preclinical evaluation. A series of tyrosine kinase inhibitors structurally related to erbastatin, called tyrphostins, have been identified to have efficacy against the p210BCR-ABL tyrosine kinase and to inhibit the growth of CML cell lines.74 Druker et al75 have shown that cellular proliferation and tumor formation by BCR-ABL–expressing cells is specifically inhibited by a compound CGP 57148, selected for specificity against the ABL tyrosine kinase. This compound inhibits growth of 92% to 98% of CML colony-forming cells but does not inhibit normal colony formation. There are plans to test the efficacy of this compound in the treatment of CML in clinical trials. This approach may be useful for either ex vivo purging of CML marrow before transplantation or for posttransplantation antileukemia therapy.
Phenotypic selection of benign progenitors.Primitive progenitors with long-term culture-initiating capacity (LTC-IC) in the marrow of normal individuals are small, lymphoid-appearing cells that express CD34 (34+) and either do not express or express at low levels the HLA-DR receptor (DR−).76 Verfaillie et al34 showed that primitive progenitors in the CD34+HLA-DR− cell fraction obtained from CML marrow generate progeny that are nonmalignant by cytogenetics and RT-PCR. This was subsequently confirmed in a high proportion of patients in early chronic phase (<1 year after diagnosis).77 Other investigators have also shown that the CD34+DR− fraction of resting marrow is enriched for Ph− progenitors.35,36 The recent observations that this progenitor populations lacks the BCR/ABL rearrangement at the genomic level addresses the concern that primitive CML progenitors may not express BCR/ABL message and may therefore not be detected by RT-PCR. Of note, the 34+DR− population is markedly reduced and contaminated with malignant cells in late chronic-phase (>1 year from diagnosis) and advanced-phase patients.77 This observation suggests that the proportion of benign primitive progenitors available to reconstitute hematopoiesis after autologous transplantation dwindles with time or with development of advanced disease. Selection of CD34+DR− cells from the marrow of patients with early chronic-phase CML may thus offer a source of leukemia-free cells for autografting, although other approaches will be required for patients with more advanced disease. Recently, Verfaillie et al have performed large-scale selection of 34+DR− cells using a modified approach entailing CD34+ cell selection using imunoadsorbtion columns and high speed FACS sorting of CD34+HLA-DR− cells (DR− cells). Using this approach, they can obtain greater than 2 × 105/kg 34+DR− cells, which is expected to be adequate for hematopoietic reconstitution after autologous transplantation.77 A potential problem with this approach is that engraftment may be delayed as a result of depletion of committed progenitors that may contribute to early engraftment. Therefore, ex vivo expansion of selected primitive progenitors to expand the primitive and committed progenitor content and transplantation of a combination of unmanipulated and expanded cells is planned in an attempt to reduce the potential risk of delayed or failed engraftment.78
Immunologic approaches.Another approach to ex vivo purging of CML marrow currently being evaluated is the use of immune effector cells to selectively target leukemic cells. A graft-versus-leukemia effect has been well documented to prevent relapse in CML after allogeneic transplant. Verma et al79 reported that culture of CML marrow with recombinant interleukin-2 (rIL-2) for 1 to 2 weeks resulted in the generation of cells cytotoxic for the A375 melanoma cell line and K562 cells of CML origin. This technique resulted in the elimination of Ph+ cells from the marrow of 4 patients with CML. One type of lymphocytes that may contribute to this effect are natural killer cells. IL-2–activated NK cells (ANK) can be generated from the blood of patients with CML and are benign in origin.80 Their proliferation and function diminish with disease progression in CML, suggesting a role in tumor surveillance.81 Miller et al82 have developed techniques for large-scale ex vivo cultivation of activated NK cells that can be applied to immunotherapy protocols. Cervantes et al83 showed that, whereas autologous ANK did not suppress normal marrow progenitors, ANK from CML patients exhibited a dose-dependent suppression of marrow progenitors. This effect was dependent on cell-cell contact and involved the β-2 integrin receptor. Likewise, autologous T lymphocytes cultured from CML marrow were shown to suppress autologous hematopoietic progenitors, whereas T lymphocytes similarly generated from normal marrow failed to suppress autologous progenitors.84 Recently, Bocchia et al85 reported that a specific cytotoxic T-lymphocyte response could be generated in HLA-matched healthy donors against p210BCR-ABL breakpoint-derived peptides. These observations support the use of autologous ANK or T cells to purge CML marrow for autologous transplantation or to prevent relapse of CML after autologous transplantation (see below).
Measures based on abnormal stromal interactions of malignant CML progenitors.It has been observed that Ph+ CML hematopoietic progenitors, in contrast to normal Ph− progenitors, are deficient in their ability to adhere to the marrow stromal microenvironment.86,87 Interaction of the BCR-ABL oncogene product with cytoskeletal elements may account for the abnormal adhesive behavior of CML progenitors.88-90 Differences in adhesion to stroma and fibronectin between CML and normal marrow progenitors could therefore potentially be used to select for Ph− progenitors. In addition, Ph+ CML progenitors, unlike normal Ph− progenitors, do not respond to normal inhibitory signals and continue to proliferate even when in contact with stroma or fibronectin.91,92 Therefore, culture of CML marrow in the presence of these ligands followed by treatment with cell-cycle–specific chemotherapeutic agents may result in selective toxicity to Ph+ progenitors. Eaves et al93 reported that the chemokine macrophage inflammatory protein-1α (MIP-1α) inhibits the proliferation of primitive normal progenitors, but does not inhibit the proliferation of CML progenitors. Treatment of marrow cultures with MIP-1α may therefore accentuate differences in proliferation between CML and normal progenitors. This differential response after MIP-1α exposure could be exploited in therapeutic interventions with cell-cycle–specific chemotherapeutic agents directed against cycling malignant CML progenitors. Another possible approach being evaluated is based on the observation that malignant CML primitive progenitors have significantly reduced survival on stroma deficient in stem cell factor (SCF ) compared with normal progenitors. This results in the generation of an increased proportion of Ph− colonies when CML marrow is cultured on such stromal layers.94 It may be possible to purge CML marrow or PB progenitors by culture on SCF-deficient feeders, which could lead to selective depletion of Ph+ progenitors.
Antileukemia Therapy to Prevent Recurrence After Transplantation
Selection of a benign progenitor population from the autologous inoculum may not be sufficient to establish durable cytogenetic and hematologic remissions after autologous transplantation for CML. Relapse is well documented in chronic-phase CML patients receiving allogeneic transplants.13-15 Relapse is even more common if the inoculum is T-lymphocyte–depleted, if syngeneic cells are used, or if a related rather than unrelated donor is used,14 suggesting that an immunologically mediated graft-versus-leukemia effect may actively suppress expansion of persistent malignant clones.13,95 96 It seems likely that ongoing biologic, pharmacologic, or immunologic therapy will be required to sustain remissions in recipients of autologous transplantation even if the inoculum contains only benign progenitors.
IFN-α.The biological agent IFN-α may represent an antileukemia agent useful for prevention of relapse after autologous transplantation. IFN-α is active when used as a conventional therapy for CML and has been used to reverse cytogenetic relapse after allogeneic transplantation.97,98 Pigreux et al99 reported that one third of patients relapsing after allogeneic transplant achieved a complete cytogenetic remission after IFN-α therapy. Barnett et al44 also reported reversal of cytogenetic relapse in 4 of 7 autologous transplant recipients.
We have used IFN-α as prophylactic antileukemia therapy in 36 CML autologous transplant recipients. IFN-α therapy was initiated at the very low dose of 0.25 × 106 U when the absolute neutrophil count reached 1,000/μL in the immediate posttransplant period. In most cases, doses greater than 106 U/d were sufficient to maintain the white blood cell count between 2,500 and 10,000/μL, suggesting sensitivity to IFN-α in autologous transplant recipients that exceeded that of nontransplanted CML patients. In our experience, use of IFN-α at maximum tolerated doses after autologous transplant was associated with persistence of Ph− marrow metaphases in some patients achieving complete cytogenetic remissions, but rarely in patients not achieving complete remissions after autologous transplantation. It is not known whether the use of IFN-α contributed to persistence of the Ph− state in complete responders; however, this agent does not reverse cytogenetic relapse in the majority of patients, even when used aggressively early in the posttransplant course.
Immunologic approaches.Immunotherapy may represent a promising antileukemia therapy after autologous transplant therapy for CML. We and others have shown that both autologous, IL-2–stimulated NK cells and autologous T lymphocytes cultivated in the presence of CML are nonmalignant; exhibit cytotoxicity against a variety of target cell lines; can suppress autologous, malignant myeloid progenitor colonies in vitro; and, in the case of NK cells, can be cultivated ex vivo in large numbers. Clinical trials testing the antileukemia effects of IL-2 administered both as a purging agent and exogenously in the posttransplant interval are underway100,101 as well as trials assessing the efficacy of Linomide, an agent thought to stimulate NK cells.102 Additional studies designed to test the use of autologous lymphocyte populations administered with IL-2 are contemplated.
Induction of drug resistance.Introduction of drug resistance genes into selected Ph− cells obtained from marrow or peripheral blood of CML patients may be useful as an antileukemia therapy approach in autologous transplant recipients.103 After transplantation, systemic chemotherapy could then be used to suppress nontransduced, malignant clones that survived initial transplant therapy. In one recently described strategy, vectors containing a drug resistance gene linked to a BCR-ABL antisense gene would be transduced into selected Ph− marrow or blood cells to avoid inadvertantly conferring a drug-resistant state on residual malignant stem cells.67
THE ROLE OF AUTOLOGOUS TRANSPLANTATION IN THE EARLY TREATMENT OF CML
The role of autologous transplantation in the early therapy of CML is not yet understood. Analysis of a first generation of autologous transplants performed largely in previously treated, older patients ineligible for allogeneic transplant or not responding to IFN-α therapy suggests that this approach has antileukemia activity associated with prolongation of survival and acceptable peritransplant mortality. However, because these studies were uncontrolled and patient selection could have contributed to the longer than expected survival, controlled trials are needed to confirm the encouraging results of these pilot studies and definitively determine whether autologous transplantation does in fact prolong survival. One important multicenter trial is underway in the United Kingdom testing the role of autologous transplantation as early salvage therapy in CML patients failing to achieve cytogenetic responses with IFN-α. This trial will provide valuable information concerning the role of autologous transplantation as second-line therapy in CML and should be supported. However, the trial does not test the potential of autologous transplantation as primary therapy for newly presenting chronio-phase CML patients. Recently, reported studies suggest that chemotherapy priming and autologous transplantation of mobilized stem cells can provide complete remissions in a majority of newly presenting chronic-phase CML patients. If primary therapy with autologous transplantation is indeed shown to be efficacious and safe on further evaluation, clinical trials comparing autologous transplantation with other approaches such as the use of IFN-α alone or in combination with chemotherapeutic agents are warranted. In addition, single-arm studies aimed at improving the efficacy of benign stem cell selection and posttransplant antileukemia therapy will be useful. Such studies will determine if autologous transplantation can move the field of CML therapy beyond the considerable strides made over the last decade by implementation of therapy with IFN-α.
Address reprint requests to Philip B. McGlave, MD, Department of Medicine, Box 480 UMHC, 420 Delaware St SE, Minneapolis, MN 55455.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal