In this issue of Blood, Allen and colleagues provide insights into the mechanisms of resistance to MDM2 and BCL-2 inhibitors such as idasanutlin and venetoclax in acute myeloid leukemia (AML), particularly in monocytic subtypes (FAB M4/M5).1 The investigators describe a positive feedback loop of interleukin-1 (IL-1)–tumor necrosis factor-α (TNF-α)–nuclear factor κB (NF-κB) pathway members regulated by CEBPB, which promotes monocytic differentiation and confers drug resistance.
AML is a heterogeneous disease characterized by a block in myeloid differentiation leading to rapid expansion of leukemic blasts and bone marrow failure.2 The addition of the BCL-2 inhibitor venetoclax to hypomethylating agents (HMAs) leads to a significant improvement in response and survival compared with HMAs alone for older unfit adults with newly diagnosed AML resulting in the approval of venetoclax by the US Food and Drug Administration (FDA) and European Medicines Agency (EMA) in this setting. Despite the promising improvement in outcome, resistant disease and relapses remain frequent.3 Altered BCL-2 family member expression, especially of MCL-1, plays a key role in venetoclax resistance.4,5 The TP53 regulator MDM2 is expressed in the blasts of around 50% of patients with AML. Targeting MDM2 for the treatment of AML with small molecule inhibitors including idasanutlin6 is thus attractive, but responses are mixed.
Recent studies suggest that therapy resistance correlates with distinct AML subsets and that the differentiation status of leukemia cells affects sensitivity to BCL-2 inhibition.7,8 Monocytic subsets have been found to be reliant on MCL-1 to mediate survival and thus are resistant to venetoclax.7 Based on this rationale, the findings of Allen and colleagues are of special interest: the investigators uncovered drug resistance mechanisms to a broad range of MDM2 inhibitors and BH3 mimetics particularly in monocytic leukemia. The underlying resistance mechanism is a positive feedback loop in which CEBPB in monocytic AML induces inflammatory cytokines, which further induce monocytic differentiation while concomitantly increasing CEBPB, thus inducing therapy resistance to MDM2 and BCL-2 inhibitors.
One strength of the present study lies in its comprehensive and integrated approach in deciphering drug resistance mechanisms in AML for MDM2 inhibitors and also venetoclax. Based on an integrated analysis of functional genomic data from the Beat AML cohort, Allen and colleagues observed that, similar to venetoclax, idasanutlin was ineffective in monocytic leukemia. The researchers then compared differentially expressed transcription factors (TFs) in monocytic vs primitive AML. Thirty-two of the differentially expressed TFs showed a significant correlation with resistance to venetoclax and idasanutlin. Five were further investigated as they had a known impact on myeloid differentiation. In subsequent validation experiments, out of the 5 TFs, only CEBPB overexpression induced resistance to both venetoclax and idasanutlin. Conversely, CRISPR-mediated knockout of CEBPB sensitized cells to several of BH3 mimetics and MDM2 inhibitors. Of note, FAB M4/M5 AML cells displayed higher nuclear levels of CEBPB than M0/M1 AML cells.
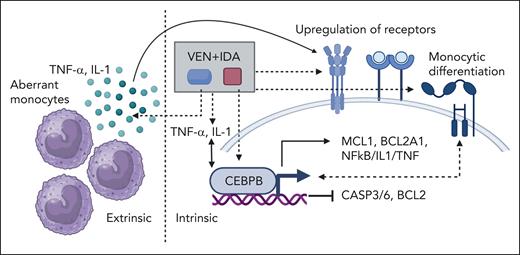
In an elegant way, Allen et al investigated both intrinsic and extrinsic resistance factors in a complex interplay orchestrated by CEBPB. CEBPB overexpression increased expression of BCL2A1, MCL-1, IL-1–TNF-α–NF-κB pathway genes, CD14, and CD11b, whereas expression of BCL-2 and downstream targets of TP53 was decreased (see figure). Furthermore, CEBPB overexpression downregulated CASP3 and upregulated IL-1β, several cytokine receptors, and MCL-1 at the protein level. Moreover, the investigators provide evidence for a coexistence and potential interplay between CEBPB-mediated intrinsic and IL-1- and TNF-α-mediated extrinsic drug resistance. Abnormal CD14+ monocytes in M4/M5 leukemia secreted IL-1 and TNF-α, which in turn conferred extrinsic drug resistance to M4/M5 blasts expressing high levels of IL-1 and TNF-α receptors. Nonetheless, it remains unclear if the described CD14+ monocytes could belong to the leukemia bulk and if IL-1β and TNF-α then further enhanced CEBPB expression in M4/M5 AML.
Interplay between intrinsic and extrinsic resistance mechanisms in monocytic AML. Idasanutlin (IDA) and venetoclax (VEN) treatment enhances CEBPB-mediated intrinsic and IL-1- and TNF-α-mediated extrinsic drug resistance in monocytic AML. CEBPB leads to an increased expression of BCL2A1, MCL-1, IL-1–TNF–NF-κB pathway genes and monocytic differentiation, whereas expression of BCL-2, CASP3, and CASP6 decreased. Abnormal monocytes in M4/M5 leukemia secrete IL-1 and TNF-α, which in turn confers extrinsic drug resistance to M4/M5 blasts expressing high levels of IL-1 and TNF-α receptors. Through an autocrine activation loop, IL-1β induces its own expression and expression of other prosurvival cytokines. IL-1 and TNF-α induce an increase in CEBPB in M4/M5 AML. Figure created with Biorender.com.
Interplay between intrinsic and extrinsic resistance mechanisms in monocytic AML. Idasanutlin (IDA) and venetoclax (VEN) treatment enhances CEBPB-mediated intrinsic and IL-1- and TNF-α-mediated extrinsic drug resistance in monocytic AML. CEBPB leads to an increased expression of BCL2A1, MCL-1, IL-1–TNF–NF-κB pathway genes and monocytic differentiation, whereas expression of BCL-2, CASP3, and CASP6 decreased. Abnormal monocytes in M4/M5 leukemia secrete IL-1 and TNF-α, which in turn confers extrinsic drug resistance to M4/M5 blasts expressing high levels of IL-1 and TNF-α receptors. Through an autocrine activation loop, IL-1β induces its own expression and expression of other prosurvival cytokines. IL-1 and TNF-α induce an increase in CEBPB in M4/M5 AML. Figure created with Biorender.com.
To precisely dissect how IL-1 and TNF-α mediate MDM2 inhibitor resistance, Allen et al performed immunoblotting on idasanutlin-treated AML samples in the presence or absence of these factors and performed RNA sequencing on idasanutlin-treated samples from patients with AML, with or without addition of IL-1β. Intriguingly, the authors discovered an autocrine activation loop of multiple prosurvival signaling pathways. IL-1β induced its own expression and the expression of other prosurvival cytokines. IL-1 and TNF-α induced a marked increase in CEBPB only in M4/M5 AML, which was accompanied by variable upregulation of MDM2 and MCL-1 and downregulation of CASP6 and BCL-2. After dissecting the autocrine activation loop, the authors observed that idasanutlin and venetoclax treatment can further enhance CEBPB-mediated intrinsic and IL1- and TNF-α-mediated extrinsic drug resistance in monocytic AML.
The positive feedback loop with increased inflammation might not only be relevant for idasanutlin and venetoclax but also have broader implications. For example, it was recently shown that high inflammatory cytokines might be responsible for the lack of efficacy of chimeric antigen receptor T cells in AML.9 Accordingly, strategies to suppress inflammatory cytokines or TFs might improve AML therapy. Allen et al provide evidence that monocytic drug resistance could be targeted. Inhibitors of MAPK14, IRAK4, IL-1, or TNF-α improved efficacy of idasanutlin and venetoclax in M4/M5 monocytic leukemias. The anti-interleukin-1 receptor antagonist anakinra, one of the proposed inhibitors, is FDA and EMA approved with a known toxicity profile. Thus, in principle, clinical trials can be envisioned where suppression of inflammatory signaling is combined with the currently less effective therapy approaches. However, adding immunosuppressive drugs such as anakinra could substantially increase toxicity of therapies. Although the role of inflammation in poor outcome is recognized in many diseases, the increased risk associated with standard immunosuppressive strategies might offset the mechanistic benefit. One example is cardiovascular disease in which IL-1β targeting lowers cardiovascular events but increases fatal infections.10 Accordingly, further studies are needed to identify suitable drugs and the best therapeutic approach.
In summary, the study by Allen and colleagues highlights the complex interplay between intrinsic and extrinsic resistance mechanisms in monocytic AML, centered around the CEBPB–IL-1β–TNF-α feedback loop. Their findings suggest a synergistic interaction between CEBPB-mediated intrinsic and IL-1- and TNF-α-mediated extrinsic drug resistance mechanisms. Targeting inflammatory cytokines might reach center stage in AML to overcome drug resistance in AML.
Conflict-of-interest disclosure: The authors declare no competing financial interests.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal