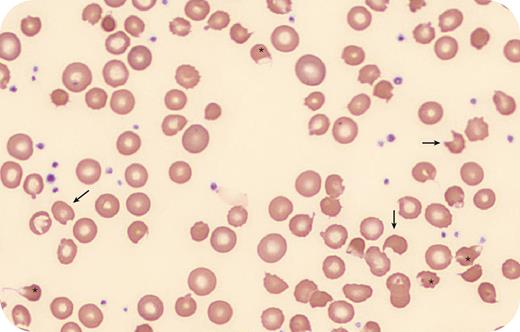
A 47-year-old woman with interstitial cystitis had abrupt onset of hemolytic anemia with nadir hemoglobin 6.1 g/dL. Labs showed reticulocytes 7%, total bilirubin elevated at 1.5 mg/dL, direct bilirubin 0.5 mg/dL, lactate dehydrogenase 385 units/L, and haptoglobin undetectable, all of which were normal previously. A direct antiglobulin test was negative. Blood smear (100× lens objective, Wright-Giemsa stain) revealed blister cells (asterisks) and bite cells (arrows). She had several recent courses of phenazopyridine for pain from interstitial cystitis, including immediately preceding the discovery of hemolysis. Hemolysis abated with the holding of phenazopyridine. Glucose-6-phosphate dehydrogenase (G6PD) testing is inaccurate acutely due to temporary normalization at the time of hemolysis, but it was normal when sent 4 months later.
Phenazopyridine is known to cause oxidative stress and should be avoided in patients with G6PD deficiency. More rarely, it can cause oxidative hemolysis without G6PD deficiency, as seen in this patient. This occurs in part through the generation of methemoglobinemia, while the presence of blister cells on the blood smear indicates direct oxidative membrane damage as well. Phenazopyridine-induced hemolysis should be suspected with an exposure and characteristic blood smear, highlighting the importance of both an accurate history and smear review.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal