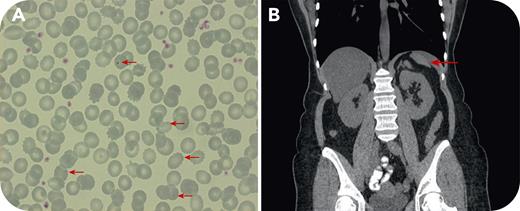
An asymptomatic 55-year-old woman presented with thrombocytosis discovered 2 years earlier. Laboratory testing revealed the following: hemoglobin 13.1 g/dL, red blood cell count 5.04 × 109/L, hematocrit 41.8%, mean corpuscular volume 83 fL, mean corpuscular hemoglobin concentration 31.3 g/dL, leukocytes 10.87 × 109/L (neutrophils 43%, lymphocytes 45%, monocytes 5%, eosinophils 4%), and platelets 513 × 109/L. Serum ferritin levels were low at 8 ng/mL. Physical examination was unremarkable. Serum ferritin normalized with adequate iron replacement, but blood counts, including platelets, remained unchanged. Peripheral blood smear examination confirmed mild thrombocytosis but also revealed Howell-Jolly bodies and target cells (panel A; original magnification ×100, arrows). Testing for JAK2-V617F, CALR9, and c-MPL mutations was negative. There was no history of splenectomy or sickle cell syndrome. In abdominal ultrasonography, the spleen “was not clearly visible.” An abdominal computed tomography (CT) scan revealed an elongated left liver lobe extending to the left hypochondrium and markedly decreased spleen dimensions (panel B, arrow). An extensive retrospective search in the patient’s medical record revealed that splenic hypoplasia was also detected, but not reported, in another CT performed 6 years earlier. There was no history of severe infections. Causes of acquired splenic atrophy/hypoplasia, including splenic vessel thrombosis, coeliac disease, sarcoidosis, and autoimmune disorders, were excluded.
Congenital or acquired splenic hypoplasia without prior splenectomy should be considered as an extremely rare “spot” diagnosis in the differential diagnosis of reactive thrombocytosis, by seeking Howell-Jolly bodies in the patient’s peripheral blood smear.
For additional images, visit the ASH Image Bank, a reference and teaching tool that is continually updated with new atlas and case study images. For more information, visit https://imagebank.hematology.org.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal