Background: Autologous stem cell transplantation (ASCT) is the major transplantation therapy for patients with lymphoma and MM, and the success of auto-HSCT depends on the mobilization efficiency of peripheral blood HSC. In clinical practice, CD34 + cell count in peripheral blood is often monitored to predict the collection effect and determine the collection time. However, prediction of poor mobilizers is still difficult .
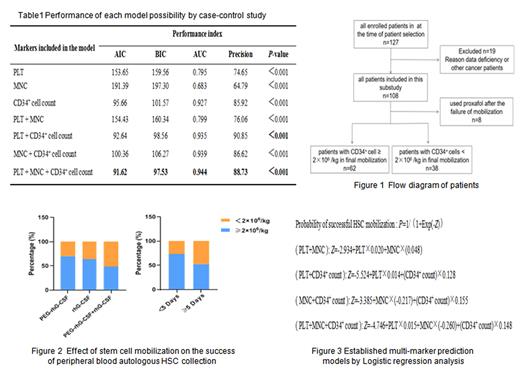
Methods: We retrospectively analyzed 108 patients with lymphoma and multiple myeloma(MM) at Chongqing University Cancer Hospital who underwent autologous hematopoietic stem cell (HSC) collection between January 2021 to August 2022. There are two groups: collection success group and collection failure group. Compared the differences of clinical characteristics and impact of peripheral blood related detection indexes before autologous HSC collection. Logistic regression analysis was used to establish a prediction model for the successful collection by multi-marker and further evaluated multi-marker prediction models.
Results : There was no significant difference in sex, disease type, disease stage, age, disease status before mobilization, mobilization drugs and chemotherapy courses between the successful collection group and the failed collection group ( P> 0.05). The proportion of patients with mobilization days less than 5 days was higher in the successful collection group ( P< 0.05). The platelet count (PLT), mononuclear cell count (MNC) and absolute CD34 + cell count in the successful collection group were significantly higher than those in the failure group. The sensitivity, specificity and area under the curve (AUC) of combining three indexes were 80.9%, 95.9% and 0.944, respectively. Applied the Logistic regression models to the absolute count of PLT, MNC and CD34 + cells to construct the multi-marker prediction algorithms. The 3-marker model of PLT+MNC+CD34 + cells had the lowest AIC, BIC and high AUC. A prediction model was established based on the absolute count of PLT, MNC and CD34 + cells.
Conclusion :Patients with less than 5 days of mobilization have a higher success rate of collection. PLT, MNC and CD34 + cell counts before collection can reflect HSC mobilization in patients with lymphoma and MM, and the combination of the three can improve the accuracy of prediction of collection effect.The predictive model based on the absolute number of PLT, MNC and CD34 + cells have good predictive value. Our study suggests that multi-markers are important diagnostic tools for predicting successful collection.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal