Background: Acute Myeloid Leukemia (AML) is a heterogenous Hematopoietic stem cell disorder and standard therapy being intensive chemotherapy (IC) followed by consolidation with either high dose Cytarabine or Allogeneic Hematopoietic stem cell transplantation in intermediate and high-risk patients. Though the outcome in younger & fit patients with IC in terms of CR rates and survivability are reasonable, however patients above 60 years may not benefit owing to increasing frailty, co-morbidities, adverse disease risk factors, chemo resistance and toxicities. Newer approaches with Novel/Targeted agents are being incorporated in treatment strategies in order to acheive better results and long-term survival. We report outcome of AML patients treated on standard chemotherapy at our institution.
Methods: Total 208 Acute Myeloid Leukemia (AML) patients were treated at our institution between January 2017 and December 2022 and analyzed after institutional review board (IRB) approval. Data was collected from institutional data base and summarized by medians and Range for continuous variables, numbers and percentages for categorical variables & Survival estimates were obtained by Kaplan-Meier method.
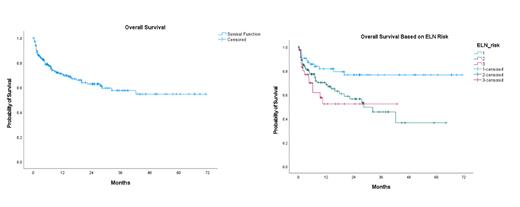
Results: Median age of our cohort was 46.5 years (range,17-90), Male patients were 57% (n-118) and 43% (n-90) were Female. Seventy-five (36%) were locals and 133 (64%) of other nationalities. Median WBC 11.5 x10^9/L (range 0.60-381); Hemoglobin 83 g/L (range 27-103), Platelets 53x10^9/L (range 2-791), Median Bone marrow blast were 50% and median LDH 357 U/L. Normal cytogenetics was present in 54.4% (n-111); 19%(n-39) were Core binding Factor (CBF), 3.5% trisomy 8 and 3.5% were complex cytogenetics. Major molecular mutations included FLT3-ITD (21%), NPM1 (18.3%), DNMT3A (11%), IDH1&2 (7%), TET2(5%), TP53(3.5%) and ASXL1(3%). As per European Leukemia Net (ELN 2017) risk stratification, Intermediate risk were 50% (n-104), Favorable 30% (n-63) and Adverse 20% (n-41). Total of 164 (79%) patients received intensive chemotherapy, 13(7%) Azacytidine and Venetoclax, 16(8%) low intensity and 12(6%) best supportive care (BSC). Intensive chemotherapy included Anthracyclines +Cytarabine and FLAG/FLAG-Ida (Fludarabine, Idarubicin, Cytarabine and G-CSF). Total of 136(65%) of patients achieved Complete Remission (CR/Cri) after 1 or 2 inductions. Major adverse events during induction were grade 4 cytopenia's and pneumonias. There were 26(13.6%) deaths during induction. Majority of patients received consolidation therapy with high dose cytarabine 1-3 g/M2 twice a day for 3 days for two to 3 cycles and 28(14%) underwent Allogeneic stem cell Transplantation. At a median follow up of 9.1 months, the 2 year and 5-year overall survival (OS) were 65% and 57% in whole cohort. ELN Favorable Risk group had a better survivability at 2 years (80%). Two-year OS in Patients above 60 and less than 60 years were 37% and 75% respectively.
Conclusion: Intensive chemotherapy resulted in significant survival improvement in AML and has been standard of care for more than 3 decades. However significant advances in understanding the biology, risk categorization and development of newer novel therapies has led to alter the treatment strategy with better outcome. Our study underlines the fact that we need to incorporate the newer therapies in treatment plan to achieve these goals.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal