Introduction: Serum Protein Electrophoresis (SPEP) is a frequently ordered diagnostic test when there is suspicion of plasma cell dyscrasia, based on clinical or laboratory abnormalities. This study describes the demographic characteristics of US Veterans who underwent SPEP testing, evaluates the distribution of clinical and laboratory abnormalities, and their influence on SPEP test ordering by Veteran Health Administration (VHA) providers.
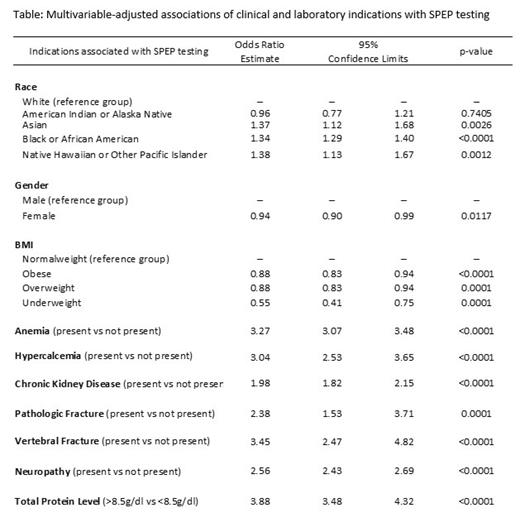
Methods: The study employed a retrospective cohort design utilizing national data from the VHA. We included Veterans aged 50-65 years who had a total protein test performed at any time. Veterans who were dually enrolled in VHA and Medicare were excluded because of the unavailability of laboratory data in Medicare. An ordered SPEP was defined by Current Procedural Terminology codes of 84165 or 83883. Multivariable logistic regression was performed to examine the association of SPEP testing with clinical and laboratory indications, including, chronic kidney disease, anemia, pathologic fractures, vertebral fracture, neuropathy, total protein level, hypercalcemia, and body mass index, as well as sociodemographic factors, including, race, sex, socioeconomic status, and geographic location. The clinical and laboratory indications were selected based on literature review and clinicians' input. For patients who received SPEP testing, data on these indications within one year before their initial SPEP test were used. For patients who did not receive SPEP testing, these indications were collected within one year of their most recent total protein test.
Result: Between 1999 and 2022, 294,640 Veterans were identified, with 17,035 (5.78%) undergoing SPEP testing. Veterans who had SPEP testing were mostly male (77%), White (51%), and frequently obese (BMI>30 kg/m 2) (42%). In addition, 17% of these Veterans who had SPEP testing had neuropathy, 15% had anemia, 11% had chronic kidney disease, 4% had a total protein level > 8.5gm/dL, and 2% had hypercalcemia. Only 0.5% had pathologic fractures and 0.5% had vertebral fractures. VHA providers ordered SPEP tests more often in African American Veterans than White Veterans (OR 1.34, 95% CI 1.29-1.39), and less often in underweight (BMI < 18.5 kg/m 2) Veterans compared to normal-weight (18.5-24.9 kg/m 2) Veterans (OR 0.55, 95% CI 0.40-0.74). SPEP testing was more likely in Veterans having total protein level >8.5gm/dL (OR 3.87, 95% CI 3.47-4.32), vertebral fracture (OR 3.44, 95% CI 2.47-4.81), anemia (OR 3.26, 95% CI 3.06-3.48), hypercalcemia (OR 3.04, 95% CI 2.53-3.65), neuropathy (OR 2.55, 95% CI 2.43-2.69), pathologic fracture OR 2.38, 95% CI 2.38-1.52), and chronic kidney disease (OR 1.97, 95% CI 1.81-2.14) compared to Veterans without the respective indication.
Conclusions: VHA providers were likely to order a SPEP for protein level >8.5gm/dL, vertebral fracture, anemia, hypercalcemia, neuropathy, pathologic fracture, and chronic kidney disease. Obesity and demographic factors such as African American race were also associated with SPEP testing. Further research is needed to evaluate the combined influence of these factors on SPEP testing, as well as factors that lead clinicians to order multiple SPEP tests prior to the diagnosis of plasma cell dyscrasias.
Disclosures
Sanfilippo:Quinn Johnston: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal