Background: Immune thrombotic thrombocytopenic purpura (iTTP) is a hematologic emergency characterized by severe acquired deficiency in the von Willebrand factor-cleaving metalloprotease ADAMTS13 and thrombotic microangiopathy, resulting in end organ damage and death if untreated. Plasma exchange (PLEX) is vital to the management of iTTP and has dramatically improved survival in this disorder since the 1980s. Guidelines recommend initiation of PLEX within 4-8 hours of presentation. However, despite the importance of prompt medical intervention, determinants of the total interval between symptom onset and initiation of PLEX (S2P) and time from presentation at the pheresis center to PLEX (door to PLEX, D2P) remain unclear. Further, the impact of S2P and D2P on clinical outcomes in iTTP have not been evaluated.
Objective: Identify factors that predict S2P and D2P in patients with iTTP and assess the clinical impacts of S2P and D2P.
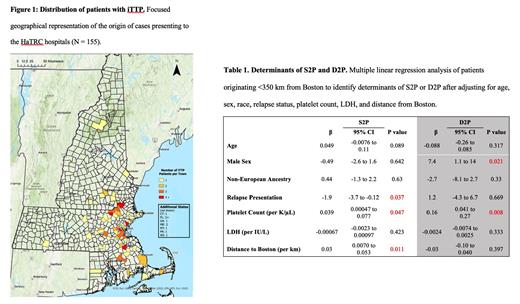
Methods: We retrospectively evaluated cases in the Harvard TMA Research Collaborative (HaTRC), a curated single-center rare disease registry containing all consecutive iTTP cases seen between 2004 and 2022 at the three main Harvard teaching hospitals. We restricted our modeling analyses to patients who resided <350 km from downtown Boston. S2P was defined as time from patient-reported symptom onset until initiation of PLEX. D2P was defined as the time from the first complete blood count specimen drawn at a HaTRC hospital until the initiation of PLEX. Determinants of S2P and D2P were identified using multiple linear regression modeling of covariates derived from the HaTRC registry. The impacts of S2P and D2P on mortality and the composite of mortality and need for ICU admission were assessed using multiple logistic regression modeling.
Results: A total of 155 unique patients comprising 243 separate iTTP episodes were recorded ( Figure 1). Analyses were limited to patients who resided <350 km from downtown Boston (n = 147 patients, 227 cases). The median (IQR) age was 40 (29-53) years. The cohort was 76% female, 63% of European ancestry, and 45% of episodes were relapse presentations. The median (IQR) S2P for the entire cohort was 4.3 (1.8-7.5) days, and the median D2P was 8.4 (5.0-16.0) hours. Excluding relapse presentations, crude S2P correlated with distance from Boston (Spearman r = 0.216, 95% CI: 0.029-0.389, p=0.02). After adjusting for age, sex, race, and LDH, we found that higher platelet count at presentation (β=0.039, 95% CI: 0.00047 to 0.077, p=0.047) and increased distance from Boston (β=0.030, 95% CI: 0.007 to 0.053, p=0.011) were associated with longer S2P, while patents with relapse presentations experienced a shorter S2P (β=-1.9, 95% CI: -3.7 to -0.12, p=0.037) ( Table 1). By contrast, increased D2P was significantly associated with male sex (β=7.43, 95% CI: 1.128 to 13.73, p=0.021) and higher platelet count (β=0.16, 95% CI: 0.41 to 0.27, p=0.008) but not with distance from Boston or relapse status. Longer S2P or D2P times were not associated with increased mortality, hospital LOS, or the composite of mortality and need for ICU admission; however, there was a non-significant trend towards increased LOS with relapse presentations (p=0.06) and longer D2P times (p=0.09).
Conclusions: Our data suggest that iTTP patients who live farther from the hospital where they ultimately receive PLEX, those with higher platelet counts at presentation, and those presenting for the first time with iTTP experience a longer time to initiation of care. After hospital presentation, the determinants of a longer time to PLEX initiation shift to male sex and higher platelet count, both of which may be associated with lower clinical suspicion for iTTP and delayed diagnosis. These findings should be externally validated in an independent dataset.
Disclosures
Bendapudi:Alexion Pharmaceuticals: Consultancy; Takeda Pharmaceuticals: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal