Healthcare inequities are often attributed to large-scale structural barriers for access to medical care or patient-medical staff interactions. However, the role of the electronic medical record (EMR) in perpetuating hidden biases has been poorly characterized. This passive form of sharing implicit biases with unknown readers may have profound ripple effects asynchronous in place and time from the note writer. This study aims to illustrate racial imbalances in ad hominem patient characterizations as documented by medical staff, regardless of role, in a large metro healthcare system.
The use of certain potentially stigmatizing language in emergency department (ED) and inpatient notes for hematology/oncology patients was investigated. Retrospective chart review of four hospitals within a university network in a major metro area between 1/1/2019 - 6/30/2021 was undertaken. Patients ≥22 years old were included with two primary hypotheses in mind: 1) Negative terms are used more frequently for underrepresented minorities, and 2) words with shock value (i.e. curse words) are used more often than more general descriptors of these terms (e.g. “cursing” or “profanity”).
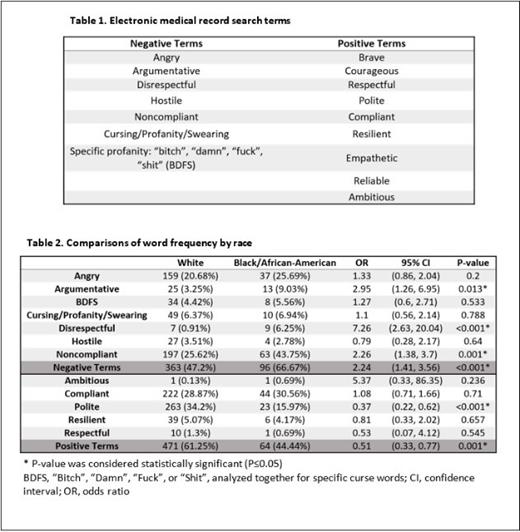
Nine positive and twelve negative terms were evaluated, based on the authors' observations of their use in the EMR in past encounters (Table 1). Some were personal descriptors in which the ED or inpatient note writer would be less likely than outpatient providers to have a full sense of outpatient care or social determinants of health (e.g. compliant). Others were behavioral descriptions (e.g. hostile) or words with minimal medical relevance (e.g. curse words). If multiple notes in an encounter included the same word(s), the encounter was only analyzed once for each word to avoid word count inflation, though re-occurrences for the same patient in subsequent encounters were counted. Authors' manual data review using natural language processing software confirmed appropriate use of terms. Generalized estimating equations were used for race-based comparisons to account for same-patient clustered encounters. Odds ratios (OR) and 95% confidence intervals (CI) were calculated for self-reported demographic comparisons with White as the reference category. P≤0.05 was considered significant.
A total of 1,059 encounters for 889 hematology/oncology patients were analyzed. Mean age was 61 years (standard deviation 16.7) and 49.4% were female. White race was reported for 80.2% of patients (72% system-wide prevalence during same timeframe) and Black for 11.4% (15.2% system-wide); all others were ≤4% so only White/Black comparisons were included. Positive terms were more prevalent than negative ones (n=535 vs 459). However, negative terms were found more often for Black individuals (OR 2.24, CI 1.41 - 3.56, P<0.001), while the positive terms were less frequently documented in Black patients relative to White patients (OR 0.51, CI 0.33 - 0.77, P=0.001), and neither category was concordant with the overall patient racial demographics. Other significant racial differences existed for the terms “Argumentative”, “Disrespectful”, “Noncompliant”, and “Polite”, all discrepancies which favored White patients (Table 2). Specific curse words were documented nearly as often as “cursing”, “swearing”, or “profanity”, but no racial differences were observed. Some words in the initial search (“Brave”, “Courageous”, “Empathetic”, and “Ambitious”) were not found in hematology/oncology notes in this timeframe.
EMR documentation in hospital-based hematology/oncology care demonstrated evidence of racial discrepancies in language that may carry stigma, positively or negatively. Importantly, many of these terms have questionable, if any, medical relevance. The use of stigmatizing terminology in the EMR may reflect implicit biases that extend past the direct patient encounter, passively and subconsciously prejudicing future care from other staff members. Time-saving heuristics and documentation shortcuts like copy-forwarding may further ossify healthcare inequities. This phenomenon is undoubtedly not limited to this hospital system or the hematology/oncology field, but quantitative real-world evidence has been scant. Improved awareness of stigmatizing language in documentation may be one step towards mitigating this contributor to unequal care for hematology/oncology providers and their patients.
Disclosures
Bendel:Merck: Research Funding. Boucher:CSL Behring: Research Funding; Takeda: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal