Introduction: Increasing number of older patients are undergoing allogeneic stem cell transplants (alloSCT) for acute leukemia and MDS. We and others have previously reported alloSCT outcomes of older patients. However, majority of these studies included very few patients older than 70 years. In addition, the information on the influence of donor source on alloSCT outcomes among older patients is limited. In this study, we aim to answer two questions: Is there any difference in long-term survival between patients 60-69 years and those older than 70 years? Does donor source affect alloSCT outcomes of these two groups?
Methods: We retrospectively evaluated alloSCT outcomes of 467 patients older than 60 years with acute leukemia (AML and ALL) and MDS. We compared outcomes between two groups: 60-69 years of age and those older than 70 years. The primary objective was to evaluate long-term overall survival (OS). Multivariable analyses included age, comorbidity index, KPS, disease risk index, donor relation, CMV serotype, conditioning regimen, GVD prophylaxis, and thymoglobulin use as variables.
Results: Between January 2010 and December 2022, 335 patients with 60-69 years and 132 older than 70 years underwent alloSCT. Median age of the population was 66 years (range, 60-80); 6% (N=30) were African American and 22% (N=101) were of ethnic minority; 53% (N=249) had AML, 39% (N=184) had MDS, and 7% (N=34) had ALL; donor was matched unrelated in 60% (N=279), matched related and haploidentical in 14% each, and mismatched unrelated in 12% (N=55). Source of allograft was peripheral blood stem cells in all patients. Higher proportion of patients older than 70 years received matched unrelated donor compared to those with 60-69 years (69% vs 56%; p=0.004). Reduced intensity conditioning (RIC) regimen was frequently used among patients older than 70 years compared to 60-69 years (97% vs 79%, p<0.001). Neutrophil and platelet engraftment time was similar in both groups. Graft failure rate was higher for patients older than 70 years compared to 60-69 years (5.3% vs. 1.2%; p=0.014). The cumulative incidence of grade 3-4 acute GVHD was similar (13.5% vs 7.6%, p=0.2), while severe chronic GVHD was higher for the 60-69 group compared to the 70+ group (20.1% vs 10%, p=0.009).
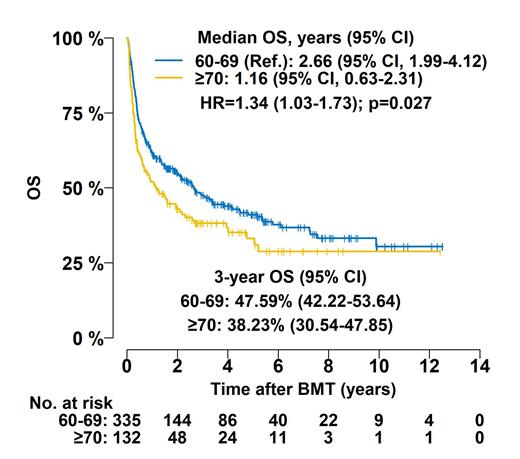
Median follow up for OS was 4.46 years. At 3 years, OS was 48% for the 60-69 group and 38.23% for the 70+ group (HR 1.34, p=0.02); RFS was 44% for the 60-69 group and 36.3% for the 70+ group (HR 1.32, p=0.02); relapse rate was 26.2% for the 60-69 group and 27.2% for the 70+ group (HR 1.13, p=0.51); and NRM was 30% for the 60-69 group and 37% for the 70+ group (sHR 1.26, p=0.19). In the multivariable analyses, patients older than 70 years experienced poor survival (HR 1.41, p=0.01) and relapse-free survival (RFS) (HR 1.4, p=0.01), and numerically higher non-relapse mortality (NRM) (sHR 1.38, p=0.08) compared to those with 60-69 years. Compared to haploidentical donors, matched related (sHR 0.39, p=0.04) and unrelated donors (sHR 0.28, p=0.005) were associated with lower NRM, while a trend for increased relapse rate and NRM was associated with the use of thymoglobulin and post-transplant cyclophosphamide (PTCy) containing GVHD prophylaxis, respectively.
Conclusion: Our results indicate that although rates of acute GVHD and relapse were similar between both groups, patients older than 70 had worse OS and RFS compared to patients between 60-69. The NRM was numerically higher in patients older than 70 years of age. Haploidentical donor was associated with increased NRM, most likely secondary to toxicity associated with PTCy based GVHD prophylaxis. Detailed analysis of toxicity will be presented at the conference.
Disclosures
Modi:BeiGene: Speakers Bureau; Karyopharm, ADC Therapeutics, Genentech: Research Funding; Morphosys, Seagen, AstraZeneca (spouse), Genentech (spouse): Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal