Background
Langerhans cell histiocytosis (LCH) is a rare, heterogeneous histiocytic neoplasm. There are few studies focusing on LCH in adults with single system multifocal disease (SS-m).
Methods
This retrospective study enrolled 43 LCH in adults with SS-m from 422 adult LCH at Peking Union Medical College Hospital between January 2001 and May 2023. We analyzed the clinical characteristics, genomic profiling, treatment approaches, and outcomes of LCH in adults with SS-m.
Results
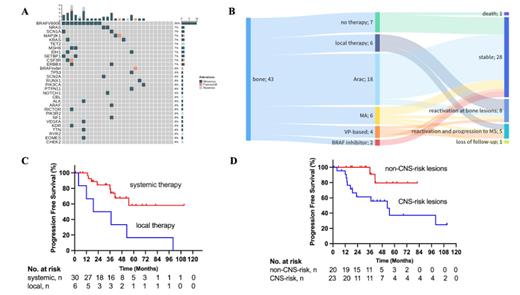
Of all patients, the median age at diagnosis was 34 years (range, 21-65 years) with a male-to-female ratio of 1.7:1. The median duration from symptom onset to diagnosis was three months (range, 1-130 months). All patients had bone involvement. Bone pain (90.7%) was the most common symptom, followed by tumor formation in a localized area of bone (11.6%), toothache (4.6%), and hearing impairment (2.3%). The median number of bone lesions was three (range, 2-11). The most common bone invasion sites were the ribs (51.2%), followed by the pelvis (46.5%), spine (39.5%), skull (30.2%), and maxillofacial bones (30.2%). Twenty-three patients (53.5%) had central nerve system (CNS)-risk lesions involvement. Of the 28 patients with next-generation sequencing, the median number of gene mutations was two (range, 1-9), and the overall percentage of MAPK pathway mutations was 64.3%. BRAF V600E, MAP2K1, and BRAF indelmutations were detected in 35.7%, 7.2%, and 3.6% of patients, respectively (Figure1 A). The initial treatments divided into local therapy (n = 6) and systemic therapy (n = 30). Systemic therapy included 18 received cytarabine monotherapy, six received methotrexate combined with cytarabine, four received vindesine and prednisone-based regimens, and two who had CNS-risk lesions involvement received BRAF inhibitors (Figure1 B). After a median follow-up of 43 months (range, 1-218 months), one patient died due to disease progression, and 13 patients had reactivation, including 8 with bone lesions, and 5 progressed to multisystem LCH. The 3-year overall survival and progression-free survival (PFS) rates were 97.4%, and 75.4%, respectively. Univariate analysis showed that systemic therapy (36.3 months vs. 28.0 months, P= 0.013) and non-CNS-risk lesions involvement (36.0 months vs. 23.0 months, P = 0.016) were associated with a better PFS (Figure1 C, D).
Conclusions
The overall percentage of MAPK pathway mutations in adult LCH with SS-m was low. Systemic therapy should be considerd as first-line treatment for LCH in adults with SS-m, and CNS-risk lesions involvement predicted a poor prognosis.
Figure Captions
Figure1. A. Next-generation sequencing of lesion tissues of LCH in adults with single-system multifocal disease (SS-m); B. Treatment and outcomes of adult patients with SS-m; C. Progression-free survival (PFS) according to first-line treatment; D. PFS according to CNS-risk lesions involvement at baseline
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal