Abstract
Background: Invasive fungal disease (IFD) represents an important complication in patients with hematologic malignancies as they are associated with substantial morbidity and treatment-related mortality. However, incidence and outcome of IFD vary substantially in the literature (e.g., prevalence of IFD in children with acute lymphoblastic leukemia is reported to range between 4 to 30%), owing to the differences in cancer type, treatment protocol, geographic location, race, and socioeconomic status of the patient population. As a "majority-minority” state located within a tropical climate, Hawai'i provides a unique opportunity for further examination of these differences among underrepresented racial groups. This may inform whether current standard of care practices are appropriate or may need to differ for patients in this region of the United States. We aim to describe the incidence and outcome of IFD in children and young adults with hematologic malignancies at Kapiolani Medical Center for Women and Children (KMCWC) over the past 6 years.
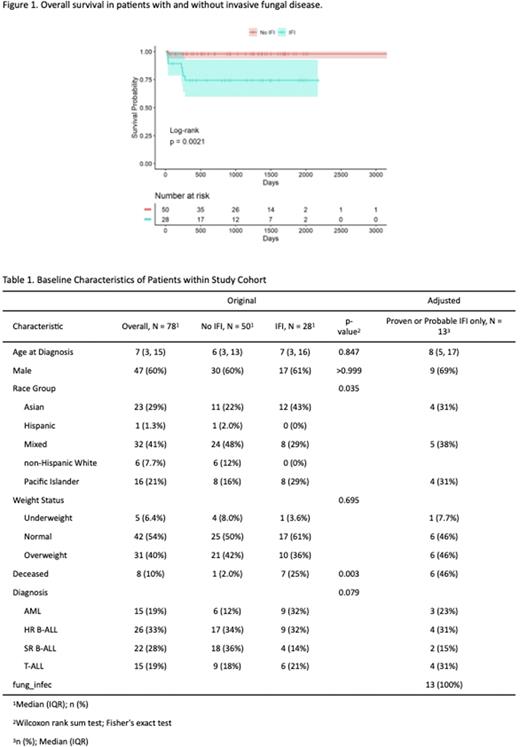
Methods: Retrospective data were collected on 78 consecutive patients (age range 0-29 years) with newly diagnosed acute leukemias from January 1st, 2016 to December 31st, 2021 at KMCWC. Each IFD episode was classified as proven, probable, or possible as defined by the 2020 European Organization for Research and Treatment of Cancer (EORTC) guideline. Demographic and clinical information were summarized by descriptive statistics, both at IFD episode and patient levels. A Kaplan Meier curve was generated showing the time to first IFD episode from diagnosis. One-year incidence of IFD was calculated. Survival analysis was conducted comparing those who had an IFD episode and those who did not, and the log-rank test was used to assess the difference between the two groups.
Results: Of the 78 patients, 28 (35.9%) patients developed an IFD, accounting for 39 distinct episodes. Of these episodes, 12 (23.3%) were classified as proven, 6 (16.6%) as probable, and 21 (53.8%) as possible. Amongst the different races/ethnicities, incidence of IFD amongst Asian patients is 12 of 23 (52%), 8 of 16 (50%) in Pacific Islander patients, 8 of 32 (25%) in multi-racial patients, 0 of 1 (0%) in Hispanic patients, and 0 of 6 (0%) in non-Hispanic White patients. Incidence rates of IFD were 13 of 48 (27.1%) in B-ALL, 6 of 15 (40%) in T-ALL, 9 of 15 (60%) in AML. IFD occurred most frequently during the Induction phase of treatment (19 of 39, 49%). Of the 18 episodes with proven and probable disease, 3 of 18 (16.7%) were infected with Candida albicans, 6 of 18 (33.3%) with non-albican Candida spp., 8 of 18 (44.4%) with Aspergillus, and 1 of 18 (5.6%) with Fusarium solani spp. Of these 18 episodes, 6 of 18 (33.3%) were receiving anti-fungal prophylaxis at the time of IFD diagnosis; 3 of 6 (50%) with fluconazole, and 3 of 6 (50%) with caspofungin. The one-year incidence of invasive fungal infection among patients with newly diagnosed acute leukemia was 36.6%. Among patients with and without an IFD episode, the one-year survival probabilities were 74.4% and 97.9%, respectively (p-value=0.002) (Figure 1). Patient and disease characteristics are summarized in Table 1.
Conclusion: A high incidence of IFD is seen within our unique patient cohort and geographic location relative to rates reported in other cohorts with similar risk. The majority of pathogens were Candida spp. followed by Aspergillus spp., and only one-third of the patients that sustained an IFD were receiving antifungal prophylaxis prior to IFD onset. These findings provide an important foundation for future studies to better understand the genetic, environmental, and socioeconomic factors underlying these differences, and suggest that current clinical practice guidelines for systemic antifungal prophylaxis may need to be tailored to specific subpopulations and locations, rather than the current "one size fits all” approach.
Disclosures
Fisher:Astellas Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees; Pfizer: Other: performing a research study for piperacillin-tazobactam use in children. Not relevant to this study; Merck: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal