Abstract
Background: Patients with chronic lymphocytic leukemia (CLL) have a higher risk of developing second primary malignancies (SPMs; Kumar et al. Blood Cancer J, 2019), but this risk has not been assessed with more recent population-based data that consider the growing use of targeted oral agents.
Aims: To assess the timing, frequency, incidence and types of SPMs in treated and untreated patients with CLL, using population-based data from the United States.
Methods: This was a retrospective cohort study of patients with newly diagnosed CLL from January 2010 to December 2016 using the Surveillance, Epidemiology, and End Results (SEER)-Medicare database, which links a nationally representative cancer registry with Medicare claims data. Patients were assessed for ≥36 months through to end of continuous Medicare Parts A/B/D or health maintenance organization enrollment, death, or end of follow-up (December 2019). Patients were defined as untreated or treated based on procedure/drug codes for CLL treatments up to 36 months post-diagnosis. SPMs were defined as having an inpatient diagnosis code for a hematologic (excluding CLL) or solid tumor malignancy, or two non-specific outpatient codes at least 30 days apart. Demographic and clinical characteristics were assessed for 12 months prior to CLL diagnosis. SPM rates were provided as frequency distributions overall and by treatment status. SPM timing was also assessed. In this analysis, non-Hodgkin lymphoma (NHL) was excluded as a SPM due to the potential diagnostic overlap between CLL and NHL; the results including NHL as a SPM will be presented as a sensitivity analysis.
Results: Of 3053 newly diagnosed patients with CLL, 620 (20.3%) were treated and 2433 (79.7%) were untreated within 36 months of diagnosis. At diagnosis, the median age was 75 years, 50.0% of patients were male, 92.5% were white, 30.7% had advanced stage disease, and 40.7% had ≥2 comorbidities. Median follow-up was 67.7 months. Among those treated within 36 months of diagnosis, the median time to first treatment was 13.9 months; 44.8% of patients received an anti-CD20 + chemotherapy, 22.1% received anti-CD20 monotherapy, 19.7% received targeted oral monotherapy/combination therapy with a BCL-2 inhibitor (fewer than 11 patients) or a Bruton's Tyrosine Kinase inhibitor, and 13.4% received other treatments. Among those untreated within 36 months of diagnosis, 12.5% eventually received their first CLL treatment at a median of 51 months since diagnosis.
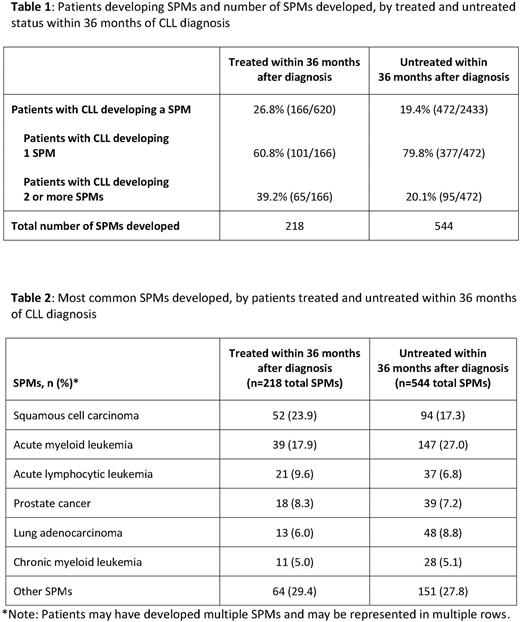
Overall, 20.9% (638/3053) of patients developed a SPM, with a greater proportion observed in the treated versus untreated cohort (26.8% [166/620] vs. 19.4% [472/2433]; p<0.001). Among the 166 treated patients who developed SPMs, 39.2% developed >1 SPM, with a total of 218 SPMs across treated patients. Among the 472 untreated patients with SPMs, 20.1% developed >1 SPM for a total of 544 SPMs across all untreated patients (Table 1). Of the 638 patients who developed a SPM, 29.3% had developed a SPM by 12 months post-diagnosis, and 64.9% had developed a SPM by 36 months post-diagnosis. The most common SPMs for both cohorts were squamous cell carcinoma, acute myeloid leukemia, acute lymphocytic leukemia, prostate cancer, lung adenocarcinoma, and chronic myeloid leukemia (Table 2). Among the 166 treated patients who developed a SPM, a greater proportion developed their first SPM after treatment initiation (69.3% [115/166]) compared with 30.7% [51/166] who developed SPMs prior to treatment initiation (p<0.001). SPM development across groups was 30.6% (85/278) for anti-CD20 + chemotherapy, 21.9% (30/137) for anti-CD20 monotherapy, and 20.5% (25/122) for targeted oral monotherapy/combination therapy (pairwise tests were not significant at 0.05). For all three groups, development of the first SPM occurred more frequently after treatment initiation than before.
Conclusions: In this recent retrospective analysis, more than 20% of patients diagnosed with CLL had a SPM. SPMs were more frequent in patients who received CLL therapy within 36 months of diagnosis versus those who did not. Among those who developed a SPM, most patients developed it within 36 months post-diagnosis. The current analysis did not show that any of the anti-CLL treatments were more likely to contribute to the risk of SPMs post-therapy. Additional analyses evaluating the impact of therapy type and baseline disease and patient characteristics on incidence of SPM are ongoing.
Disclosures
Ravelo:Roche: Current equity holder in private company, Current holder of stock options in a privately-held company; Genentech / Roche: Current Employment. Ng:Genentech: Current Employment; F. Hoffman-La Roche Ltd.: Current equity holder in publicly-traded company. Wang:Genentech, Inc: Current Employment; Roche: Current equity holder in private company. Eakle:Genentech / Roche: Current Employment; Roche: Current equity holder in private company, Current holder of stock options in a privately-held company. Biondo:Roche: Current equity holder in private company, Current holder of stock options in a privately-held company; Genentech Inc: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal